The results of a three-year research program on assessment of primary diagnostic issue of congenital heart defects in children under 1 year and the availability of cardiac surgical care in the Kyrgyz Republic
CONFERENCE PAPER
The results of a three-year research program on assessment of primary diagnostic issue of congenital heart defects in children under 1 year and the availability of cardiac surgical care in the Kyrgyz Republic
Article Summary
- DOI: 10.24969/hvt.2019.122
- Page(s): 74-82
- Published: 17/04/2019
- Received: 06/03/2019
- Accepted: 17/04/2019
- Views: 7158
- Downloads: 5757
- Keywords: congenital heart disease, echocardiography, diagnosis, cardiac surgical care
Address for Correspondence: Taalaibek Kudaiberdiev, Scientific Research Institute of Heart Surgery and Organs
Transplantation, Bishkek, Kyrgyzstan
Taalaibek Kudaiberdiev1, Irina Akhmedova1, Bakyt Imanov1,2, Damirbek Abibillaev1, Zhunus Kadyraliev1, Nazgul Shoonaeva3, Chinara Satarova3, Gulzada Imanalieva1, Kayirnisa Tilemanbetova1, Zarema Zhakypova1, Gulnaz Tursunbekova1
1Scientific Research Institute of Heart Surgery and Organ Transplantation
2National Center for Cardiology and Therapy named after M.M.Mirrakhimov
3Kyrgyz State Medical Institute for Requalification
Abstract
In this article, the results of 3-year research program on primary diagnostics of congenital heart defects in children < 1 year of age are presented.
Key words: congenital heart disease, echocardiography, diagnosis, cardiac surgical care
IntroductionThe congenital heart diseases (CHD) are defined as proposed by Mitchell et al: “a gross structural abnormality of the heart or intrathoracic great vessels that is actually or potentially of functional significance” (1). The frequency of CHD at birth (sometimes referred to as the prevalence per childbirth) depends on how the population is studied (2). According to the World Health Organization (WHO), 1.35 million newborns with CHD are born each year (3).
When examining newborns using the echocardiography, small defects (small defects of the interventricular and interatrial septa, small sized patent ductus arteriosus (PDA)) predominate. With the inclusion of all forms of CHD into study, the prevalence of CHD, according to Hoffman and Kaplan (4) can reach 75 cases per 1000 live births. Performing an echocardiogram in all newborns revealed that about 5% have small ventricular septal defects, most of which spontaneously close for up to a year. Vast majority of newborns have delayed closure of the PDA (4). In 90% of cases CHDs are found in general populations without any particular risk factor, and only in 10% of cases CHD is associated with certain risk factors (5).
Early detection of CHD and timely cardiac surgery is essential for prognosis in children with heart defects. The total mortality from CHD without intervention is sufficiently high. Usually, in most low- and middle-income countries, the diagnosis of CHD is considerably delayed (6). The average age of the primary diagnosis establishment can vary from the first day of life to almost 80 years (7).
A previous study of CHD in Kyrgyz Republic territory showed that only 14% of children had been diagnosed before discharge from the maternity hospital, and 86% of patients had a delayed diagnosis (8).
The aim of study is evaluation of the scope of problem and gaining of novel statistical data on prevalence and detectability of CHD in various regions of Kyrgyz Republic
Objectives:
1. To assess the significance of contribution of various risk factors in complex CHD formation in intrauterine period
2. To evaluate the prevalence of CHD in newborns of Kyrgyz Republic
3. To determine the causes of disability and early mortality in adults with CHD.
Methods
The study was conducted in all territories of the Kyrgyz Republic (KR), in the high-altitude, mid-altitude and low-altitude regions, including the most remote areas (Table 1). The researchers organized more than 60 on-site evaluation of the local population.
The population of the country, according to the National Statistics Committee, is 6.4 million citizens. The average annual birth rate in the country over the past three years is 158.160 thousand annually.
