Methods for endovascular treatment of bifurcation lesions of coronary arteries: commonly used techniques
REVIEW
Methods for endovascular treatment of bifurcation lesions of coronary arteries: commonly used techniques
Article Summary
- DOI: 10.24969/hvt.2020.218
- Page(s): 139-148
- Cardiac Surgery
- Published: 03/10/2020
- Received: 23/09/2020
- Accepted: 02/10/2020
- Views: 9927
- Downloads: 7687
- Keywords: bifurcation lesions (BL), percutaneous coronary interventions (PCI), provisional T-stenting, “kissing” dilatation, "culotte" technique, T-stenting, “Double Kissing crush (DK)", bifurcation stents
Address for Correspondence: Zairbek A. Syrgaev, Scientific Research Institute of Heart Surgery and Organ Transplantation, Ministry of Health of the Kyrgyz Republic 720040, Togolok Moldo St 3/1, Bishkek, Kyrgyzstan
Email: z_syrgaev@mail.ru, Mobile: +996 999299986
Authors
Scientific Research Institute of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan
Scientific Research Institute of Heart Surgery and Transplantation of Organs of the Ministry of Health of the Kyrgyz Republic, Bishkek, Kyrgyzstan
Abstract
In everyday operating practice, the endovascular surgeon often encounters complex lesions of the coronary arteries, in particular bifurcation lesions. Percutaneous coronary interventions (PCI) is technically difficult in these cases and has always been associated with lower procedural success rates and poorer clinical outcomes than non-bifurcation lesions. The introduction of antiproliferative coated stents into clinical practice significantly improved the results and gave impetus to the development of various treatment techniques. The provisional technique for implanting one stent into the main branch remains the approach of choice for most bifurcation lesions. The choice of the most effective technique for each individual bifurcation is important. The use of a two-stent technique is an acceptable approach for some forms of bifurcation lesions. However, a large amount of metal in the artery wall, as a rule, remains uncovered in the lumen of the vessel during this tactic, which is especially true for the risk of stent thrombosis. New techniques and special bifurcation stents may possibly overcome some limitations of the using two stents and revolutionize the management of PCI of bifurcation lesions of the coronary arteries in the future.
Scientific Research Institute of Heart Surgery and Organ Transplantation, Ministry of Health of the Kyrgyz Republic, Bishkek, Kyrgyzstan
Abstract
In everyday operating practice, the endovascular surgeon often encounters complex lesions of the coronary arteries, in particular bifurcation lesions. Percutaneous coronary interventions (PCI) is technically difficult in these cases and has always been associated with lower procedural success rates and poorer clinical outcomes than non-bifurcation lesions. The introduction of antiproliferative coated stents into clinical practice significantly improved the results and gave impetus to the development of various treatment techniques. The provisional technique for implanting one stent into the main branch remains the approach of choice for most bifurcation lesions. The choice of the most effective technique for each individual bifurcation is important. The use of a two-stent technique is an acceptable approach for some forms of bifurcation lesions. However, a large amount of metal in the artery wall, as a rule, remains uncovered in the lumen of the vessel during this tactic, which is especially true for the risk of stent thrombosis. New techniques and special bifurcation stents may possibly overcome some limitations of the using two stents and revolutionize the management of PCI of bifurcation lesions of the coronary arteries in the future.
Key words: bifurcation lesions (BL), percutaneous coronary interventions (PCI), provisional T-stenting, “kissing” dilatation, "culotte" technique, T-stenting, “Double Kissing crush (DK)``, bifurcation stents
Search for evidence: databases PUBMED, GOOGLE SCHOLAR, ELIBRARY
Introduction
Bifurcation lesions (BL) - are coronary artery lesions, affecting the main artery, dividing into two vessels, where the longest and largest distal branch should be accepted as the “main branch” (MB), and the second, the shorter and smaller, is the side branch (SB).
