The effects of nutritional support for premature babies with ELBW and VLBW with hypoxic damage to the central nervous system
ORIGINAL RESEARCH ARTICLE
The effects of nutritional support for premature babies with ELBW and VLBW with hypoxic damage to the central nervous system
Article Summary
- DOI: 10.24969/hvt.2020.193
- Page(s): 45-54
- INTERNAL MEDICINE
- Published: 26/04/2020
- Received: 05/02/2020
- Revised: 01/04/2020
- Accepted: 05/04/2020
- Views: 9036
- Downloads: 7490
- Keywords: preterm infants, nutrition, extremely low body weight, neurological disorders
Address for Correspondence: Gulban M. Abdullayeva, Department of Propaedeutics of Children's Diseases, Kazakh National Medical University named after S.D. Asfendiyarov, Almaty, Kazakhstan e-mail: dm.gulban@mail.ru
Gulban M. Abdullayeva1, Shayhslam K. Batyrhanov1, Stalbek M. Akhunbaev2, Orozaly J. Uzakov2
1 Kazakh National Medical University named after S.D. Asfendiyarov, Almaty, Kazakhstan
2 International Higher School of Medicine, Bishkek, Kyrgyz Republic
Abstract
Objective: Effect of nutritional support for preterm infants with very low (VLBW) and extremely low body (ELBW) weight with hypoxic damage of the central nervous system (CNS) of varying severity is not well elucidated.
The aim of this investigation is to study clinical, laboratory, neurosonography and electroencephalography characteristics of preterm infants with VLBW and ELBW with hypoxic injury of CNS on complex comprehensive nutritional support, diagnostic criteria of which were infants body weight gain, increase in growth and head circumference.
Methods: Criteria of including into the study were VLBW and ELBW of an infant at birth and hypoxic damage to the CNS. Overall, 254 preterm infants born at the term of 23-24 weeks of gestation with body weight at birth less than 1500 grams were included into the prospective study. All patients underwent anthropometric and clinical observation of height, weight, head circumference and body mass index till 50 weeks of postconceptual age with following evaluation by central curves; standard laboratory and biochemical blood analyses, neurosonography and electroencephalography. Data analysis of further growth of observed infants after discharge from hospital was made in 2017-2019 years on the basis of studying of stationary cards.
Results: In the ELBW group with severe level of hypoxic damage to the CNS, optimum gain was 20-22 g/kg/daily, which allowed to avoid complications on the alimentary tract; in the VLBW group with severe degree it was 16-18g/kg/daily during the first three months of life. In the ELBW and VLBW groups of children with moderate degree of hypoxic damage the desired gain did not differ and was at the level of 20-25 g/kg/daily. Physiological body weight gain in infants with VLBW and ELBW according to gestational time is connected with favorable somatic and neurological prognosis in these infants. Calculation of calorie intake, selection of the type of feeding for infants with ELBW and with VLBW according to recommendations made by ESPGHAN (2010) ensures positive anthropometric data dynamics without metabolic disruptions.
Conclusion: Physiological body weight gain according to gestation period is connected with favorable somatic and neurological prognosis in these infants.
Key words: preterm infants, nutrition, extremely low body weight, neurological disorders.
Introduction
Nursing problem of preterm infants does not lose its sharpness in connection with an increase in preterm birth rate indicators during the last 20 years. From the data of Worldwide Health Organization of health protection for 2018 year in 184 countries, the amount of preterm born infants from the number of all born is from 5 to 18% (www.who.int). Therefore, it is approximately 1 million infants annually die from complications connected with preterm birth; many survivors suffer lifelong disability, often with deep defeats of nervous system (1-3). Therefore, the main task of neonatologists in the process of nursing of preterm born babies is providing not only their surviving, but also maximally possible normal development of all the functional systems of a child.
Creation of optimal conditions for normal development of preterm born infants traditionally is connected with the organization of feeding and type of nursing in connection with their high vulnerability and severity of their state at birth, especially in infants with extremely low body weight (ELBW) and with very low body weight (VLBW). Data of numerous investigations show that preferable starting product of enteral nutrition is breast milk in connection with less frequency of intolerance in these babies. However, the main problem of nursing is not only in morpho-functional immaturity of preterm infant (respiratory disturbance, weakening of suction and swallowing, weak intestinal motility and other), but in declining of the main nutrients of breast milk during process of its "ripening", which is the predictor of the development of hypoglycemia and hypoproteinemia in infants (4). Nutrient deficiency (of energy, albumin, mineral composition of breast milk or mixtures) during the first three months of life, and according to some data (5), even in the first day of life results in growth retardation, and as a result provokes severe changes in the central nervous system (CNS), that are not compensated by good nutrition established in the subsequent period of life.
