Right ventricular strain
REVIEW
Right ventricular strain
Article Summary
- DOI: 10.24969/hvt.2020.187
- Page(s): 16-25
- Echocardiography
- Published: 02/03/2020
- Received: 15/02/2020
- Accepted: 24/03/2020
- Views: 20039
- Downloads: 7984
- Keywords: right ventricle, echocardiography, Doppler echocardiography, TAPSE, myocardial performance index, strain analysis
Address for Correspondence: Oben Baysan, Guven Hospital, Ankara, Turkey, Email: obbaysan@gmail.com
1Guven Hospital Cardiology Clinic, Ankara, Turkey
2Private cardiology clinic, Izmir, Turkey
Abstract
This review is devoted to comprehensive echocardiographic analysis of right ventricular function - right ventricular strain rate analysis.
Key words: right ventricle, echocardiography, Doppler echocardiography, TAPSE, myocardial performance index, strain analysis
Introduction
Left and right sides of the heart are interconnected with each other both functionally and structurally. Left ventricle is the most studied part of the heart however, in recent years other parts of the heart have also gained attention. Luckily, right ventricle (RV) is one of them. Right ventricle has a long history starting from being realized as an unnecessary part of the heart to its recognition as a respectful and an indispensable part of the heart.
Magnetic resonance imaging (MRI) is the preferred imaging method for RV evaluation (1) however echocardiography is the most frequently used one due to its widespread availability, safety, repeatability, and real time imaging with high temporal and spatial resolution (2). In our previous reviews in depth analysis of left ventricle and left atrium were discussed (3, 4).
Here in this mini review we will focus on echocardiographic deformation imaging of the right ventricle and its derived parameters.
Right Ventricle: Brief Physiology
The right ventricle with borders from tricuspid valve to pulmonic valve has three parts: Inflow, apical trabecular and outflow (infundibular). The principal work done by the RV is the transfer of blood flow coming from systemic venous circulation to pulmonary circulation. Apart from interventricular septum, the RV’s obliquely oriented superficial fibers and deep longitudinal fibers are the main tools for accomplishing this work (5). The right ventricle’s contraction begins in inflow section and spreads to the apical and infundibular sections with 25-50 msec time intervals (6). Peristaltic contraction of the RV creates a stroke volume equal to left ventricle (7).
Major contribution to the RV stroke volume comes from longitudinal contraction and pulling of its free wall towards interventricular septum. About 15% of RV’s stroke volume is provided by infundibulum (7). Left ventricular contraction has a very important effect on RV function via the shared interventricular septum which is called ventricular interdependence. About 20% to 40% of the pressure increase in the RV is because of left ventricular contraction (8). In contrast to left ventricle, rotational or circumferential shortening has a very little role in the stroke volume generation of the RV (9). Low resistance and high capacitance of pulmonary circulation also provides a basis for lower stroke work of RV (10).
Right Ventricle: Echocardiographya)Diameter Measurement
Right ventricular dysfunction has prognostic importance on several diseases including pulmonary hypertension (11) and myocardial infarction (12). Therefore, early recognition of RV dysfunction is a very important task for a clinician, which leads to the ways for implementing of appropriate therapies.
The RV has an anterior location in thorax and its complex shape precludes a thorough evaluation from a single echocardiographic window. A simple diameter measurement seems logical for determination of RV dilatation, albeit it is a relatively late finding. Multiple echocardiographic windows can be used for that purpose including apical four-chamber, parasternal long-axis and short-axis views at the aortic valve level, RV inflow view, subcostal and RV focused views (Fig. 1a-f) (13). Reference values for RV dimensions and their respective cut-off values are provided in Table 1 (13-14). Right ventricular focused views can be preferred in diameter measurements due to their better reproducibility (15).