To date, their endovascular treatment remains one of the most serious problems in performing percutaneous coronary intervention (PCI). These procedures constitute 15-20% of the total number of interventions (1- 4). The frequency of BL is explained by the fact that atheromatous plaques form at the sites of the greatest tension of the vessel wall, in the areas of turbulent blood flow, which are observed mainly at the level of bifurcations, in the region of carina, at the ostium of the side vessel (5). Therefore, according to the ARTS II study, their frequency among all types of stenosis of the coronary arteries was 22% (6).
The beginning of endovascular treatment of patients with BL of coronary arteries should be considered 1977, when Gruentzig proposed the idea of simultaneously inflating two balloon catheters in the main and side bifurcation branches. And later, in 1989, Meier first used this technique in clinical practice (7). However, it was not widespread due to the high frequency of unsatisfactory results of the intervention. The risk of SB occlusion during balloon dilatation of the main artery was 14–33%, and the deterioration of blood flow in SB occurred in 27–41% of cases (8).
The unsatisfactory results of balloon angioplasty of bifurcations in most cases are due to the displacement of plaque elements at the ostium of the SB (snow-plough effect), which makes it necessary to repeat balloon inflations in the main and side branches. This, in turn, can lead to the development of extensive dissections of arterial intima, as well as thrombosis and subsequent myocardial infarction (MI) (9).
In a large randomized clinical trial TULIPE, in which provisional T-stenting was used, it was found that the angle of bifurcation is the most common predictor of side branch occlusion, along with its diameter and well-head lesion nature (10). In contrast, the DK CRUSH-1 study, where patients underwent classical or double- kissing crush stenting, showed that the bifurcation angle does not affect the incidence of restenosis and major cardiac complications in the long-term period after the intervention (11).
Another unfavorable factor in the treatment of bifurcation stenosis is the eccentricity of the lesion. The uneven distribution of effort during balloon inflating due to the eccentricity of the lesion causes overstretching of the free part of the vessel wall, making it difficult to form tears in the intima of the plaque itself, and leads to elastic collapse of the artery. This is one of the main causes of residual stenosis after balloon angioplasty (7, 12).
Classification of bifurcation lesions of the coronary arteries
The complexity of BL treatment further contributed to the development of various classifications. Nowadays, in the literature, several classifications of BL of coronary arteries are known. The most common division of all bifurcations is into true and non-true. True bifurcation lesions are narrowing of the coronary arteries, in which, according to coronary angiography, the lumen of the MB and the ostium of the SB are narrowed by more than 50% of the diameter. Significant lesions of only one branch are called non-true lesions (13). The authors noted that 4–16% of all PCI in the coronary arteries is performed for true BL. Of these, most cases are bifurcations of the left anterior descending and diagonal arteries (74–87%).
According to other authors, the frequency of interventions for BL is 14-18% (14, 15). This includes interventions for not only true, but also non-true BL, since in most cases they become true during the execution of the interventions. The reason for this is the axial redistribution of the plaque substance at the ostium of the SB during stenting of the main artery.
There are also so-called “hidden” bifurcations. These include, firstly, lesions that were not diagnosed due to the inadequacy of the selected projection during coronary angiography, and secondly, lesions that are difficult to diagnose due to poor contrast or lack of contrast of the bifurcation area during acute or chronic total occlusion of the coronary artery (16).
In the era of bare metal stents, four classifications (Sunburn, Lefevre, Safian, Duke) of bifurcation lesions of the coronary arteries have been proposed (17- 20). However, they are not widely used in clinical practice due to various shortcomings and inconvenience in use.
Modern, more complex is the classification of Movahed (20). It uses a 5-letter code and numbers. It provides information on the proximal segment of MB, the significance of narrowing of the ostium of the SB, the angle of divergence of branches, and the nature of the lesion on bifurcation. However, despite the fact that some authors noted the advantage of the Movahed classification in that it can be used to easily choose the tactics of PCI, this classification is also not widely used due to the difficulty in use.