Since 2010 year specialists in perinatal centers of Kazakhstan have been developing recommendations on composition and quantity of food substances, necessary for preterm infants, in order to achieve optimal indicators of physical development and satisfactory functional parameters based on guidance of the European Society on Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN, 2010) - "Enteral nutrition of premature newborn babies" (6). Requirements in nutrients and microelements of preterm infants beginning from their birth to 2-3 weeks of life gradually increase. At partial and full enteral feeding, energy requirement is 110-135 kcal/kg/day, which as a rule, is achieved to 6-8th day of life (7, 8). Separate descriptions of feeding of preterm infants with the body weight of 1000-1800 are observed in following limits: daily necessity in albumin is 3.5-4.0 g/kg (at body weight < 1kg - 4-4.5g/kg); necessity in fats – 4.8-6.6 g/kg/daily; necessity in carbohydrates 11.6-13.2 g/kg/daily (9, 10). However, these recommended descriptions of preterm infants nursing in every separate cases are specified and adjusted according to weight, organism maturity and identified health issues.
Thus, characteristics of nutritional support for preterm infants, providing energy requirements of the organism as they grow become a starting point in babies nursing with ELBW and VLBW and the main condition in stopping pathologies in growth, including neurological pathologies.
In 2008 in the territory of Kazakhstan international criteria of live birth and stillbirth recommended by the WHO protection were accepted (Order MH RK from the 1st of December 2007 №746 ("About regionalization of prenatal help in the Republic of Kazakhstan", www.egov.kz). Introduction of these criteria leading to the reorganization of the system of obstetric care and of childhood in a whole, found a reflection in developing and active introduction of the programs "Hospitals of friendly attitude to a baby", "Effective perinatal care", "Integrated conduction of illnesses of child's age", which provided high survivability of preterm infants with low and extremely low body weight.
Therefore, from data www.medinfo.kz in 2017 survival in the group of children with body weight at birth - 500-999 grams was 96.66%. However, increasing in survival led to simultaneous growth of a number of complications in preterm infants, connected with severity of antenatal hypoxic damage and postnatal development of albumin and energy insufficiency. One of the indicators of prematurity of children in Kazakhstan is a neurological pathology, which shows progressive increase in frequency - 80% cases organ disorders of CNS (11). Different forms of hydro- and microcephalus combined with development of motor function delays (forming and/or formed cerebral palsy), epileptic syndromes of early childhood are related to the latter.
The aim of this investigation is to study clinical, laboratory and neurosonography and electroencephalography characteristics of preterm infants with VLBW and ELBW with hypoxic of CNS on complex comprehensive nutritional support, diagnostic criteria of which were infants body weight gain, increase in growth and head circumference.
Methods
Study design and population
Design of the study is observational and prospective.
The study was conducted at the Obstetric Hospital and at the departments of perinatal (CP – Center for Perinatology, Almaty city) and neonatal (CPPCS – Center for Perinatology and Pediatric Cardiac Surgery, Almaty city) centers of the Children`s City Clinical Hospital (CCCH №2), Almaty city, Kazakhstan between 2016 and 2018. All premature babies were nursing in the chambers of joint stay “Mother and child“ and did not need intensive and resuscitation care.
The sample consisted of 254 preterm infants who experienced hypoxic damage to the CNS in perinatal period that caused the formation of a neurological pathology. Criteria of including into the study were VLBW and ELBW of an infant at birth and hypoxic damage to the CNS. Preterm infants born at the term of 23-24 weeks of gestation with body weight at birth less than 1500 grams were included into the main sample. Criteria for exclusion from the sample were: 1) low birth weight of a full-term baby; 2) phenotypic signs of chromosomal abnormalities confirmed by karyotyping; 3) malformations and heredity diseases identified during the examination; 4) refusal of parents of a premature baby to participate in this investigation.
Informed consent of parents, legal representatives of a child, to use for scientific purposes clinical, laboratory, and instrumental data was obtained.
Clinical, laboratory, and neurological examinations
According to clinical protocols for data collection, we conducted collection of anamnesis data - obstetric and gynecological anamnesis and somatic health of mother, analysis of pregnancy and maternity, analysis of adaptation period of an infant.
Clinical observation of an infant was made for informed choice of nutritional support and for calculation of food composition to meet growing needs of infants in certain nutrients.
