Bundle branch reentrant tachycardia treated with cardiac resynchronization therapy in a patient with dilated cardiomyopathy
CASE REPORT
Bundle branch reentrant tachycardia treated with cardiac resynchronization therapy in a patient with dilated cardiomyopathy
Article Summary
- DOI: 10.24969/hvt.2019.128
- Page(s): 105-108
- CARDIOVASCULAR DISEASES
- Published: 03/05/2019
- Received: 01/05/2019
- Accepted: 03/05/2019
- Views: 9779
- Downloads: 7703
- Keywords: bundle branch reentrant tachycardia, ventricular tachycardia, cardiac resynchronization therapy
Address for Correspondence: Panagiotis Koudounis, Red Cross Hospital, Athens, Greece, 11526
Tel: 0030 2132068005 Email: panagiotis.koudounis@gmail.com
1 1st Department of Cardiology, Red Cross Hospital, Athens, Greece
2 4th Department of Internal Medicine, Athens National and Kapodistrian University, School of Medicine, Attikon University General Hospital, Athens, Greece
Abstract
A 66 years old woman with known dilated cardiomyopathy and severely reduced ejection fraction presented with bundle branch reentrant tachycardia. Bundle branch reentrant tachycardia is an uncommon form of ventricular tachycardia incorporating both bundle branches into the reentry circuit. The diagnosis is based on electrophysiological findings and pacing maneuvres that prove participation of the His- Purkinje system in the tachycardia mechanism. Radiofrequency ablation of right bundle is proposed as the first line therapy. In our patient, the ablation imposed a high risk of complications in view of the existing conduction defects. We decided to proceed with a CRT – D implantation, which improved patient’s symptoms and diminished ventricular tachycardia episodes. As a result, biventricular pacing may serve as an alternative method to ablation treatment.
Key words: bundle branch reentrant tachycardia, ventricular tachycardia, cardiac resynchronization therapy
Introduction
We present a case with dilated cardiomyopathy and bundle branch re-entrant tachycardia (BBRT) treated with cardiac resynchronization therapy-defibrillator (CRT-D).
BBRT is an uncommon form of ventricular tachycardia incorporating both bundle branches into the reentry circuit. Radiofrequency ablation of right bundle is proposed as the first line therapy. In our patient, ablation deemed as a high risk procedure due to existing conduction defects. We decided to proceed with CRT – D implantation, which improved patient’s symptoms and attenuated ventricular tachycardia recurrences.
Case
A 66 years old woman with known dilated cardiomyopathy and severely reduced ejection fraction presented in our clinic with progressive dyspnea on minimal exertion (NYHA Class III – IV). Physical examination revealed blood pressure 90/70 mmHg, fine crackles over lung basis, a third heart sound, distended jugular veins and mild peripheral pitting oedema.
Drug therapy history included ramipril 5mg once daily, spironolactone 25 mg once daily and furosemide 40 mg once daily. Laboratory results showed only an elevated BNP level-850pg/ml.
Electrocardiogram at presentation demonstrated sinus rhythm with markedly prolonged PR interval, right bundle branch block with left axis deviation and frequent runs of wide complex tachycardia with QRS morphology same as in sinus rhythm (Fig. 1, 2).
Echocardiogram reported a dilated left ventricle with diffuse hypokinesia, severely depressed ejection fraction=20%, preserved right ventricular function, moderate mitral regurgitation and elevated filling pressures (Fig. 3).