The most convenient and widely applicable at present is the classification proposed by Medina et al. in 2006. In contrast to the previous ones, this classification characterizes each type of bifurcation with a combination of three digits, which reflects, respectively, the state of MB proximal and distal to the origin of the SB, as well as the state of the ostium of the SB. Each of these segments is evaluated according to the binary system: if there is no angiographically significant stenosis in the segment, its condition is characterized as “0”, if there is angiographically significant stenosis in the segment, its status is displayed by the number “1”. In this classification, as in other modern classifications of BL of coronary arteries, 7 anatomical types are distinguished. This classification is easy to use and easy to remember, therefore it is approved by the European Bifurcation Club. However, in this systematization there is no information on the angle between the main and side branches (21).
Treatment of bifurcation lesions
In order to systematize many methods and their varieties, the MADS classification was developed, which was approved and proposed for use in clinical practice by the European Bifurcation Club. The classification is presented in the form of a table, the column distribution is determined by the first stent implanted in which segment of the bifurcation: M (main proximal first) - the first stent is implanted in the proximal segment of the MB, A (main across side first) - the first stent is implanted through the ostium of the SB, D (distal first) - the first stent is implanted in the distal segment of the MB, S (side branch first ) - SB is first stented. The distribution of the rows of the table depends on other details of the correction: the total number of implanted stents, the features of their location, etc. The above classification can be replenished with new techniques, information about which periodically appears in the literature (22).
In modern practice, the following techniques for correcting coronary artery bifurcations are most often and best used.
Provisional T-stenting” This is a method of single-stent BL treatment strategy with the ability to implant a second stent if necessary. Currently, most interventional cardiologists adhere to the provisional T-stenting strategy for BL, which is shown in Figure 1. This method was distinguished from other methods by its relatively quickness, ease, use of one stent and finally the best clinical results, both immediate and long-term.
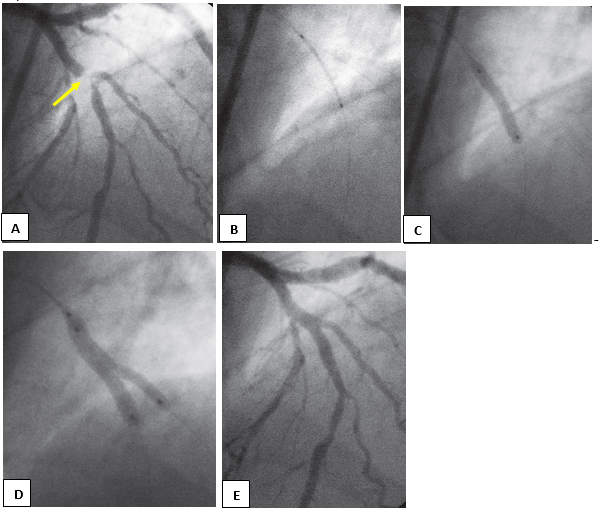
Figure 1. Provisional T-stenting of the bifurcation of the left anterior descending (LAD) and diagonal (DA) arteries: A - initial coronary angiogram: lesions of LAD and DA, type 1.1.1 (arrow); B - stent positioning in LAD; C - stent implantation in the main branch (LAD) with the wire inserted into the side branch (DA); D - final bifurcation formation using the “kissing balloons” technique; E - angiographic result of correction.
Using this approach, it will be limited to the implantation of one stent into the MB in 80-90% of cases (23). However, another multicenter registry reports that the need for a second stent after kissing dilation was 34% (22).
Coronary wires in the distal sections of the main and side branches: Routine carrying out two wires has several advantages:
• Can improve SB patency after stenting the main branch.
• Serves as a marker of the ostium of the SB in case of occlusion.
The wire in the SB reduces the angle between the main and side branch by an average of 30 °, which contributes to an easy change of wires (24).
Next, pre-dilatation is performed if necessary. A stent is inserted and implanted into the MB. The choice of the stent should be based on the maximum possible increase in the diameter of the stent, which allows to achieve the optimal apposition of the stent cells in the MB and the patency of the ostium of the SB. The use of stents with an ``open cell`` design is preferred in this case before using stents with ``closed cells`` (25). Then proximal optimization technique is performed.