Adequacy of individually selected nutrition was estimated by everyday gain in body weight, measured by electronic scales (12). This indicator was supplemented by head circumference and the length of the infant, weekly measured with sufficient accuracy with a centimeter tape. Generalized indicator of a child development (BMI - body mass index) was calculated according to the formula: BMI = body weight (g)/ height (cm) proposed by A. Quetelet in 1835 (13). Body weight, height and head circumference measurements after birth were correlated with the parameters of expected changes appropriate to gestational term, which allowed us to build a growth curve describing the condition of a child. To assess growth and weight gain we used centile curves of fetus growth and of preterm infant developed by Fenton et al. (14). These curves include the period of post conceptual age from 22 weeks of gestation and till 50 weeks when the most of preterm infants are discharged from hospital. For weight category correction of preterm born infants in the range from 10 to 90 percentile, in which there are about 80% preterm born infants with the average development level, we conducted: calculation of nutrition calorie, calculation of suckling tempo and belching moments, everyday measurement of a child`s body weight to control body weight gain.
Standard laboratory analysis of total blood count, biochemical blood analysis (total protein, glucose, total bilirubin with fractions, electrolytes (Na+, K+, Ca++, Cl-), alkaline phosphatase and urea were performed in all patients.
All preterm infants underwent evaluation by specialists - neurologist, pediatrician, infectious disease specialist and ophthalmologist upon admission and discharge.
Degree of damage to the CNS was ascertained upon admission to the department from medical records according to ICD -10 revision (International Classification of Diseases -10 revision). All patients underwent neurosonography (NSG) and electroencephalography (EEG).
Hospital discharge criteria were improving of overall condition, stabilization of neurological status, adequate thermoregulation, and positive weight dynamics - achievement of body weight not less than 2000 grams.
Nutritional support
Nutritional support was based on recommendation of the European Society on Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN, 2010) - "Enteral nutrition of premature newborn babies" (6).
Follow-up
Prospective observation of growth and development of children till one year of corrected age was conducted in the follow-up rooms. Analysis of data of further growth of observed infants after discharge from hospital was made in 2017-2019 years on the basis of studying of ambulatory cards f.112/y at the follow-up rooms of perinatal (CP, Almaty city) and neonatal (CPPCS, Almaty city) centers.
Statistical analysis
Statistical analysis of research results was made by SPSS Inc 19.0 (New York, USA) software. Data are presented as number and proportion, mean and standard error. Comparison of continuous variables on admission and discharge was made using paired t test, categorical variables – Chi-square test. The significance level was set – p<0.05
Results and discussion
Overall, 116 (45.7%) boys and 138 (54.3%) girls were included in the study (Table 1). For children in the group with ELBW, more severe forms CNS damage were characteristic (>57%), whereas in the group of babies with VLBW, severe degree of damage to the CNS was detected in 40% of infants, moderate degree - 46%. All anthropometric data were included in the table before the start of the correction of nutritional support.
|
Table 1. Clinical characteristics of preterm infants included in the study |
||||
|
Variable |
Preterm infants |
|||
|
ELBW |
VLBW |
Total |
||
|
Number of infants, n (%) |
66 (26) |
188 (74) |
254 |
|
|
Girls, n (%) |
42 (63.6) |
96 (51.1) |
138 |
|
|
Boys, n (%) |
24 (36.4) |
92 (48.9) |
116 |
|
|
Gestation age at birth, weeks |
23-27 |
28-34 |
23-34 |
|
|
Hypoxic damage to the CNS in perinatal period according to patient records, % |
100 |
100 |
100 |
|
|
Degree of severity, n (%) |
mild - Р 91.0; Р 91.2; Р 91.4 |
0 |
25 (13.3) |
25 (9.8) |
|
moderate - Р 52.0; Р 52.5; Р 52.1 |
28 (42.4) |
87 (46.3) |
115 (45.3) |
|
|
severe - Р 21.9; Р 91.1; Р 91.2; Р 91.5; Р 91.8; Р 52.1; Р 52.9 |
38 (57.6) |
76 (40,4) |
114 (44.9) |
|
|
Body weight at birth, g |
916 (73.9) |
1473 (117) |
|
|
|
Body length at birth, cm |
33.3 (1.1) |
38.9 (1.6) |
||
|
Head circumference, cm |
26.3 (0.7) |
28.1 (1.1) |
||
|
Body mass index |
10.2 (0.5) |
11.8 (0.8) |
||
|
ELBW – extremely low birth weight, CNS – central nervous system, VLBW – very low birth weight |
||||
Total number of children with ELBW and VLBW were distributed by type of feeding as follows: 13.78% cases (35) were on exclusively breastfeeding, 7.87% (20) received breast milk with fortification, 52.76% children (134) on mixed feeding and 25.59% children (65) were on artificial feeding.