|
Table 1. Reference values (13) and the cut-off values (14) for right ventricle diameter measurements |
||||
|
Parameter |
Mean (SD) |
Normal Range |
Cut-Off Value |
|
|
RV basal diameter , mm |
33 ( 4) |
25-41 |
<42 mm |
|
|
RV mid diameter , mm |
27 ( 4) |
19–35 |
<36 mm |
|
|
RV longitudinal diameter , mm |
71 ( 6) |
59–83 |
|
|
|
RVOT PLAX diameter, mm |
25 (2.5) |
20–30 |
|
|
|
28 (3.5) |
21–35 |
<36 mm |
|
|
RVOT distal diameter, mm |
22 (2.5) |
17–27 |
<28 mm |
|
|
RV wall thickness, mm |
3 (1) |
1–5 |
|
|
|
RV- right ventricle, RVOT – right ventricular outflow tract, RVOT PLAX - right ventricular outflow tract Parasternal long axis view |
||||
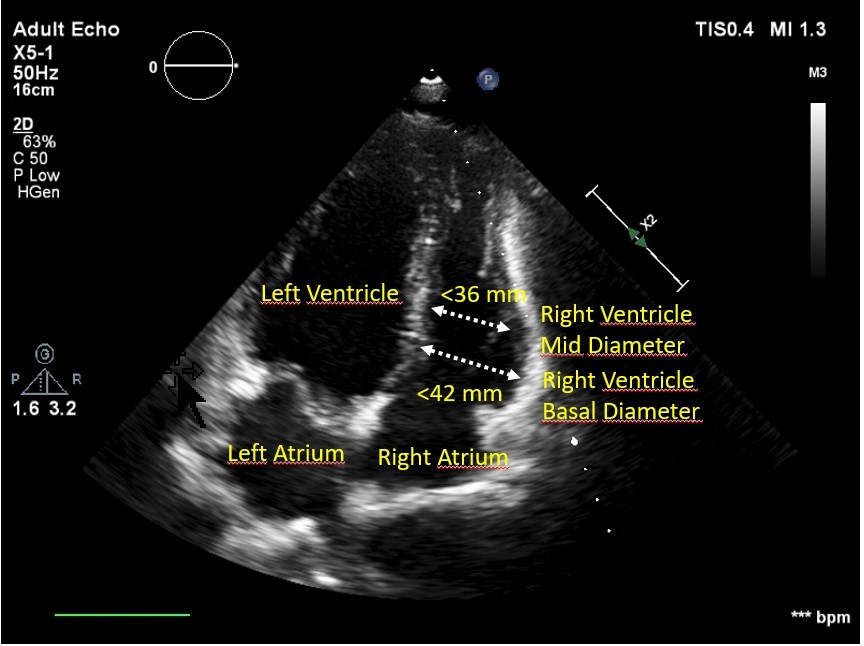
igure 1a. Apical 4-chamber view of right ventricle
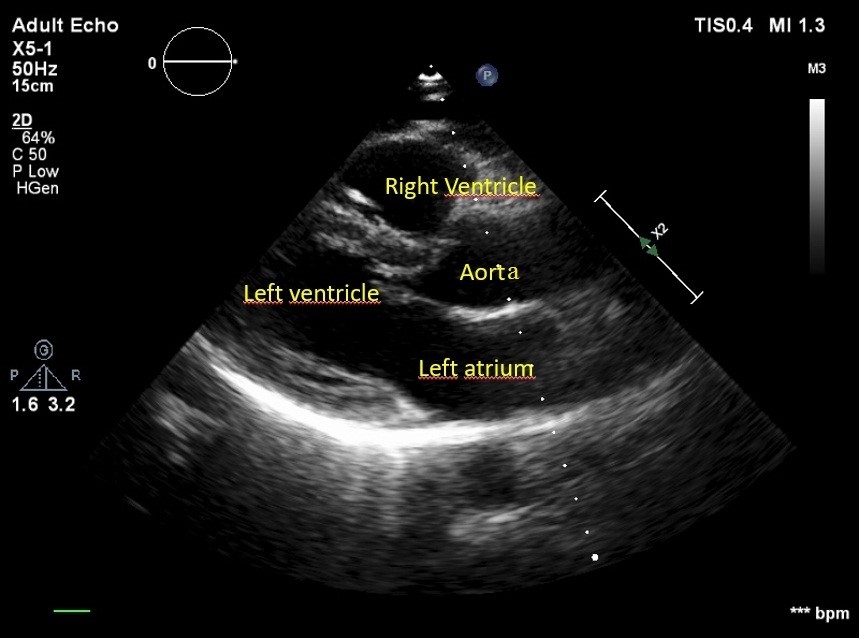
Figure 1b. Right ventricular outflow tract: parasternal long-axis view
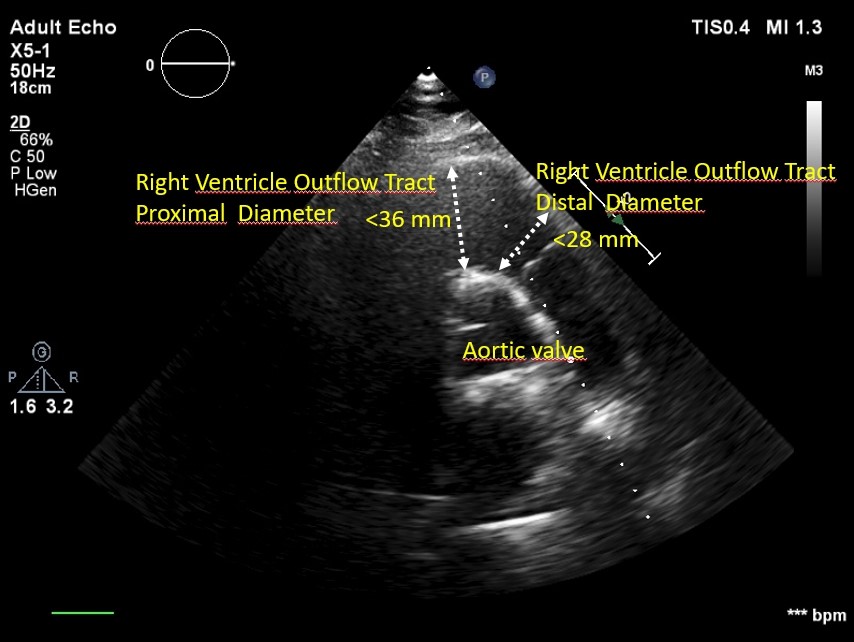