Investigation was achieved by 2D transthoracic echocardiography assessment (US scanners of General Electric Vivid Е9, Phillips CX – 50 (portable)), prenatal screening was conducted by convex transducer and fetal echo program. Included groups were: newborns of 0-28 days, children under 1 year, pregnant women with more than 20th week gestation.
|
Table 1. Regions, districts of Kyrgyz Republic where study was conducted (geographical altitude is shown) |
|||
|
|
Regions of Kyrgyz Republic |
Districts |
Altitude |
|
2016 |
|
||
|
1 |
Chuy region |
Kemin district: Orphanage District hospital, Orlovka village |
Mid-altitude |
|
2 |
Issyk-Kul region |
Jeti-Oguz district |
High-altitude |
|
Ak-Suu district, Ak-Chiy djayloo |
High-altitude |
||
|
Karakol city |
Mid-altitude |
||
|
3 |
Talas region |
Regional maternity hospital and pediatric unit of Talas Regional Hospital |
Mid-altitude |
|
Talas district, maternity hospital |
Mid-altitude |
||
|
Talas district, Karaoy djayloo |
High-altitude |
||
|
4 |
Batken region |
Kyzyl-Kiya city |
Low-altitude |
|
5 |
Djalal-Abad region |
Aksy district |
Mid-altitude |
|
Ala-Buka district |
High-altitude |
||
|
6 |
Bishkek city |
City perinatal center |
Mid-altitude |
|
City maternity hospital №2, №4 ,№6, Chuy regional maternity hospital. |
Mid-altitude |
||
|
Baby house |
Mid-altitude |
||
|
2017 |
|
||
|
7 |
Chuy region |
Moskva district Regional hospital maternity unit |
Mid-altitude |
|
Tokmok city |
Mid-altitude |
||
|
Issyk-Ata district Regional hospital maternity unit |
Mid-altitude |
||
|
Djayil district Regional hospital maternity unit |
Mid-altitude |
||
|
Sokuluk district Regional hospital maternity unit |
Mid-altitude |
||
|
Kemin district Regional hospital maternity unit |
Mid-altitude |
||
|
8 |
Naryn region |
Naryn city |
High-altitude |
|
Ak-Talaa district Regional hospital maternity unit |
High-altitude |
||
|
At-Bashy district Regional hospital maternity unit |
High-altitude |
||
|
9 |
Batken region, Leylek district |
Isfana city |
Low-altitude |
|
Dostuk village |
Low-altitude |
||
|
Kulundu village |
Low-altitude |
||
|
Katyran village |
Mid-altitude |
||
|
10 |
Batken region, Batken district |
Batken city |
Mid-altitude |
|
Kyzyl-Kiya city |
Mid-altitude |
||
|
Suluktu city |
Mid-altitude |
||
|
11 |
Batken region, Kadamjay district |
Kadamjay city |
Mid-altitude |
|
12 |
Osh region |
Osh city, regional unified territorial hospital |
Mid-altitude |
|
Osh city, city perinatal center |
Mid-altitude |
||
|
|
|
Alay region |
High-altitude |
|
Gulcho village |
High-altitude |
||
|
13 |
Bishkek city |
City perinatal center City maternity hospital №2, №4, №6, Chuy maternity hospital National Institute of maternal and pediatric care City pediatric clinical hospital № 3 |
Mid-altitude |
|
2018 |
|
||
|
14 |
Chuy region |
|
|
|
Chuy regional maternity hospital |
Mid-altitude |
||
|
Tokmok city Republic orphanage disabilty center |
Mid-altitude |
||
|
Moskva district Regional hospital maternity unit |
Mid-altitude |
||
|
Belovodskoye village Belovodskoe psychoneurological house Belovodskoye baby house |
Mid-altitude |
||
|
15 |
Naryn region |
Naryn city |
High-altitude |
|
16 |
Djalal-Abad region |
Toguz-Toro district, Kazarman village |
Mid-altitude |
|
17 |
Batken region, Leylek district |
Isfana city |
Low-altitude |
|
Suluktu city |
Low-altitude |
||
|
Kulundu village |
Low-altitude |
||
|
18 |
Batken region, Batken district |
Batken regional hospital, maternity unit |
Mid-altitude |
|
Zardaly village |
High-altitude |
||
|
19 |
Bishkek |
Republic specialized center of rehabilitation of pediatric patients with central nervous system disorder City perinatal center City maternity hospital №2, №4, №6, Chuy maternity hospital National Institute of maternal and pediatric care City pediatric clinical hospital № 3 |
Mid-altitude |
Results
The research study was conducted by two sections: prenatal diagnostics and workup of newborns and children under 1 year
I. Prenatal diagnostics: Prenatal echocardiography is the most valuable method for the diagnosis of fetal heart disease. As a non-invasive and innocuous procedure, it allows examiner to fully evaluate cardiac structures, assess intracardiac hemodynamics in the prenatal period and makes it available for dynamic control during pregnancy. All these qualities determine the priority of this method in the prenatal diagnosis of fetal congenital heart disease.