Analysis of antenatal growth of observed infants showed that all mothers experienced complicated pregnancy and childbirth (Table 2). The most often found pregnancy pathology were fetoplacental insufficiency (FPI) and threat of pregnancy discontinuation in 100% of cases, chronic fetus hypoxia (ChFH) - 92.52%, severe respiratory infections - 53.94%, sexually transmitted infections - 53.54%, pyelonephritis -32.68%, abundance of water – 13.78%. Ten infants (3.94%) were born by the technology of extracorporeal impregnation, nine (3.54) - in multiple pregnancy (8 twins). 110 (43.31%) infants were delivered by scheduled and emergent Caesarean operations in severe condition.
Evaluation by Apgar scale at birth at the first minute varied from 2 to 8 points (5.6(1.4)). Overall, 225 infants were born in asphyxia (88.58%). Resuscitation methods were conducted due to the clinical protocol of MH RK; artificial ventilation of lungs (AVL) with endotracheal installation of surfactant was conducted in 254 infants (96.46%), duration of AVL at average was 18 days (15.3(2.9) days) (Table 2).
|
Table 2. Structure of the pregnancy pathology of mothers with preterm infants |
|||
|
Variables |
ELBW (n=66) |
VLBW (n=188) |
Total (n=254) |
|
n (%) |
n(%) |
||
|
Fetoplacental insufficiency |
100 |
100 |
100% |
|
Chronic hypoxia of fetus |
63 (95.5) |
172 (91.5) |
235 |
|
Threat of pregnancy discontinuation |
100 |
100 |
100% |
|
Severe respiratory infections |
39 (59.1) |
98 (52.3) |
137 |
|
Sexually transmitted infections |
43 (65.1) |
93 (49.5) |
136 |
|
Pyelonephritis |
26 (39.4) |
57 (30.3) |
83 |
|
Polyhydramnios |
11 (16.7) |
24 (12.8) |
35 |
|
Evaluation by Apgar scale |
5.5 (2; 7) |
4.7 (2; 8) |
5.6 (2; 8) |
|
AVL + surfactant |
100 |
179 (95.2) |
245 |
|
AVL, artificial ventilation of lungs, ELBW – extremely low birth weight, VLBW – very low birth weight |
|||
According to the results of consultations by profile specialists the following clinical diagnosis were established (Table 3). In assessing of neurological status the most newborn infants had dominant syndrome of CNS depression -102 (40.16%) followed by syndrome of hyperexcitability - 82 (32.38%), hypertensive and hydrocerphalic - 26 (10.24%), and also the formation of cysts in peri- and intraventicular region - 16 (6.3%). Only 10.63% of examined infants had combination of several syndromes.
|
Table 3. Morbidity pattern of infants group investigated according to ICD-X |
|||
|
Diagnosis (main) |
ELBW (n=66) |
VLBW (n=188) |
Total |
|
n (%) |
n (%) |
||
|
Hypoxic and ischemia encephalopathy transient: G 91.9; G0.9; F 90.1; F 82; F 84; R 56.0; R 56.8. |
0 |
82 (43.62) |
82 |
|
Hypoxic and posthemorrhagic encephalopathy transient: G 91; G 91.0; G 91.1; G 91.2; G 91.8; G 91.9 |
45 (68.18) |
57 (30.32) |
102 |
|
Posthypoxic and posthemorrhagic damage of CNS persistent(organic): F 06.9;G80.0-G 8.9; G4O-G40.9; G41-G41.9 |
21 (31.82) |
49 (20.06) |
70 |
|
Respiratory distress syndrome with outcome in bilateral pneumonia and bronchopulmonary dysplasia |
54 (81.82) |
25 (13.3) |
79 |
|
Preterm anemia |
66 (100) |
104 (55.32) |
170 |
|
Rickets |
29 (43.94) |
18 (9.57) |
47 |
|
Inguinal and umbilical hernia |
15 (22.73) |
22 (11.7) |
37 |
|
Preterm retinopathy of the I-II degrees |
12 (18.18) |
143 (76.06) |
165 |
|
Preterm retinopathy of the III degree |
48 (72.73) |
31 (16.49) |
79 |
|
Specific infection for perinatal period |
60 (90.91) |
132 (70.2) |
192 |
|
ELBW – extremely low birth weight, VLBW – very low birth weight |
|||
In 200 children (78.74%) the main neurological pathology was complicated by bronchopulmonary dysplasia in 31.1%, by preterm anemia in 66.93%, by rickets in 18.5%) and also inguinal and umbilical hernias were noted in 14.5% of children. Retinopathy I-II degrees was found in 64.96% and of the III degree -31.1% cases. Infectious diseases were represented by persistence of cytomegalovirus and herpes simplex virus infection in 75.59% of cases, but in most cases without realization into generalized process, only in 13 cases (5.12%), specific antivirus treatment was carried out. Complications of the main illness and accompanying pathology worsened general condition of children and caused prolonged treatment and negatively affected the prognosis.
