Types and Structure of Complications, and Causes of Mortality with Different Combinations of Immunosuppressants in Patients of Undergoing Organ Transplantation
BRIEF REPORT
Types and Structure of Complications, and Causes of Mortality with Different Combinations of Immunosuppressants in Patients of Undergoing Organ Transplantation
Article Summary
- DOI: 10.24969/hvt.2017.21
- Page(s): 61-64
- Transplantation
- Published: 10/09/2017
- Received: 23/08/2017
- Revised: 28/08/2017
- Accepted: 10/09/2017
- Views: 9896
- Downloads: 8740
- Keywords: kidney transplantation, liver transplantation, immunosuppression therapy, survival
Address for Correspondence: Janybek Gaibyldaev,
SRI of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan, E-mail: janybek_86@mail.ru
Authors
Scientific Research Institute of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan
Abstract
We aimed to retrospectively analyze morbidity and mortality in recipients of kidney and liver transplant receiving immunosuppressive therapy (tacrolimus and cyclosporine with mycophenolate mofetil and mycophenolic acid). Overall, 228 patients who underwent kidney and liver transplantation were included in the study. The overall graft survival of patients who underwent kidney and liver transplantation from 1999 to 2017 was 84.2%. Combinations including cyclosporine, were associated with high rate of complications acute rejection, CMV and candida infections as compared to tacrolimus. The most unfavorable in terms of mortality was combination of cyclosporine – mycophenolate mofetil.
One of the important problems of modern transplantology is the creation of combination of immunosuppressants having the lowest possible toxic effects on the body of the recipient. The most frequent variety of infectious complications, sometimes reaching to sepsis and lethal outcome in patients receiving immunosuppressants (1-10).
Many modern immunosuppressants effectively suppress the immune system of recipients after transplantation of vital organs, but also affect other organs, causing hypo-and aplasia of the bone marrow with the progress of agranulocytosis (7-10).
In remote period in patients receiving immunosuppressants, carcinogenic and teratogenic side effects may develop (7-11).
All these factors force to seek new combinations of immunosuppressants in dosages that provide sufficient suppressive effect, avoiding toxic effects. The most common cause of reduced graft function and occasionally recipients’ mortality during the first year after transplantation is infection, especially cytomegalovirus infection (CMV). Cytomegalovirus infection may be primary and associated with the reactivation of the virus in a recipient with positive results of serological tests as a consequence of immunosuppressive therapy. Approximately 90% of patients are able to cope with infection, and they do not have any symptoms, but in 5-10 % of cases, it leads to death (7-10).
There are studies on outcomes and side effects of immunosuppressive therapy in kidney and liver transplant patients with new combinations of immunosuppressant therapies (11-16), however short-term and long-term effects of combinations of immunosuppressive therapy (tacrolimus and cyclosporine with mycophenolate mofetil and mycophenolic acid) on morbidity and mortality after kidney and liver transplantation need further investigation.
We aimed to retrospectively analyze and present preliminary results on the effects of immunosuppressive therapy (tacrolimus and cyclosporine with mycophenolate mofetil and mycophenolic acid) on morbidity and mortality after kidney and liver transplantation in cohort of patients being followed-up at our institution.
We retrospectively analyzed records of 228 patients who underwent organ (kidney - 178 and liver – 50) transplantation between 1999 and 2017, received immunosuppression therapy and have been followed up in our clinic.
The following data were collected: type of immunosuppressive therapy, proportion of acute rejection, overdose, cytomegalovirus and candidiasis infections, and mortality, countries where patients underwent kidney transplantation and rate of return to hemodialysis. Survival analysis was based on 1-5-10 -year follow-up data.
Statistical analysis was performed using Chi-square test to compare proportions.
Table 1 reflects a different combination of immunosuppressants that were received by patients after organ transplantation. Of these, 51.3% received the combination of tacrolimus - mycophenolate mofetil, 28% - tacrolimus - mycophenolic acid, 15% - cyclosporine – mycophenolate mofetil, and 6% - cyclosporine - mycophenolic acid.
|
Table 1. Types of immunosuppressive therapy |
|
|
Types of immunosuppressive therapy |
% |
|
Tacrolimus – Mycophenolate mofetil |
51.3 |
|
Tacrolimus - Mycophenolic acid |
28 |
|
Cyclosporine - Mycophenolate mofetil |
15 |
|
Cyclosporine - Mycophenolic acid |
6 |
|
Table 2. Analysis of complications of different combinations of immunosuppression
|
||||||
|
Immunosuppressant’s induction |
Number of patients, n(%) |
Acute rejection, n(%) |
Overdose, n(%) |
Cytomegalovirus infection, n(%) |
Candidiasis, n(%) |
Mortality, n(%) |
|
Tacrolimus, Mycophenolate mofetil |
117(51.3) |
5(4.0) |
5(4.0) |
9(7.7) |
3(1.3) |
5(2.2) |
|
Cyclosporine A, Mycophenolate mofetil |
35(15) |
3(8.5) |
3(8.5) |
6(17.1) |
2(5.7) |
5(14.3) |
|
Tacrolimus, Mycophenolic acid |
62(28.0) |
3(4.8) |
2(3.2) |
7(11.3) |
5(8.1) |
1(1.6) |
|
Cyclosporine A, Mycophenolic acid |
14(6.0) |
2(14.2) |
1(7.1) |
1(7.1) |
- |
- |
|
Total |
228 |
14(6.1) |
11(4.8) |
23(10.1) |
10(4.4) |
11(4.8) |
The table 2 shows the causes of complications in different combinations of immunosuppressants. Complications were common in combination of cyclosporine and mycophenolate mofetil, and mortality was 14.3%. Analysis results are also clearly shown in the Figure 1.