A standard fetal cardiac scan is carried out at 18-22 weeks of gestation in accordance with the protocol of the reference centers (5).
We started examinations of pregnant women from the 21st week of gestation, which was explained by the first visits of women to our center.
|
Table 2. Number of conducted examinations |
||||||
|
|
|
Retrospectively 2010 - 2015 |
2016 |
2017 |
2018 |
Total |
|
1. |
Fetal echo in SRIHSOT |
850 |
79 |
57 |
62 |
198 |
|
2. |
Fetal echo in regions |
|
34 |
63 |
39 |
136 |
|
|
Total |
|
113 |
120 |
101 |
334 |
|
|
Retrospectively |
850 |
|
|
|
|
|
Table 3. Detectability of CHD by fetal echocardiography
|
||||
|
|
Years |
Investigated |
Detected |
% |
|
1 |
2016 |
113 |
14 |
12.39% |
|
2 |
2017 |
120 |
13 |
10.84% |
|
3 |
2018 |
101 |
8 |
7.92% |
|
|
Total: |
334 |
35 |
10.48% |
|
CHD – congenital heart disease |
||||
|
Table 4. Detected CHD forms by fetal echocardiography
|
||||||
|
|
CHD forms |
Outcome |
||||
|
2016 |
|
Atrio-ventricular septal defect, complete type |
2 |
|
||
|
|
Single ventricle |
1 |
|
|||
|
|
Ventricular septal defect |
5 |
|
|||
|
|
Ventricular septal defect (muscular) |
3 |
|
|||
|
|
ASD in IAS aneurysm |
2 |
|
|||
|
|
Atrial septal defect |
1 |
|
|||
|
|
|
|
||||
|
2017 |
|
|||||
|
|
Atrio-ventricular septal defect, complete type |
4 |
|
|||
|
|
Ventricular septal defect |
2 |
|
|||
|
|
Single case –ASD in IAS aneurysm |
1 |
|
|||
|
|
Hypoplastic left heart syndrome |
1 |
|
|||
|
|
Total anomalous pulmonary venous connection with tricuspid anomaly |
1 |
|
|||
|
|
Tricuspid atresia |
2 |
|
|||
|
|
Hypoplastic right heart syndrome |
2 |
|
|||
|
|
|
|
|
|
||
|
2018 |
|
|
|
|
||
|
|
Aortic dextraposition. VSD. Hypoplastic pulmonary artery. |
1 |
Ds has been confirmed, patient is on follow-up |
|||
|
|
PA stenosis ( valvular), ASD |
1 |
Ds has been confirmed, lethal outcome on 10th day |
|||
|
|
Ventricular septal defect (muscular) |
1 |
- |
|||
|
|
Persistent truncus arteriosus, Double-chamber heart. |
1 |
- |
|||
|
|
Ventricular septal defect |
1 |
- |
|||
|
|
Atrio-ventricular septal defect, complete type |
1 |
Did not born |
|||
|
|
Atrio-ventricular septal defect, complete type |
1 |
? |
|||
|
|
Total anomalous pulmonary venous connection with tricuspid anomaly, TR moderately severe |
1 |
Ds has been confirmed, lethal outcome on 3rd day |
|||
|
ASD – atrial septal defect, CHD – congenital heart disease, IAS – interatrial septum, TR – tricuspid regurgitation, VSD – ventricular septal defect |
||||||
The lack of data after birth is due to failure of the information from maternity hospitals
|
Table 5. Examination of the risk groups
|
||||
|
|
Risk factors of CHD |
Risk groups |
Detected CHD |
% |
|
1 |
Existence of CHD in mother |
58 |
10 |
17.24% |
|
2 |
Prior pregnancy CHD |
10 |
4 |
40% |
|
3 |
Arrhythmias in mother |
3 |
1 |
33.34% |
|
4 |
Chronic rheumatic heart disease |
1
|
- |
- |
|
5 |
Somatic disease in mother (SLE) |
1 |
- |
- |
|
CHD – congenital heart disease, SLE – systemic lupus erythematosus |
||||
II. Primary workup of CHD in newborns and children under 1 year:
The study included newborns and children under 1 year old in the investigated area. The presence of a structural anomaly of the heart was regarded as the presence of CHD. Patients with congenital rhythm disturbances, cardiomyopathy, myocarditis, additional persistent vena cava, patent foramen ovale, acquired valvular heart disease were excluded.