Hemogram indicators of preterm infants with hypoxic damage during the period of the neonatality differ in essential features. According to the presented data, the disturbances of the ratio of the composite of blood elements were noted upon admission in the vast majority of premature babies with ELBW and VLBW.
In both groups, anemia of moderate severity was revealed and in the VLBW group, it had a pronounced regenerative character. Hyporegenerative anemia of mild degree was noted in the ELBW group. It is necessary to note that changes in red blood counts were observed without correction with antianemic drugs and was achieved through careful selection of nutritional support.
|
Table 4. Differences in hemogram indices of preterm infants upon admission and discharge from the hospital |
||||||
|
Variables |
ELBW |
VLBW |
||||
|
Up on admission |
Up on discharge |
p |
Up on admission |
Up on discharge |
p |
|
|
Hemoglobin, g/L |
152.9(3.01) |
148.1(2.11) |
|
103.7(3.88) |
161.0(3.58) |
<0.05 |
|
Erythrocytes, 1012/ L |
4.3(0.05) |
4.1(0.02) |
|
3.2(0.01) |
5.7 ( 0.08) |
<0.05 |
|
White blood cells, 109/ L |
6.30(0.71) |
11.07(0.84) |
<0.01 |
3.91(0.62) |
9.72(0.14) |
<0.01 |
|
Neutrophils, 109/ L |
5.01(0.26) |
4.77(0.16) |
|
2.11(0.19) |
3.35(0.15) |
<0.05 |
|
Monocytes, 109/ L |
2.64(0.06) |
1.62(0.40) |
<0.05 |
1.33(0.22) |
1.48(0.08) |
|
|
Lymphocytes, 109/ L |
3.53(0.25) |
5.14(0.71) |
<0.05 |
1.47(0.48) |
4.20(0.31) |
<0.01 |
|
Eosinophils, 109/ L |
0.31(0.01) |
0.45(0.01) |
|
0.20(0.04) |
0.36 ( 0.08) |
|
|
Total protein, g/ L |
31.5(5.9) |
61.4(4.2) |
<0.01 |
52.9(4.3) |
72.5(6.5) |
<0.05 |
|
Albumin, g/ L |
35(0.9) |
44(1.1) |
<0.05 |
36(0.6) |
49(1.5) |
<0.05 |
|
Total bilirubin, mmol/ L |
205(41.6) |
86(10.8) |
<0.01 |
197(28.8) |
68(4.6) |
<0.01 |
|
Urea, mmol/ L |
2.5(0.3) |
4.4(0.6) |
<0.05 |
3.7(0.4) |
5.8(0.8) |
<0.05 |
|
Glucose, mmol/ L |
2.3(0.9) |
5.7(1.4) |
<0.01 |
4.2(1.5) |
6.4(1.7) |
<0.05 |
|
ELBW – extremely low birth weight, VLBW – very low birth weight |
||||||
All observed preterm infants admitted to the hospital revealed a large variation in the values of white blood counts. Leukopoiesis state in separate types of perinatal pathology in preterm infants had distinctive signs. So, change of leucopenia upon admission to moderate leukocytosis was observed in preterm infants with ELBW, without clinical manifestations of infection. Overall, 81% of preterm infants had pronounced leucopenia.
Low values of phagocytic system indices were registered upon admission in the group with VLBW: polynuclear neutrophilic granulocytes, monocytes, which were combined with general reduced orientation of hemostasis. The absolute neutrophils count in each group with ELBW is almost similar, as well as upon admission and after discharge. Nevertheless, in each group there were preterm babies with neutropenia and neutrophilia, which is obviously associated with different gestation age of children. Monocytosis in the analysis of blood of premature infants at admission was three times more common than at discharge. Such changes in the parameters of the elements of the blood count, apparently, reflects a change in the type of hemoglobin, and also complications of the postnatal period associated with the immaturity of the myeloid and lymphoid sprouts of the brain. According to Menon et al. and Subramanian et al. , such changes in the quantitative composition of blood cells may reflect stimulation of precursors in the bone marrow by proinflammatory cytokines in the context of the addition of complications of hypoxic and inflammatory genesis (15, 16).
It should be noted that all children were characterized by severe bilirubinemia upon admission with background hypoproteinemia. Hypoglycemia in blood is explained by defects in feeding. Low values urea (less than 1.5-2.5 mmol/L) may indicate protein deficiency. Albumin level for evaluation of a nutritional status is less specific in preterm infants, however, its indicators less than 30-35 g/L with a low urea confirmed a pronounced deficiency in protein supplementation. Therefore, our attention in breastfeeding was paid on protein subsidies. Therefore, all changes in blood counts were associated with nutritional correction in each case taking into account the gestational age of the child and the severity of the disease of the CNS.
