Choosing the vascular access in interventional cardiology: evolution and contemporary practice
REVIEW
Choosing the vascular access in interventional cardiology: evolution and contemporary practice
Article Summary
- DOI: 10.24969/hvt.2021.260
- Page(s): 123-130
- VASCULAR DISEASES
- Published: 14/07/2021
- Received: 02/06/2021
- Revised: 13/07/2021
- Accepted: 14/07/2021
- Views: 9874
- Downloads: 6118
- Keywords: radial artery, femoral artery, ulnar artery, brachial artery, cardiac catheterization, percutaneous transluminal coronary angioplasty
Address for Correspondence: Paulo Vinicios Falcao Duarte, Interventional Cardiology Department, Instituto Nacional de Cardiologia, Rua das Laranjeiras, 374, Rio de Janeiro, 22240-006, Brazil, Phone: +55 21 30372288
E-mail: pv_falcao@hotmail.com
1Interventional Cardiology Department, Instituto Nacional de Cardiologia, Rio de Janeiro, Brazil
2Research and Teaching Department, Instituto Nacional de Cardiologia, Rio de Janeiro, Brazil
Abstract
Percutaneous coronary diagnostic and therapeutic procedures are very frequent worldwide and therefore bring to discussion the best vascular access for each patient. The vascular access for coronary angiography or coronary interventions must be chosen according to the patient's clinical and anatomical characteristics, as well as the experience of the interventional cardiologist. Several studies have shown the superiority of radial access compared to femoral access, reducing local complications, major cardiovascular events, death and hospital costs. The ulnar approach is a feasible and safe option in the absence of radial access.
Key words: radial artery, femoral artery, ulnar artery, brachial artery, cardiac catheterization, percutaneous transluminal coronary angioplasty
The use of percutaneous diagnostic and interventional catheterization procedures is very high worldwide, reaching 480.000 coronary angioplasty interventions in the USA in 2014 (1). Initially, cardiac catheterization was performed through brachial or femoral sites; however, due to frequent complications such as local bleeding, and also to the need for hospital stay in the latter, with its additional costs, other techniques using different types of access were developed (2, 3).
In the last two decades, the radial access route has been demonstrated to be safer than the femoral route for percutaneous coronary procedures - either coronary angiography or coronary angioplasty. This route has proven to reduce the risk of vascular complications, hospital admission, hospital costs, time to ambulate, besides increasing patient comfort (2, 4).
Despite being the preferred route, the radial access also has limitations, including the propensity to vasospasm, small diameter and frequent anatomic variations, which result in up to 10% failure rate in attempted catheterization. Therefore, before choosing the access route, it is important to thoroughly know local anatomy, techniques and potential complications, besides taking into account the patient´s clinical aspects and the operator´s experience (4).
Temporal evolution of vascular access choices in interventional cardiology
Since the 1930´s decade, several reports of partial, nonselective opacification of the coronary vessels through aortography have been published, using different access routes and techniques such as retrograde, left ventricular puncture and via sternal needle puncture of the aorta (5).
The first registered selective coronary angiography was performed in 1958. After studying the left ventricle of a patient with valve disease, Mason Sones pulled back the catheter to the aorta and accidentally catheterized the right coronary ostium, injecting 40 ml of contrast. The patient had brief asystole, which ceased after provoked cough. Shortly afterward, Sones developed the technique of selective coronary angiography with specially designed catheters for the dissection of the brachial artery (5).
In 1967, Judkins and Amplatz developed the antegrade technique with femoral artery puncture for selective angiography of the coronary arteries (5). In 1989, Campeau described the first coronary angiographies using the radial route, with low complication rates, due to the absence of nerves and large veins close to the sheath insertion site, to the superficial localization of the radial artery, which enables easy hemostasis, and also to the dual arterial irrigation of the hand, by radial and ulnar arteries, preventing hand ischemia (6).
General aspects of the main access routes
Radial access route
The transradial access was an innovation for procedures in interventional cardiology. Despite being developed in 1989, it was employed in less than 50% of the procedures in most countries in 2010. During that time period, the femoral technique prevailed, due, in particular, to the longer learning curve of the procedure by the transradial approach (7).