A total of 4177 patients were examined, 523 had a primary diagnosis of congenital heart disease, which was 12.52%.
|
Table 6. Results of primary examination of children |
||||||
|
|
Study |
2016 |
2017 |
2018 |
Total |
Total number of investigated children |
|
1 |
Echo in SRIHSOT |
|
|
|
|
4177 |
|
2 |
Echo in regions |
531 |
579 |
784 |
1894 |
|
|
Table 7. Detectability of CHD |
|||
|
|
0 – 1 month |
1 month – 1 year |
Total |
|
Examined |
998 |
3179 |
4177 |
|
Detected CHD |
240 |
283 |
523 |
|
Detectability% |
24.12% |
8.93% |
12.52% |
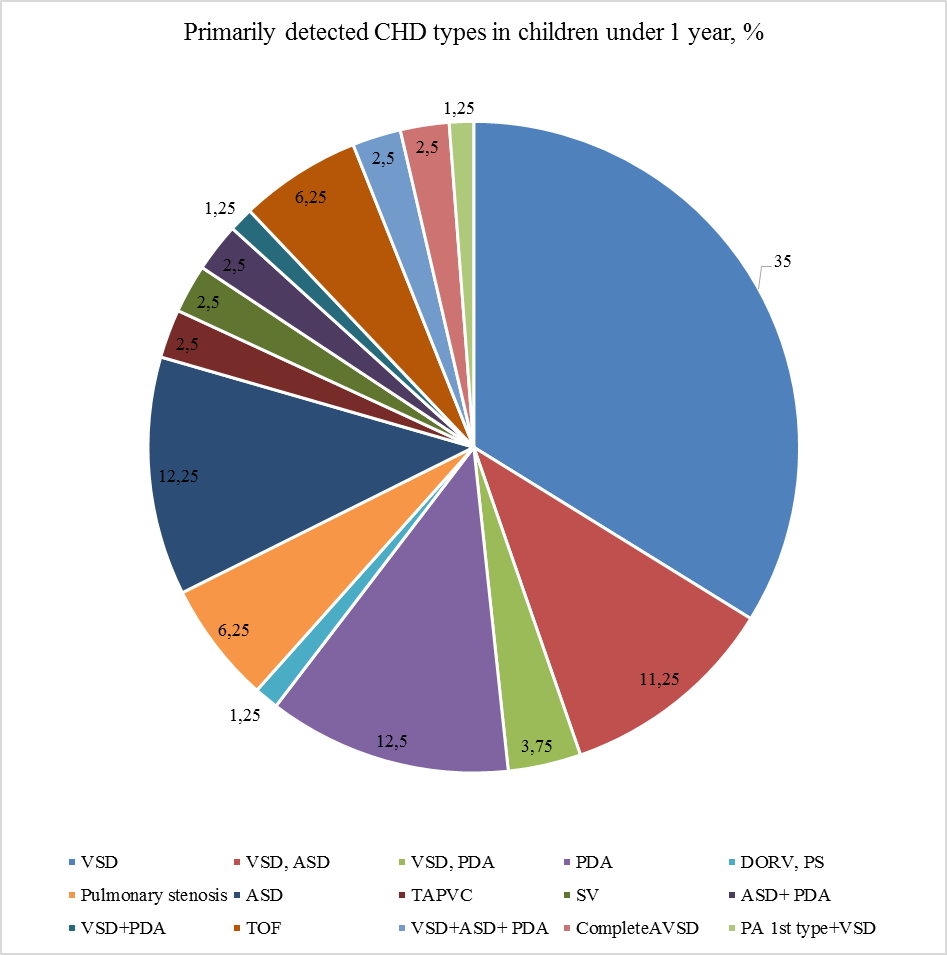
Figure 2. CHD forms detected in primary examination of children <1 year old
ASD – atrial septal defect, AVSD – atrioventricular septal defect, CHD – congenital heart disease, DORV – double-outlet right ventricle, PA- pulmonary atresia, PDA – patent dusctus arteriosus, PS – pulmonary