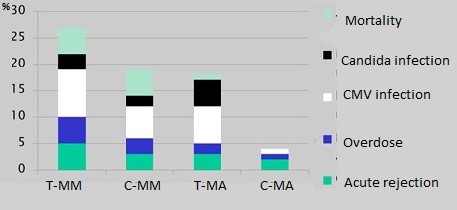
Figure 1. Types and rate of immunosuppressive therapy complications
C-MA – cyclosporine A - mycophenolic acid, C-MM – cyclosporine A - mycophenolate mofetil, CMV – cytomegalovirus, T-MA – tacrolimus - mycophenolate mofetil, T-MM – tacrolimus - mycophenolic acid
Figure 2 illustrates the causes of complications in various combinations of immunosuppressants. Acute rejection was often observed in combination with tacrolimus and mycophenolate mofetil at 4.0%. Despite the strict control of the dosage, overdose was observed and amounted to 4.0% in combination of tacrolimus and mycophenolate mofetil. CMV infection was found in all the combinations, but the combination of cyclosporine and mycophenolate mofetil amounted to 17.1%, being asymptomatic in 8% of patients, and in 5% patients wasaccompanied with deterioration of graft function and mortality. Candida infection was identified with 15% of patients. Mortality and candida infection were not observed in combination of cyclosporine and mycophenolic acid, however acute rejection was characteristic for this combination. Cyclosporine and mycophenolate mofetil caused high rate of complications and mortality (14.3%).
Analysis of causes of mortality (Fig. 2) revealed the highest percentage was accounted for chronic rejection, followed by acute rejection, CMV infection and sepsis, hepatic failure and cancer.
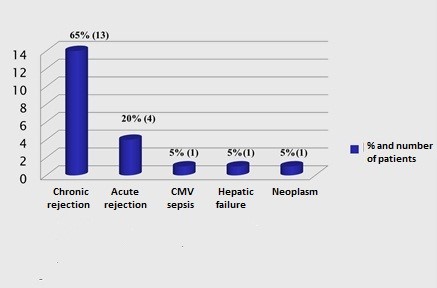
Figure 2. Causes of mortality in patients on immunosuppressive therapy after organ transplantation
CMV – cytomegalovirus infection
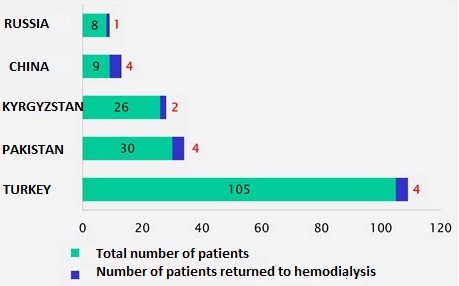
Figure 3. Absolute number of patients returned to hemodialysis program by country
After transplantation in case of rejection after the loss of graft function (Fig. 3), 15 (7.02%) patients returned to hemodialysis. There were 105 transplantations in the Republic of Turkey, 4 patients returned to hemodialysis, 30 transplantations in the Pakistan, 4 patients returned to hemodialysis, 26 transplantations in the Kyrgyz Republic, 2 patients returned to hemodialysis.
There were identified cases of acute and chronic rejection of different degrees at early stage, that was successfully managed with drugs in 17 (11.2%) of patients after the transplantation of kidney.
The overall graft survival in all patients from 1999 to 2017 was 84.2% (Fig. 4 and Table 3.). Among patients who underwent kidney transplantation and returned to hemodialysis, 4.8% - after transplantectomy and 2.2% without removal of graft, mortality rate for kidney transplantation was 7.9%. Mortality rate after liver transplantation was – 21.4%.
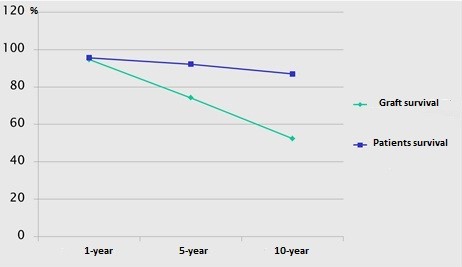
Figure 4. Survival of grafts and patients
|
Table 3. Mortality and survival analysis of grafts and patients (1999-2017) |
|
|
Overall survival of grafts, % |
84.2 |
|
Overall survival of patients, % |
91.2 |
|
Return to hemodialysis, n (%) |
16 (7.0) |
|
With kidney removal (transplantectomy), % |
4.8 |
|
Without kidney removal, % |
2.2 |
|
1-year grafts` survival, % |
94.7 |
|
1-year patients` survival, % |
95.6 |
|
5-year grafts` survival, % |
74.2 |
|
5-year patients` survival, % |
92.2 |
|
10-year grafts` survival, % |
52.4 |
|
10-year patients` survival, % |
87 |
|
Overall mortality, n(%) |
20 (8.7) |
|
Mortality after liver transplantation, n(%) |
3 (21.4) |
|
Mortality after kidney transplantation, n(%) |
17 (7.9) |
Our study has limitations as being descriptive in design and includes relative small number of patients.
In conclusion, the overall graft survival of patients who underwent kidney and liver transplantation from 1999 to 2017 was 84.2%. Combinations including cyclosporine, were associated with high rate of complications acute rejection, CMV and candida infections as compared to tacrolimus. The most unfavorable in terms of mortality was combination of cyclosporine – mycophenolate mofetil.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: J.A. and J.G. equally contributed to the preparation of brief report
Acknowledgement and funding: None to declare.
Informed consent for procedures and treatment was obtained from all patients as a part of center policy (retrospective study)
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