Figure 1c. Right ventricular outflow tract: parasternal short-axis view at the aortic valve level
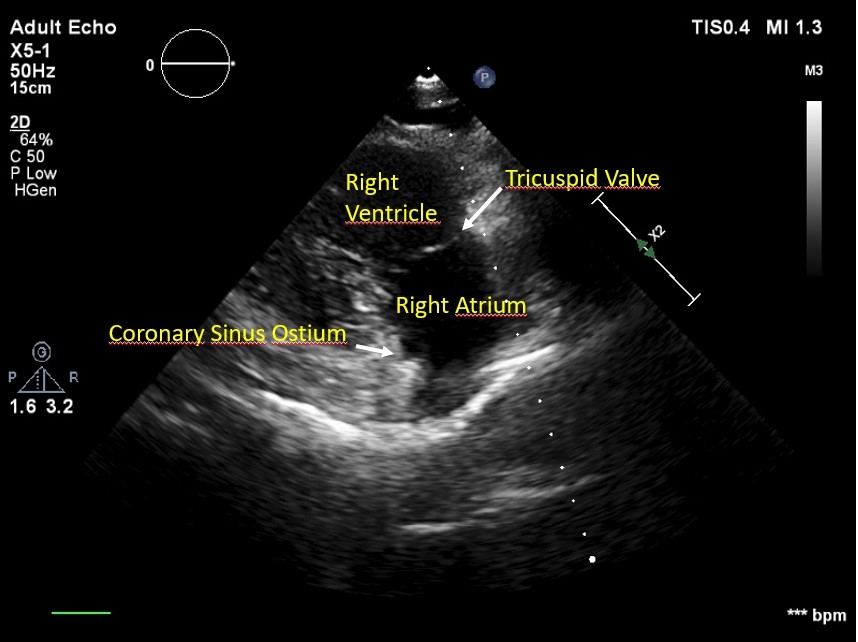
Figure 1d. Right ventricular inflow view
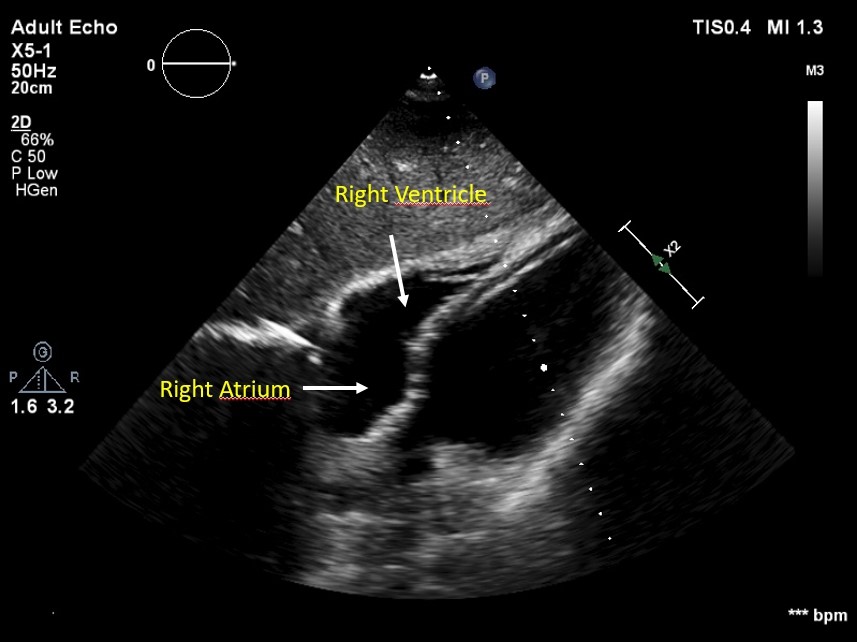
Figure 1e. Subcostal view of right ventricle
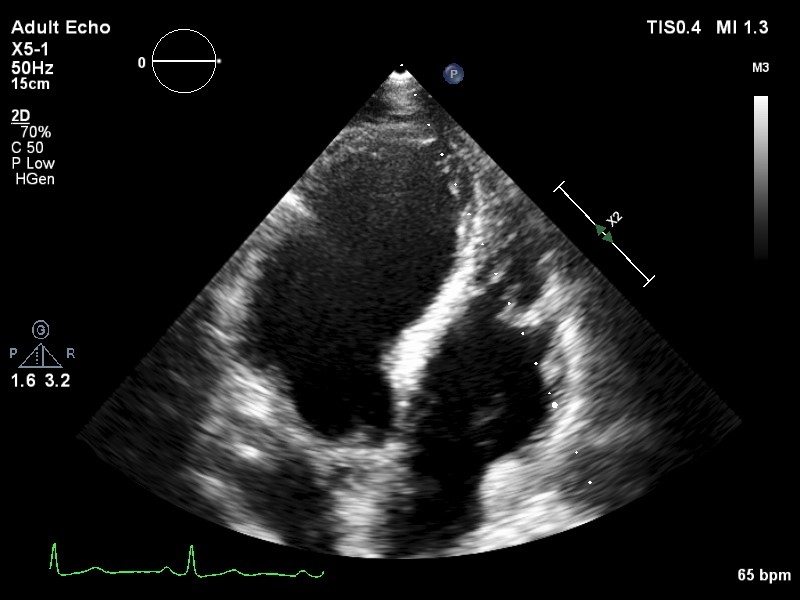
Figure 1f. Right ventricular focused view
b) Right Ventricular Systolic Performance Analysis
The surrogate markers principally reflecting longitudinal shortening has gained widespread acceptance in practical echocardiographic evaluation of the RV. M-Mode based tricuspid annular plane systolic excursion (TAPSE) (Fig. 2a) and tissue Doppler imaging (TDI) based pulsed wave (PW) S velocity (TDI S wave) (Fig. 2b) are the most frequently used longitudinal shortening markers. Their cut-off values are shown in Table 2. TAPSE and TDI S wave are angle dependent, and hence, apical 4-chamber view is more suitable for their measurement. Although very frequently used TAPSE and TDI S wave measure only very localized portion of RV (lateral tricuspid annulus). It is assumed that this area correctly reflects the global RV function. However, any disease causing a localized damage such as RV myocardial infarction makes this assumption invalid.
RV myocardial performance index (RVMPI) is the ratio of the sum of isovolumic contraction and relaxation time divided by ejection time. PW or TDI PW can be used for its calculation. RV MPI values >0.43 by PW or >0.54 by TDI PW suggest RV dysfunction (16). RV MPI is not reliable in the setting of elevated right atrial pressure (13).
Right ventricular fractional area change (RV FAC) is a 2-dimensional echocardiography based method relying on correct identification of systolic and diastolic RV areas. Its formula is:
RV FAC (%) = 100 × (end-diastolic area- end-systolic area)/end diastolic area.