stenosis, SV – single ventricle, TAPVC – total anomalous pulmonary vein connection, TOF – tetralogy of Fallot, VSD – ventricular septal defect
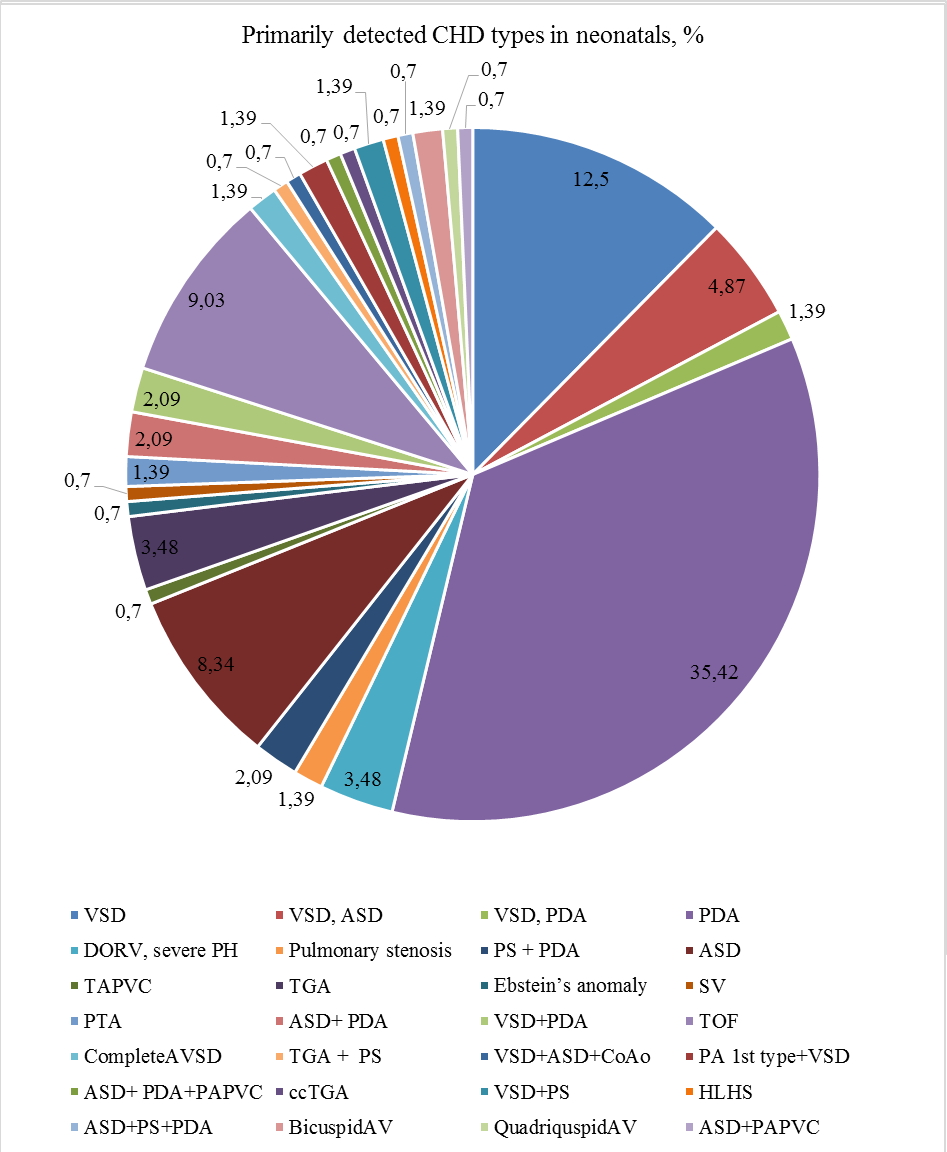
Figure 3. CHD forms detected in primary examination of newborns (0-28 days)
ASD – atrial septal defect, AV – aortic valve, AVSD – atrioventricular septal defect, CHD – congenital heart disease, CoAo – coarctation of aorta, DORV – double-outlet right ventricle, PA- pulmonary atresia, PAPVC – partial anomalous pulmonary vein connection, PDA – patent dusctus arteriosus, PH – pulmonary hypertension, PS – pulmonary stenosis, SV – single ventricle, TAPVC – total anomalous pulmonary vein connection, TGA – transposition of great arteries, TOF – tetralogy of Fallot, VSD – ventricular septal defect
- In newborns group cyanotic defects rate was 26.38%, non-cyanotic defects – 73.61%.