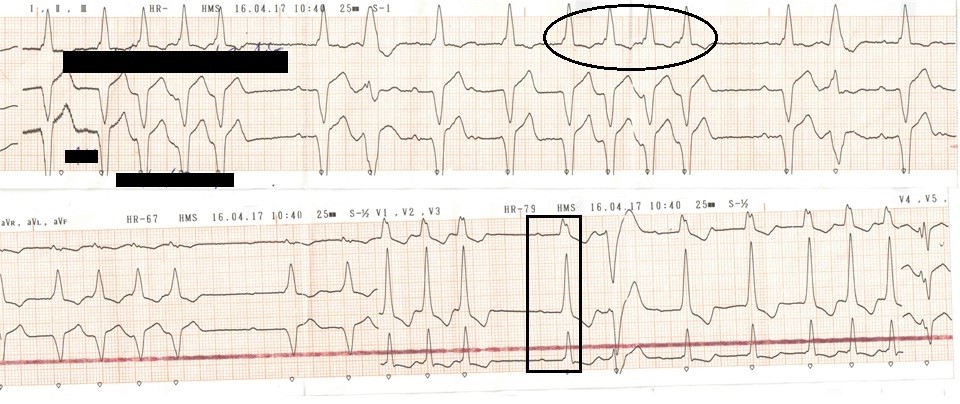
Figure 1. ECG at presentation. Sinus rhythm with markedly prolonged PR interval, right bundle branch block (black square) with left axis deviation and frequent runs of wide complex tachycardia with QRS morphology same as in sinus rhythm (black circle)
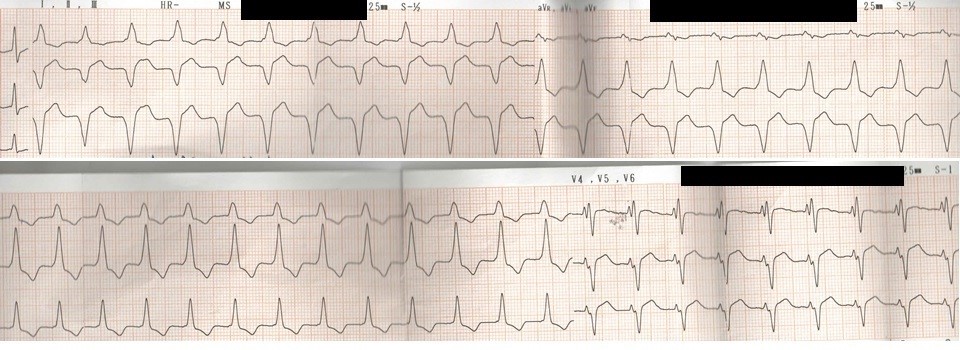
Figure 2. Self-terminated sustained episode of wide complex tachycardia in the same patient
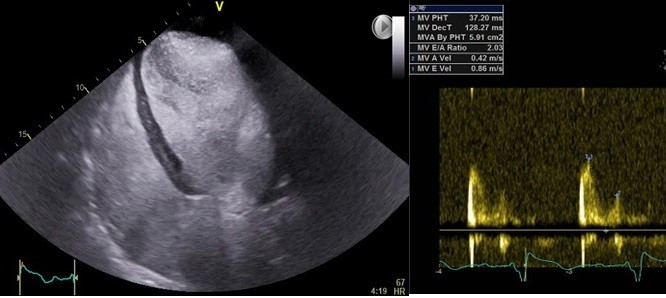
Figure 3. Echocardiogram at presentation demonstrated severe left ventricular dilatation with increased filling pressures.
We performed an electrophysiological study in order to investigate the nature of the wide complex tachycardia. Baseline intervals in sinus rhythm were: cycle length (CL)=826ms, AH=76ms, HV=220ms and QRS=176ms (Fig. 4). The clinical tachycardia that was reproducibly induced with atrial extrastimulation at 600ms and one extrastimulus at 400ms, had CL=487ms , HV= 318ms and atrioventricular (AV) dissociation confirming the diagnosis of BBRT (Fig. 5).