Proximal optimization technique (POT): First presented at a meeting of the European Bifurcation Club in 2008 by surgeons Leymarie and Darremont as a way to correct stent malapposition in the proximal MB. Performed by inflating a short, non-compliant high-pressure (NC) balloon directly proximal to the carina area. In this case, the distal part of the distal label of the balloon should be located at the level of carina, while the proximal mark should be within the stent to avoid complications such as dissection or occlusion of the ostium of the SB.
The disadvantage of POT is varying degrees of expansion of the proximal segment of various stents, which can lead to the formation of various gaps between cells and even to a violation of the coverage of the stent over a large length of the vascular wall.
Wire re-crossing. Re-insertion of the wire from the MB into the SB through the cell most closely located in the carina region, accompanied by better coverage of ostium of the SB with the stent after performing “kissing” dilatation (24). After that, the wire under the stent should be removed and held in the distal sections of the MB.
“Kissing” dilatation. The goal is to achieve an optimal apposition of stent cells at the ostium of the SB, as well as to optimize the fit of the stent in the proximal segment of the MB.
Mortier et al. proposed to perform sequential dilation, starting from the SB. The technique consists of performing POT and changing wires with subsequent dilatation of the SB (12 atm) by the first stage, and the second stage of the MB (12 atm) with simultaneous dilatation of the SB (4 atm). This reduces the elliptical deformation of the stent at the end of the dilatation and optimizes SB access (25, 26).
Another study also showed that prolonged (up to 60 sec) balloon inflation is accompanied by a large stent opening, therefore it is recommended to perform 3 inflations of 20 sec (27, 28).
"Culotte" technique. Stenting of BL of coronary arteries of the type “culotte” or “stent-trousers” was first described by Chevalier et al. in 1998 and is considered one of the most elegant stenting techniques for both bifurcation branches (29, 30). The technique is used in the absence of a large difference in diameter between the main and lateral branches, otherwise there is a high risk of incomplete apposition of cells in the proximal segment of MB during stent implantation in SB.
After predilation of both branches, one of the wires is removed, as a rule, from a more direct branch, which is often the main. The SB is stenting first. After that, the wire is removed from the stented branch and inserted through the stent cell into the non-stented branch. The stent cell is expanded with a balloon catheter. A second stent is inserted through it so that its proximal part is located inside the proximal part of the previously implanted stent. A second stent is implanted in the MB. Then, a wire is inserted into the SB through the cell of the second stent and the final bifurcation is performed according to the “kissing balloons” technique as shown in Figure 2.
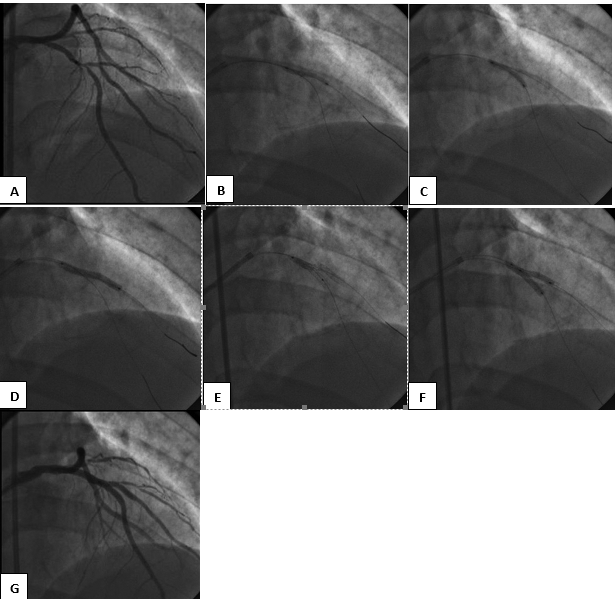
Figure 2. An example of stenting using the culotte technique: A - initial coronary angiogram, B - wires were guided to the anterior descending artery (LAD) and the diagonal artery (DA), predilation DA, C – predilation LAD, D - stent implantation in the DA, wire re-crossing, E - implantation of a second stent in LAD, wire re-crossing, stent dilatation with an non-compliant balloon, F - final “kissing-balloon” dilation, G - final angiographic result.