A value lower than 35% accepted as abnormal. RVFAC neglects about 25%- 30% of the RV volume in the outflow tract. Drawing of endocardial contour in the heavily trabeculated RV is not an easy task, which increases interobserver variability (13).
|
Table 2. Reference values for TAPSE and TDI S wave |
||
|
Parameter |
Mean (SD) |
Normal Range |
|
TAPSE, mm |
24 (3.5) |
>17 |
|
TDI S wave, cm/sec |
14.1 (2.3) |
>9.5 |
|
TAPSE - tricuspid annular plane systolic excursion, TDI S wave- tissue Doppler imaging based pulsed wave S velocity |
||
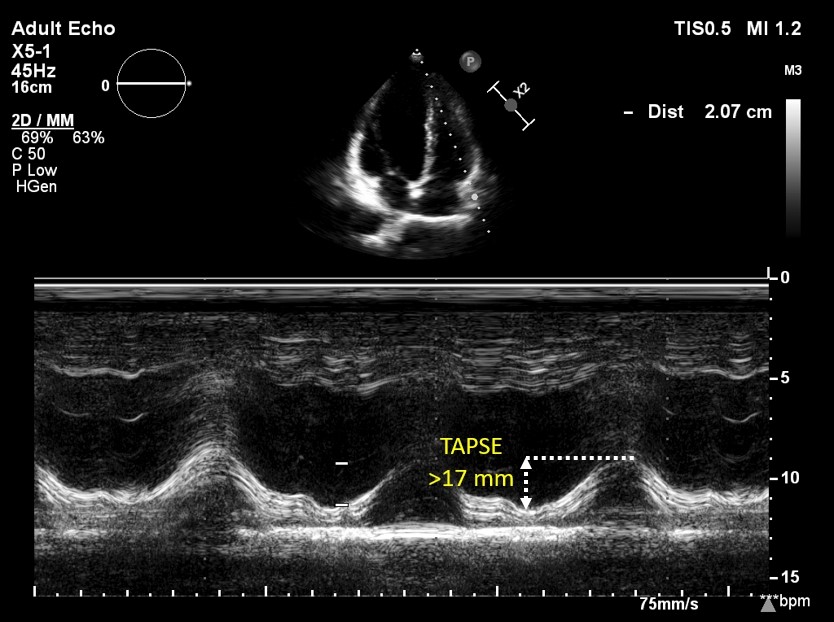
Figure 2a. M-Mode TAPSE
TAPSE - tricuspid annular plane systolic excursion
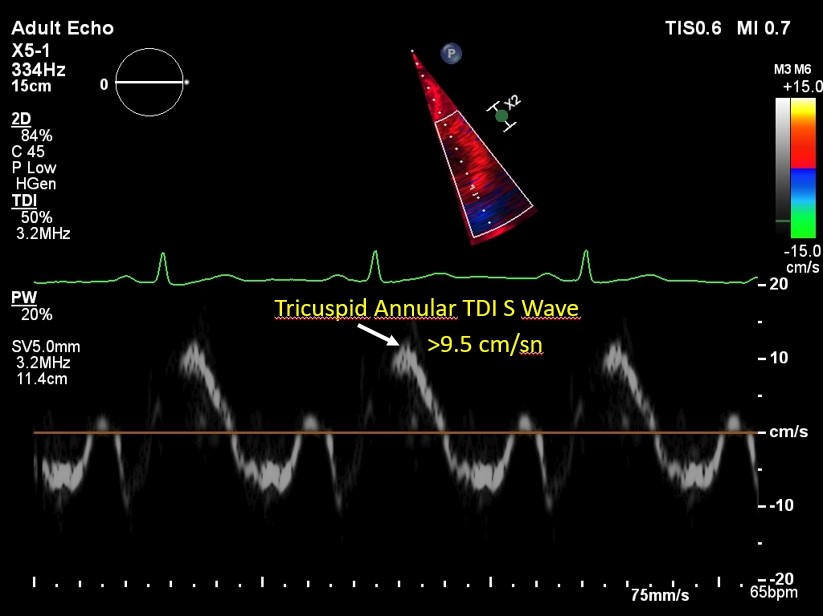
Figure 2b. TDI S wave
TDI S wave- tissue Doppler imaging based pulsed wave S velocity
c) Right Ventricular Strain
Nowadays, speckle-based deformation imaging has a very important place in daily routine of echocardiography laboratories due to its less dependence on imaging angle compared to other methods such as TAPSE and TDI S wave. It is a feasible and repeatable method for measuring RV function (17).
RV systolic strain is a load dependent measure of RV deformation (18) and has significantly better correlation with MRI based RVEF measurements compared to other indices of RV function (19,20).
A focused RV view obtained from apical four-chamber view is usually used for RV strain analysis with better reproducibility (21). RV strain measurement needs high quality images with a frame rate more than 40 frame/sec.