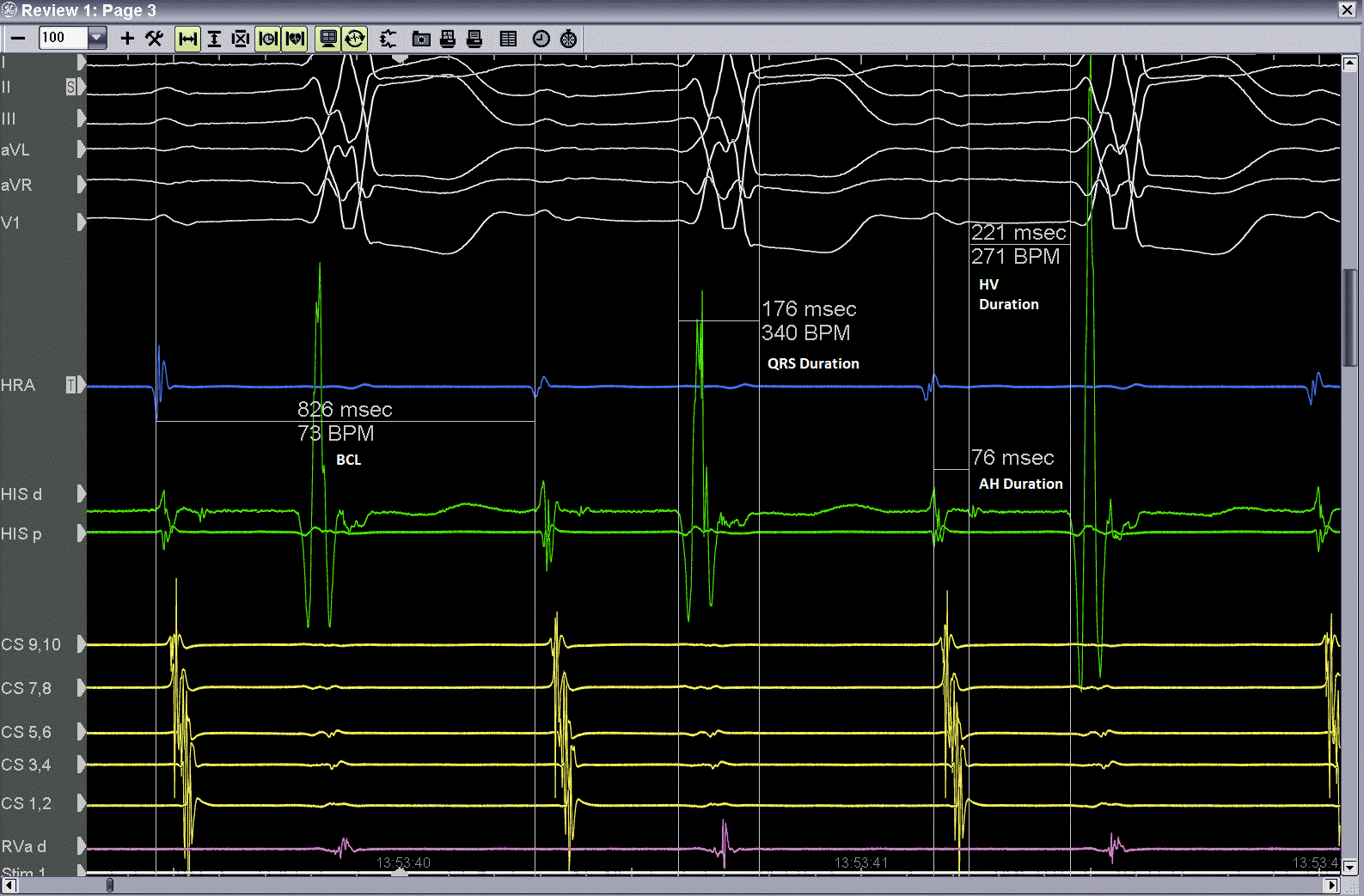
Figure 4.Electrophysiological study. Baseline intervals
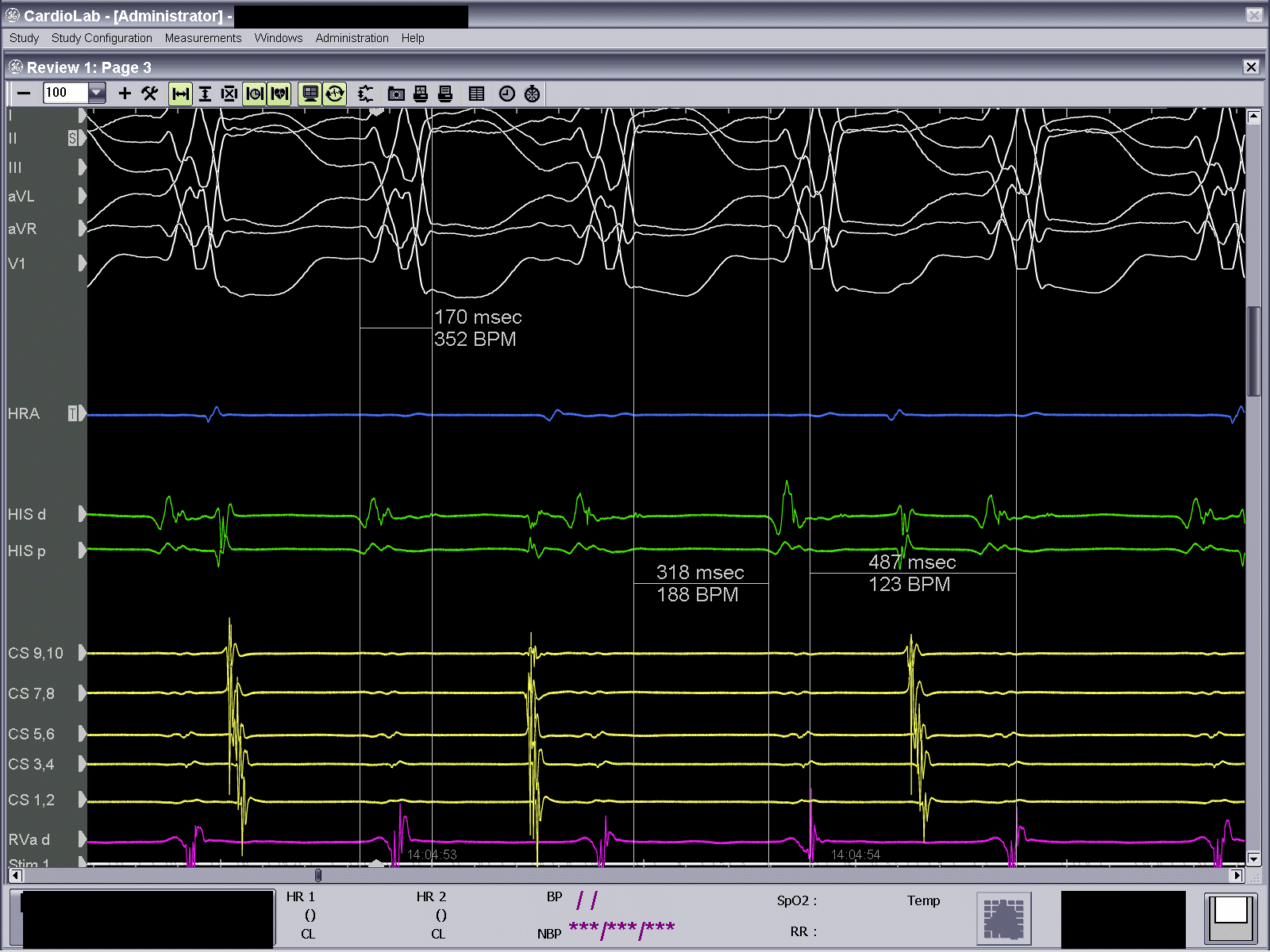
Figure 5. Clinical tachycardia reproduced at electrophysiology laboratory. CL=487ms, HV= 318ms and AV dissociation confirming the diagnosis of bundle branch reentrant tachycardia
Discussion
BBRT is an uncommon form of ventricular tachycardia (VT) incorporating both bundle branches into the reentry circuit (1). It is often seen in patients with cardiomyopathy and conduction defects (2). The QRS morphology during VT is a typical bundle branch block pattern, usually with left bundle branch block. In addition, the CL of the tachycardia is very short and patients become severely symptomatic in contrast to our findings with extremely long CL of the tachycardia. The diagnosis is based on electrophysiological findings and pacing maneuvres that prove participation of the His- Purkinje system in the tachycardia mechanism (3). Antiarrhythmics are not helpful, with radiofrequency ablation of right bundle regarded as the first line therapy (4).
In our patient, the ablation imposes a high risk of complications in view of the existing conduction defects. Consequently, we decided to proceed at first with a CRT – D implantation that allowed us to optimize medical treatment according to the current guidelines and evaluate the ablation strategy in one month. Patient’s follow up surprisingly revealed no VT episodes and marked symptomatic improvement, supported by device interrogation (report demonstrated increasing thoracic impedance and enhanced patient’s activity).
Clinical implication/ Conclusion
We describe the first bundle branch re-entrant tachycardia treated with cardiac resynchronization therapy. The rationale is that biventricular pacing can intervene in the tachycardia circuit interrupting the re-entry mechanism. As a result, biventricular pacing may serve as an alternative method to ablation treatment.
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: P.K., P.C.F., M.A., A.C., P.M., I.T., N.B., A.K. equally contributed to case report and fulfilled authorship criteria
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