Comparative analysis of bioelectric activity data and echographic structure of the brain upon admission and upon discharge allow us to evaluate the adequacy of therapy (17). The study of NSG in 254 children revealed structural changes in peri- and intraventricular zones of the ventricular system of the brain and white matter intraventricular hemorrhage (IVH) of the I degree – in 82 (32.28%), IVH of the II degree – in 102 (40.16%), IVH of the III degree – in 70 (27.56%), IVH of the IV degree – in 79 (31.1%); and periventricular brushes were detected in 9 (10.98%), periventricular leukomalacia (PVL) – in 47 (18.52%), and porencephaly – in 37 (14.4%). In 19 (28.79%) of the examined children, the damage was bilateral in nature; in 14 (21.21%) a combination of a disturbances of the structure of the brain tissue, (PVL, periventricular brushes and others) and hemorrhagic damage (IVH) of various degrees were noted. The average duration of treatment for children of this group was 26(4) days (Table 5).
|
Table 5. Results of the instrumental examination of the brain of children |
|||
|
Variables |
ELBW (n=66) |
VLBW (n=188) |
Total (n = 254) |
|
Neurosonography |
|||
|
IVH I degree, n(%) |
0 |
82 (43.62) |
82 (32.28) |
|
IVH II degree, without ventriculodilation, n(%) |
45 (68.18) |
57 (30.32) |
102 (40.16) |
|
IVH III degree with ventriculodilation, n(%) |
21 (31.82) |
49 (26.06) |
70 (27.56) |
|
IVH IV degree (spread to the parenchyma of the brain), n(%) |
54 (81.82) |
25 (13.3) |
79 (31.1) |
|
Peri- and intraventricular brushes, n(%) |
66 (100) |
104 (55.32) |
170 (66.93) |
|
Periventricular leukomalacia, n(%) |
29 (43.94) |
18 (9.57) |
47 (18.52) |
|
Porencephaly, n(%) |
15 (22.73) |
22 (11.7) |
37 (14.57) |
|
Electroencephalography |
|||
|
Decrease in the amplitude and frequency of brain activity, n(%) |
42 (63.64) |
143 (76.06) |
185 (72.83) |
|
Paroxysmal curve with peak wave frequency 1,5-2 Hertz, n(%) |
48 (72.73) |
31 (16.49) |
79 (31.1) |
|
Periodic curve with multi-focal or focal sharp waves, n(%) |
56 (84.85) |
32 (17.2) |
88 (34.65) |
|
Periodic curve with rare flashes of activity and a sharp decline in amplitude, n(%) |
2 (3.03) |
3 (1.6) |
5 (1.97) |
|
Isoelectric line, n(%) |
1 (1.52) |
0 |
1 (0.39) |
|
ELBW – extremely low birth weight, IVH - intraventricular hemorrhage, VLBW – very low birth weight |
|||
Dynamic EEG studies in preterm infants to assess the functional state of the brain were undertaken in the acute period and at the time of discharge, we failed to get similar data at the time of discharge due to the fact that with clinical improvement in neurological status this diagnostic test is not recommended. This is due to the fact that changes in the basal activity of the encephalogram of premature infant in the acute stage of the disease for hypoxic damage are largely non-specific and reflect only the severity of brain dysfunction. A comparison of the slice EEG of the brain in a small sample of children with ELBW (9 – 13.6%) and children with VLBW (47 – 24.46%) showed that these data do not give visible changes that could be linked to overall improvement in the condition of the child at the time of discharge which is consistent with the literature. So, Palchik (17), believes that in order to obtain an informative picture of the changes that have taken place, a longer observation period is needed and a diagnostic EEG should be carried out once in three months.
Upon admission, all children included in the surveyed group were characterized by a pronounced deficiency of body weight in relation to corrected age (Table 1). In this case, due to parameter “type of feeding” the sample was divided into four groups unequal in the number of children. The bulk of children -134 infants - were on mixed feeding (breast (milk mixture), 65 infants – on artificial feeding and 20 infants received breast milk with fortification. Diagnostic criteria for the adequacy of nutritional support leading to growth and development of infants with ELBW and VLBW against the background of hypoxic damage to the CNS of different severity were body weight gain, increase of indicators of growth and head circumference.
Achievement by a child of anthropometric parameters corresponding to gestational age is associated with a phenomenon of catching-up growth that occurs after the stabilization due to neurological status in preterm born infants. According to Ivanova et al. (18), the maximum favorable thing for the further development is growth spurt during the first 2 months of the corrected age. In a number of publications Volodin et al. (19, 20) indicated that children gradually caught – up their centile corridor to 6-9 months of corrected age have the best neuropsychic development, in comparison with those who did not reach the demanded indicators of body weight and growth.