- In the group of children 1 month-1 year cyanotic defects 14.70%, non-cyanotic defects – 85.29%
Discussion
According to European authors, only 49% of pregnancies in Europe are planned. On the territory of our country, the exact data of the planned pregnancies is unknown, but according to a preliminary survey of the women examined, only 5% of the pregnancies were planned. The program was implemented with a focus on women with CHD in history. Only 21% of the examined pregnant women were at risk of having children with CHD.
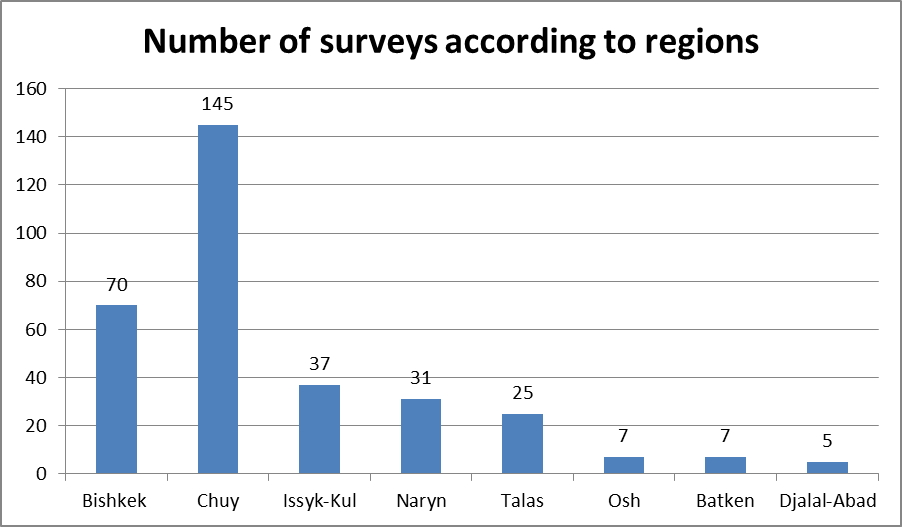
The accessibility of the study is the highest in the Chuy region and the capital of the country - Bishkek, that is, in areas located in close proximity to the central institution, and it is probably higher due to the internal migration, because the registration address during the survey have not been supplied.
The influence of high-altitude has not been revealed as a causative factor, which corresponds to the international data obtained in different years and in different altitudes (9-12).
Based on the obtained results, the most common forms of CHD (in children under 1 year old and newborn babies) in our country are “acyanotic” heart defects, such as the patent ductus arteriosus (12.5% and 35.42%), atrial septal defect (11.25% and 8.34%), ventricular septal defect (32% and 12%) and their combinations. On the other hand, assessment of newborns and the children under 1 year reveals the high prevalence of critical and complex forms of CHD requiring well-qualified care and timely surgical treatment. The proportion of detection of cyanotic defects is significantly reduced with age, which also correlates with international data that more than half of children born with cyanotic CHD do not live up to 1 year.
The main causes of disability and early mortality in vast majority of patients with CHD in remote regions of Kyrgyz Republic are late detection, lack of accessible specialized medical care, and low awareness of the parents/relatives of the patient about the importance of timely surgical treatment.
Peer-review: internal
Conflict of interest: None to declare
Authorship: T.K., I.A., B.I., D.A., Zh.K., N.Sh., Ch.S., G.I., K.T., Z.Zh., G.T. equally contributed to the study and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