Strain analysis software developed for left ventricle is applied to RV. An end-diastolic frame is selected with manual selection of anatomic landmarks (lateral tricuspid annulus, septal tricuspid annulus and apex), which automatically creates a region of interest (ROI) between RV endocardium and epicardium. ROI definition is the most important part of strain measurement, which directly affects measured strain values. A default ROI width of 5 mm is recommended due to thin RV wall (21). Both the RV free wall and interventricular septum should be included (Fig. 3) (21). ROI can be manually adjusted in width and position to fit the RV. Too low positioning of the sample volume on the tricuspid annulus /on the right atrial side or too wide selection of ROI with pericardial inclusion must be avoided; otherwise, strain values would be underestimated.
After correct positioning, the software automatically calculates strain values from six segments pertinent to the RV: three free wall and three interventricular segments (basal, mid and apical). The RV shortens in longitudinal direction during systole, which leads to negative strain values on the graph. More negative values points to more deformation.
The echocardiographer should select which RV strain data to use. There are two options for the operator to select from RV strain data; RV global longitudinal strain (RVGLS) and RV free wall strain (RVFWS). RVGLS contains deformation data from interventricular septum and RV free wall. RVFWS provides data from whole free wall and hence is the better surrogate marker for RV function. It has additive predictive value (16). Which one is more useful clinically is still controversial. Recent guideline about deformation imaging recommends that RV longitudinal deformation should be reported as RVFWS and leave RVGLS as optional (21).
RVFWS can be calculated from two models: 6-segment or 3-segment model. In the first model all six segments are used for strain calculation and then a simple average value for three free wall segment peak strain is calculated (Fig. 3).
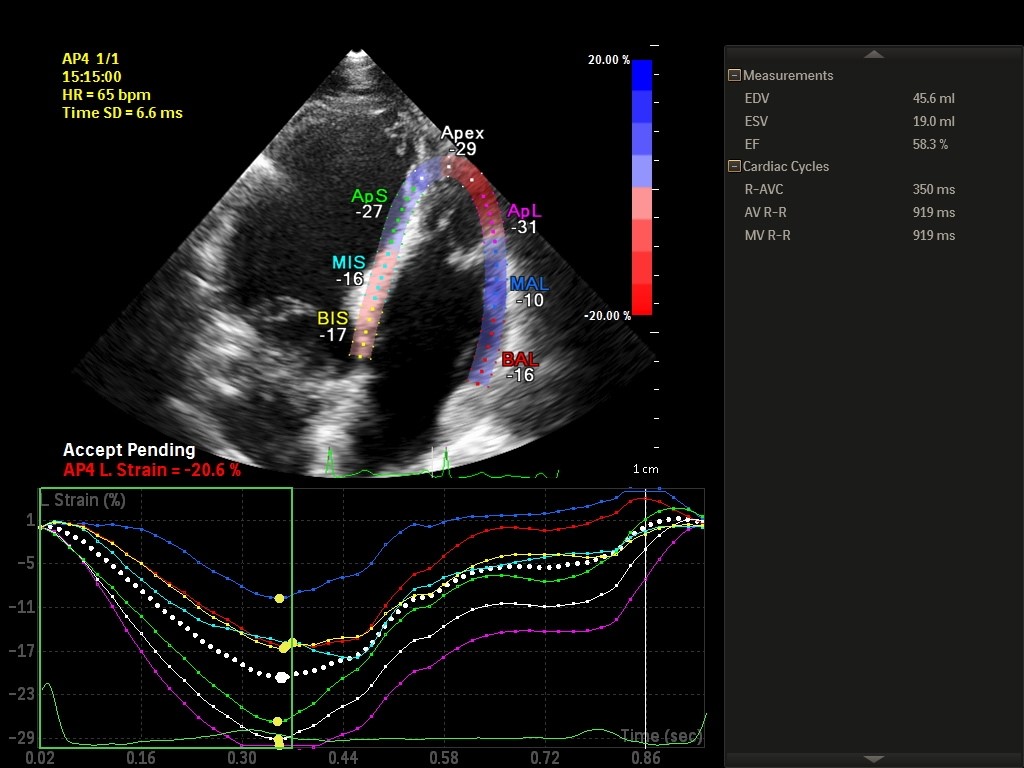
Figure 3. Right ventricular strain in a 6-segment model
The operator focuses on RV free wall at beginning of the measurement in the second model. Both models yield very similar and comparable values, but the 6-segment model is more feasible and reproducible than the 3-segment model (22). Most prominent confounders affecting RV strain are age, sex, pulmonary artery systolic pressure and minimal right atrial volume (22).RVFWS value obtained from 3-segment model is higher than 6-segment RVLS value (22). Fine et al. in their meta-analysis found a RVFWS value of −27(2)% (23). The 2015 guideline about cardiac chamber quantification reported RVFWS mean (SD) value as −29.0(4.5)% with abnormality threshold of > −20 (13). RVFWS is feasible in 88% to 94% of patients (24). The RVFWS’s coefficients of variation for intraobserver and interobserver variability were 2—7% and 3—10%, respectively (24).