Rate of increase depended on the whole complex of conditions: maintenance of dose and feeding schedule; lessening of invasive procedures; full sleep; regulation of sleep and wakefulness. It should be underlined that with different difficulty degrees of neurological symptom, nutritional correction was needed for every baby, taking into account his individual peculiarities. So, in the ELBW group with severe level of hypoxic damage to the CNS optimum gain was 20-22 g/kg/daily, which allowed to avoid complications of the alimentary tract, in the VLBW group with severe degree such loading was not tolerated and at an average it was 16-18g/kg/daily during the first three months of life. For all that, in the ELBW and VLBW groups of children with moderate degree of hypoxic damage the desired gain did not differ and was at the level of 20-25 g/kg/daily (Table 6).
|
Table 6. Centiles of growth curves by T.R. Fenton (2013) of children of ELBW and VLBW groups with different degrees of severity at admission and at discharge from the hospital (n=254) |
|||||||
|
|
Severity degree of condition (n) |
||||||
|
ELBW (n=66) |
Mild (n=0) |
Moderate (n=45) |
Severe (n=21) |
||||
|
Upon admission |
Upon discharge |
Upon admission |
Upon discharge |
Upon admission |
Upon discharge |
||
|
Weight, gram |
- |
- |
3-5 |
8-12 |
3-5 |
5-8 |
|
|
Height, cm |
- |
- |
7-10 |
10-15 |
7-8 |
8-10 |
|
|
Head circumference, cm |
- |
- |
10-30 |
30-45 |
10-30 |
30-45 |
|
|
BMI |
- |
- |
11,1 (10; 12) |
12,8 (11; 14) |
11,1 (10; 12) |
12,8 (11; 14) |
|
|
Gain, g/kg/daily |
- |
20-25 |
20-22 |
||||
|
VLBW (n=188) |
Mild(n=82) |
Moderate(n=57) |
Severe (n=49) |
||||
|
Upon admission |
Upon discharge |
Upon admission |
Upon discharge |
Upon admission |
Upon discharge |
||
|
Weight, gram |
35-45 |
50-65 |
25-35 |
40-45 |
20-25 |
35-42 |
|
|
Height, cm |
30-45 |
50-55 |
20-25 |
40-45 |
20-25 |
35-40 |
|
|
Head circumference, cm |
47-50 |
50-52 |
42-45 |
50-52 |
37-45 |
40-48 |
|
|
BMI |
13.7 (12; 16) |
16.2 (13; 17) |
11.8 (12;14) |
13.4 (12; 15) |
11.7 (10;14) |
12.5 (11; 17) |
|
|
Gain, g/kg/daily |
15-20 |
20-25 |
16-18 |
||||
|
BMI – body mass index, ELBW – extremely low birth weight, VLBW – very low birth weight |
|||||||
The results of the correlation analysis (r – Spearman coefficient) indicate that in the group of infants with ELBW weight, height and head circumference indicators are not related, but there is a significant correlation between weight and head circumference (r=0.828; p=0.003) at the time of discharge. In the group of infants with VLBW weight and height are correlated at birth (r=0.775; p=0.008), as well as at the time of discharge - correlation of weight and height (r=0.723; p=0.018), height and head circumference (r=0.753; p=0.012), which in part may speak of cumulative changes in the development of the infant`s organism.
Individual selection of food, taking into account the peculiarities of infant`s nutritional behavior, was carried out with an orientation towards weight gain, correlating with anthropometric data indicators not exceeding 10-90 corresponding centile (14).
Compliance with this condition was accompanied by a decrease in the severity of neurological symptoms in both groups. Manifestations of symptoms of severe forms of diseases of the CNS in the group of infants with ELBW who gained weight according to gestational age due to individual selection of diet and regimen of feeding decreased from 57% to 31.8%. A similar pattern was observed in the group of infants with VLBW of severe forms. Their condition after correction of nutritional behavior and calculation of adequate caloric intake improved to moderate and mild degrees, and the number of infants in this group reduced to 20.06% (Table 1 and Table 3).
The required dynamics of therapeutic weight gain with improved symptoms was observed in groups of infants who were on artificial feeding and breastfeeding with fortification. Ensuring such dynamics in groups of infants with mixed feeding and breast milk required a longer correction of the weight curve due to persistent hypoglycemia and hypoproteinemia. A significant improvement in the condition of children at discharge should be noted.
Calculation of calorie intake, regimen and type of feeding for each child provided an adequate nutritional support. In particular, this resulted in a stable and expected increase in body weight and an increase in BMI according to the centile range of the growth curve as for boys, so as for girls (14). Correspondence of anthropometric measurements to the gestational age provided stabilization of neurological status and reduction in the severity of hypoxic lesions of the CNS at discharge (Fig. 1).