A feature of this technique is that proximal to the bifurcation of the artery is covered by two layers of stents, distal to the bifurcation of the main and side branches are covered by one stent. It is logical to assume that the formation of bifurcation in this way using coated stents will create a double concentration of the drug substance proximal to the bifurcation and could theoretically interfere with normal stent endothelialization.
The disadvantage of this method is the need for sequential repeated passage through stent cells in both branches, which can be a technically difficult task and take a lot of time. In addition, excessive expansion of the proximal stent of the MB can lead to significant deformation and rupture of stent cells (1).
T-stenting. This method is suitable when the angle between two vessels is close to 90 °. A stent is implanted in SB covering its ostium with very minimal protrusion into the lumen of the MB. Then the MB is stented, followed by the re-crossing of the wires and the “kissing” dilation.
The advantages of this method of stenting are that the change of wires occurs after the implantation of the second stent and the probability of losing the clearance of the main or SB is minimized. This method provides a good reconstruction of carina, but is associated with the risk of leaving a small gap between the stents, therefore, subsequent restenosis at the ostium of the SB. The T-stenting technique is most often used in the transition from provisional stenting to SB stenting.
Colombo et al. proposed modified T-stenting technique (31). It consists in the simultaneous placement of stents in the side and main branches. First, a stent is implanted in SB, and after removal of the balloon and wire, a stent is implanted in MB. The wire is reintroduced into the SB and dilatation is performed according to the “kissing balloons” technique (to correct possible deformation of the stent in SB during stenting of the MB). The described technique is useful in a situation where the SB departs at an angle close to 90 °. Its main advantage is accurate stenting of the SB ostium.
Protrusion T-stenting (TAP) is a modification of T-stenting which purpose is to completely cover carina with a stent. More often, the method is used with an inadequate result of single-stent tactics. The bottom line is the implantation of a stent in the SB with a deliberate minimum protrusion into the lumen of the MB, while the balloon is positioned in the MB deflated. After the stent is implanted in the SB, the stent balloon is pulled back and dilatation is performed according to the “kissing balloons” technique as shown in Figure 3 (1).
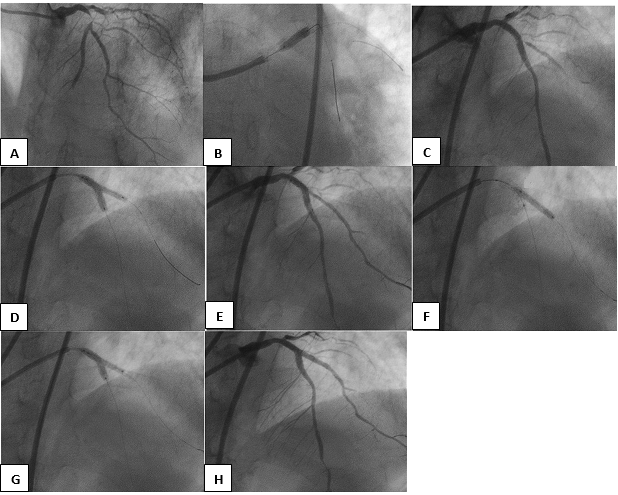
Figure 3. T-stenting and protrusion (TAP): A - initial coronary angiogram, B - wires were inserted into the anterior descending artery (LAD) and the diagonal artery (DA), a stent was implanted in the LAD, C - pronounced stenosis of the DA ostium and reduced blood flow are visualized, D - “kissing” dilatation, E - residual stenosis of the DA ostium is noted, F - a stent is implanted in the DA with low protrusion into the lumen of the LAD, G - the balloon of stent in DA is pulled back and “kissing” dilation is performed, H - final result.
The “crush” stenting technique: The crush technique, also proposed by Colombo, is an “extreme” version of a two-stent strategy. The classical technique consists of stenting the SB, stenting the MB with squeezing the stent in the SB, re-introducing the wire through three layers of the stent in the SB to perform the final “kissing” dilation (32, 33).