Right Ventricular Strain in Cardiovascular Disease
The worsening of right ventricular strain is an early sign for RV dysfunction in many disease states even when the other traditional RV functional indices are within normal limits (25). The efficient work of RV needs appropriate coupling with pulmonary circulation and undisturbed intrinsic RV contractility. RV longitudinal strain has a correlation with ventricular-arterial coupling and arterial load but not with load-independent contractility (26).
Pulmonary hypertension is the main cause for the increased RV afterload, which decreases RV deformation. RVFWS is a significant determinant of all-cause mortality in patients with pulmonary hypertension. Patients with RVFWS ≥−19% had more than a 3-fold mortality risk compared with patients with RV LPSS <−19% (27).
Acute pulmonary embolism is associated with an abrupt increase in RV afterload. Non-survivors of acute pulmonary embolism have lower RVGLS and RVFWS values compared to survivors (28).
RVFAC and RVFWS are independent predictors of all-cause mortality, reinfarction, heart failure in patients with myocardial infarction (29). The RVFWS lower than 22.1% was associated with an adjusted hazard ratio of 2.18 for the occurrence of the composite end-point. Antoni et al. (29) also has shown that RVFWS has an incremental value over clinical information, infarct characteristics, left ventricular function, and RVFAC for the prediction of adverse outcomes in post-acute myocardial infarction patients.
Heart failure patients have subclinical RV dysfunction detected by lower RVGLS and RVFWS values (25, 30). Morris et al. (25), in their multicenter study including 208 heart failure patients with reduced ejection fraction, has reported that reduced RV strain, defined as RV global and free wall systolic strain >-17% and >-19% respectively, successfully has shown RV dysfunction despite preserved TAPSE, TDI S wave and RVFAC.
In heart failure with preserved EF (HFpEF) patients, RV dysfunction is also a frequent finding (31). RVGLS and RVFWS are more impaired in HFpEF patients compared to patients with asymptomatic left ventricular dysfunction (32).
Recently, Hamadai-Harimura et al. (33) reported that impaired RVFWS with cut-off value of ≥-13.1% was independently associated with cardiac events in acute heart failure patients. This result related to RVFWS has led to a more accurate reclassification of acute heart failure patients irrespective of their left ventricular ejection fraction status.
Right Ventricular Strain Analysis: Limitations
The RV strain imaging has limitations directly related to thinner RV wall, poor speckle tracking due to suboptimal image quality (27). Load dependency of RWFS should also not to be forgotten (18). Any increase in RV afterload also directly affects measured RWFS values.
Different software solutions coming from different vendors cause to a meaningful variability in strain measurement (34). Recent efforts to reduce inter-vendor variability would be helpful for RV deformation analysis (35). A few special software is available for RV strain analysis on the market (e.g., Epsilon Imaging EchoInsight). It is expected that more vendors will release their RV specific strain analysis software packages in the near future but there is still a long way to go.
Conclusion
The RV function should always be checked in every echocardiographic examination. A simple eyeball evaluation of the RV should be supported by other tools: RV diameters from different echo views, TAPSE, TDI S wave and RV strain imaging. All data from these echocardiographic tools should be used for reaching a conclusion about the RV function.
RV strain imaging provides early warning signs for RV dysfunction, which may be used for the implementation of appropriate therapies. Three-dimensional echocardiography including deformation data and its integration with artificial intelligence will be the next step in the RV evaluation in the future.
If RV strain analysis is going to be used in everyday echocardiography practice, we are still in need for robust clinical outcome data from large prospective trials for confirming its incremental predictive value.
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: O.B. and I.Z.A equally contributed to preparation of manuscript and fulfilled authorship criteria
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