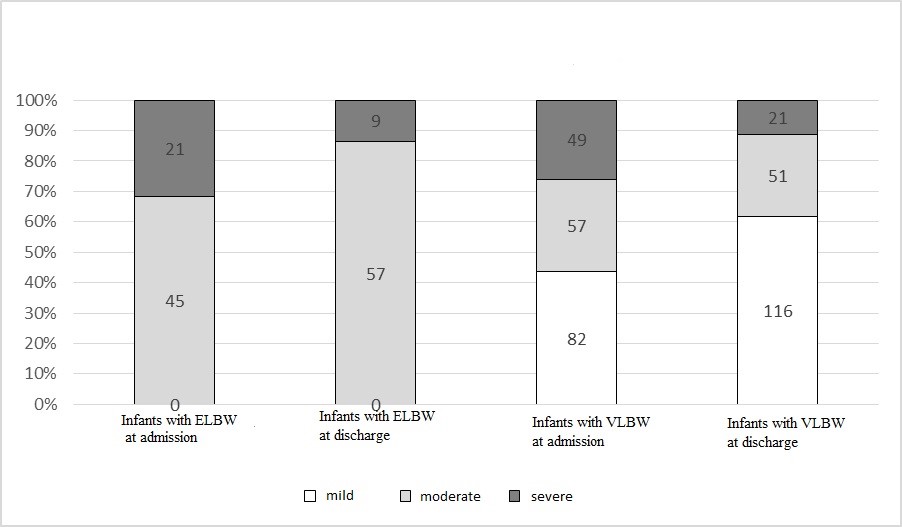
Figure 1. Assessment of the severity of the hypoxic disorders of children upon admission and upon discharge from the hospital. ELBW – extremely low birth weight, VLBW – very low birth weight
The data presented indicate that 78 (30.71%) children of the study group after discharge from the CCCH №2 for two years received a specialized assistance and took part in the programs of neurological rehabilitation at the offices of follow up. These children showed a healthy and progressive physiological and psychomotor development despite a burdened history of birth. Therefore, the issue of individual selection of type and regimen of feeding of preterm infants for the prevention of severe cerebral disorders remains relevant.Limitations of the study
The detected effects of nutritional support are associated in our research with a sample of only preterm infants. The examination of nutritional problems of full-term babies who were born with low body weight is in need of a further study.
Conclusions
Results of comprehensive evaluation of infants with ELBW and VLBW and hypoxic damage of CNS of different severity on different types of feeding lead to conclusions:
1. Deep gestational immaturity combined with hypoxic damage to the CNS cause formation of stable metabolic disorders and, as a result, leads to severe cerebral damage with unfavorable outcome. To prevent such complication it is necessary to observe and achieve daily weight gain for children with ELBW to 20-22 g/kg/daily, in the group with VLBW to 16-18 g/kg/daily.
2. The results of our observation confirm the data of other studies, aimed at searching predictors and conditions for ensuring the quality of life of preterm infants. Therefore, physiological body weight gain in infants with VLBW and ELBW according to gestational time is associated with favorable somatic and neurological prognosis if weight and head circumference are in the range above 10 or below 90 percentile according the growth curve by Fenton et al. (14).
3. Calculation of calorie intake, selection of the type and rate of feeding for infants with ELBW and with VLBW according to recommendations made by ESPGHAN (2010), which is 110-135 kcal/kg/daily in our investigation provided positive anthropometric data dynamics without metabolic disruptions.
4. In preterm infants with different gestational age in case of hypoxic damage to the CNS in the neonatal period significant changes in hemogram are noted, which are characterized by a large variety and indicate pronounced shifts in hematopoiesis, incomplete formation of the marrow bone barrier, the permeability of which was increased for young, immature cells, including the соnditions of pathology. These hemogram changes reflect a deep hypoxic damage.
5. The data obtained allows us to demonstrate pronounced differences supported by neurosonography between the infants with ELBW and VLBW at birth, the latter may retain transitory not permanent disturbances until full compensation for neurological deviations in the first year of life. To obtain a detailed picture of changes in the structure of the brain and its bioelectric activity longer period of observation is required.
Organizing the right, individually tailored nutritional support is one of the important tasks, solved at the first and second stages of nursing of preterm newborns. An important indicator of the adequacy of nutritional support accepted by all specialists is everyday weight gain, closed to intrauterine fetal growth rate.
Peer-review: External
Conflict of interest: None to declare
Authorship: G.M.A., Sh.K.B., S.M.A., and O.J.U.are equally contributed the study and preparation of article
Acknowledgments and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