The disadvantages of the classical “crush” technique are the difficulty of re-introducing the wire into the SB, which is the frequency of the inability to complete the “kissing” intervention by dilatation in 20-25% of cases (33). Due to the limitations of the classic crush technique, other variations of this technique have been developed to facilitate the final kissing dilatation.
1."Crush" with minimal stent protrusion in SB ("Mini-crush").
2.Reopening the ostium of the SB by performing “kissing” dilation before stent implantation in the MB (“Double Kissing (DK) - crush”).
The DK-crush modification involves a double “kissing” dilation and consists of the following steps: stenting of the SB with 1-2 mm protrusion, squeezing of stent cells with a balloon located in the MB, the first “kissing” dilation, stenting of the MB and final “kissing” dilation.
The DK-crush technique allows both stents to be positioned and implanted sequentially and accurately, as well as to perform interventions using a 6F guide catheter (Fig. 4). According to the first experience with this technique, the final “kissing” dilatation was successfully completed at 100% (33).
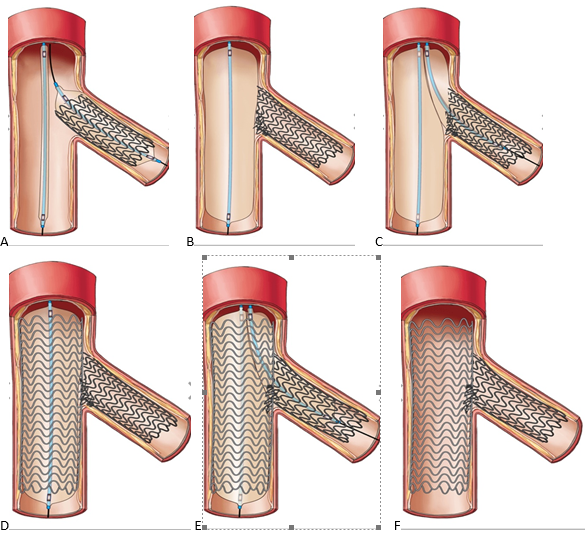
Figure 4. DK-Mini-crush technique: A - stent implantation in the SB with protrusion, B - squeezing the stent with a balloon in the MB, C - first “kissing” dilation, D - stenting of the MB, E - final “kissing” dilation, F - final result
Also, there is a mention in literature on a new technique called “nano-crush technique”. It is used in Medina 1:1:1 situations and is similar to method DK-crush technique. The only difference is that the balloons in the MB and the stent in the SB are inflated simultaneously (34). This technique is not yet very popular and is rarely used in clinical practice.
A technique for accurately positioning a stent according to Szabo for lesions of the 0: 1: 0 and 0: 0: 1 type according to Medina and well-head lesions of the LM was proposed by Szabo et al in 2006. Researchers led by Dr. Guitierez-Chico compared the results of this technique with traditional stent positioning (35). Intervention using the Szabo technique was carried out as follows: a wire is introduced in the stentable vessel; a second wire is introduced in the non-stentable vessel. Then, a stent is drawn along the first wire. The second wire is carefully guided through the proximal cell of the stent. The resulting system of two wires allows you to accurately position the stent at the ostium of the vessel, while the second wire plays the role of a limiter. After positioning, the stent is inflated under a pressure of 6 atmospheres. Wire-limiter is removed, after which the stent balloon expands to the proper diameter. If necessary, after stent deployment, kissing-dilation is performed. However, given its certain difficulties in the execution of the technique, this method is used quite rarely.
The impossibility of creating an “ideal” geometric structure using various bifurcation stenting techniques, as well as the high frequency of restenosis in SB, contributed to the development and implementation of special bifurcation stents in clinical practice. Recent stent generations include AXXESS, TRYTON Side-Branch Stent, E-TRYTON 150 bifurcation structures, coated with a biodegradable polymer, that releases biolimus and allowing both bifurcation branches to be stented simultaneously (36). At the end of 2009, the first randomized trial TRYTONLM was announced, which was dedicated to assessing the safety and effectiveness of the combined use of the TRYTON bifurcation stent and the Xience Prime stent.
The stent is first introduced in the SB, and then any conventional stent can be implanted in the MB. In Europe, the third generation bifurcation stent “Nile Pax” (Minvasys, France) coated with paclitaxel is approved for use. It uses non-polymer technology, which should reduce the intensity of inflammatory processes after implantation (6).
BIOSS optimized bifurcation stent (Poland) is a two-piece tubular balloon-expandable stent with proximal larger diameter and distal smaller diameter. In addition, in the middle of the stent there is a wide cell, which greatly facilitates access to the SB.
The main advantage of this stent is the ease of implantation, namely, as a conventional balloon expandable stent, as well as the presence of a wide cell opposite to the ostium of the SB. Thus, this stent is optimal for applying the T-stenting technique or provisional T-stenting. Stents of the first generation were made of steel and lacked a drug-coating. Today there are BIOSS stents coated with both paclitaxel and sirolimus, which have been proven to be highly effective in treating patients with BL of coronary arteries (37-40).
Visualization methods
Despite the fact that coronary angiography is the “gold standard” for the diagnosis of coronary lesions, in patients with bifurcation stenosis it often gives an ambiguous idea of the degree of damage, which can lead to diagnostic errors and unjustified stenting of the coronary arteries.
Since 1989, intravascular ultrasound (IVUS) has been used in clinical practice, which is today a modern method of non-X-ray diagnostics, which allows to obtain more significant information compared with coronary angiography (41). It allows to obtain a tomographic (silhouette) image, directly visualize the lumen of the vessel, directly measure the diameter and area of the lumen, and also has high resolution and makes it possible to differentially evaluate the lesion (42). Nevertheless, IVUS does not need to be considered as an alternative, but as a method complementary to angiography. Pre-performed IVUS may provide valuable information on the morphology of the plaque, its prevalence, the likelihood of bias during angioplasty and occlusion of SB (43). This makes it possible to choose the optimal tactics of stenting BL and reduce mortality and the development of acute myocardial infarction in comparison with those cases when the strategy is based only on the results of coronary angiography. However, it is worth remembering that for a better understanding of the anatomy of BL, it is advisable to carry out a catheter both in the main branch and from the side branch to the main (44, 45).
Optical coherence tomography (OCT) is another intravascular imaging technique that uses laser radiation with a wavelength of 1300 nm to obtain information about the three-dimensional structure of the vascular wall. The method was first described in 1991 by Huang et al. and used in evaluation of retina (46). From that moment, the use of optical coherence tomography in ophthalmology had begun (47). Subsequently, the method found its application in gastroenterology, dermatology, dentistry and, finally, in intravascular imaging in cardiology (48- 52). OCT can help assess the composition of the plaque (calcification, lipid, fibrotic and thrombotic components, degree of tire erosion) in order to predict the risk of SB occlusion and the need to use a strategy with two stents. In addition, OCT allows you to assess the tightness of the stent to the artery wall after implantation and, if necessary, perform repeated
post‑dilation (53, 54).
Conclusion
Bifurcation lesions of the coronary arteries remain one of the most difficult treatment problems when performing PCI. Over the years, more and more new methods for their correction have been developed and introduced into clinical practice. Some methods did not receive widespread use in clinical practice because of various shortcomings, while other techniques that proved to be simple and provide better results were actively applied and modified over time. With the advent of antiproliferative coated stents, there has been a significant improvement in the endovascular treatment of BL. The provisional approach to implantation of a single stent into the MB remains the approach of choice in many cases. However, in some BL, two stents must be implanted for complete correction. Special bifurcation stents are a new technology that may possibly further contribute to the success of one of the most difficult milestones in interventional cardiology. However, at present, they are also rarely used in practice due to difficulty in use.
As the famous expression “everything ingenious is simple” sounds, endovascular surgery does not stand still and every day develops the latest methods that will strive for maximum ease of use and please with successful results, both immediate and long-term.
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: Z.A.S. and A.K.T. are equally contributed to article preparation
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Guvercinlik, Bodrum. Summer2020, Bulent Gorenek, Eskisehir, Turkey.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