Radial artery puncture technique
The distal portion of the radial artery in the forearm is superficial, covered by the integument and superficial and deep fasciae, located over the prominence of the radius.
For the puncture, the palm of the hand must be supported in the supine position and with an extended wrist, increasing the feasibility of the palpation of the radial artery. After administering local anesthesia with 1% lidocaine, the artery is punctured with a needle or 21-gauge catheter at a 30-degree angle, two centimeters from styloid process. After arterial puncture, a 0.018” guidewire is advanced and a 5 French sheath for diagnostic angiography or a 6 French sheath for percutaneous coronary intervention (Seldinger technique) is introduced. To reduce vasospasm, hydrophilic sheaths are recommended, as well as the administration of vasodilators such as nitroglycerin or verapamil (8, 9).
Pre-procedure assessment
The Allen's test was described in 1929, and consists of the simultaneous compression of the ulnar and radial arteries at the wrist for approximately 1 to 2 minutes.
It requires that the patient closes the hand tightly, until the hand skin becomes pale. After the hand must be opened quickly with extended fingers, and then the operator decompresses the ulnar artery and observes the color of the hand. If the patient has normal integrity of the hand circulation and a patent palmar arch, the pallor is quickly replaced by flushing in about 5 to 9 seconds. The process is then repeated to assess the untested artery (9).
Because Allen's test relies on a subjective analysis and may lead to false-negative results, in 2004 Barbeau modified it by adding pulse oximetry of the first finger to record oxygen saturation, as well as plethysmography. The method consists of vigorous compression of the radial artery for two minutes. The results are divided into four possible types: A, without dampening the pulse trace immediately after compression of the radial artery; B, dampening of the pulse trace; C, immediate loss of the pulse tracing followed by recovery of the tracing within two minutes; D, loss of pulse trace without recovery of the trace in two minutes. The findings showed that only 1.5% of the patients had a D classification, which precluded the use of the radial access (9, 10).
Despite the recommendations for the use of these tests before proceeding to radial or ulnar artery catheterization, their applicability has been questioned, mainly due to the subjective assessment of the Allen test but also due to doubts related to Barbeau's more objective technique in predicting ischemic risk of the hand during periprocedural arterial occlusion (11).
In fact, a single-center study assessed the safety of using transradial access across different Allen test results. Among 203 patients, the Allen test scores were described as normal in 83 patients (palmar flushing ≤ 5 seconds), intermediate in 60 (palmar flushing between 6 - 10 seconds) and abnormal in 60 (palmar flushing > 10 seconds). Barbeau's D pattern was not seen in patients classified as normal or intermediate Allen's test, but was seen in 40% of patients with an abnormal result. Serial measurements of the hand’s capillary lactate, plethysmography of the first finger and tests to measure the isometric strength of the hand and forearm were performed. The result showed no difference in the three groups and no case of hand ischemia was reported (12).
Several reasons can lead to the failure to obtain the radial access for the hemodynamic study; among them are calcification, tortuosity and a small-caliber radial artery. Radial spasm and loops of the radial and brachial arteries should also be considered (8).
The failure rate in obtaining the radial access, with the need to choose another site, varies between 4.6% and 10%, with the operator's experience being a considerable predictor of this value (4). Other predictors for failure of radial access catheterization include age greater than or equal to 75 years, female gender, short biotype, previous revascularization surgery and cardiogenic shock (4).
A common complication, which can lead to failure in acquiring this route, is the spasm of the radial artery, which is reported in 10% of cases. This is due to the greater presence of alpha-1 and alpha-2 receptors, leading to an accentuated spasmodic response due to the catecholaminergic stimulation, unlike other arteries in the arm. Measures such as the technique of careful puncture, administration of antispasmodic drugs, like calcium channel blockers or nitrates, local anesthetics and use of hydrophilic sheaths are the pillars to prevent this complication (13). If clinically severe spasm occurs, it can often be treated successfully with repeated doses of intra-arterial vasodilators, local anesthetics, increased analgesia and sedation. In extreme cases of vasospasm, operators have employed an axillary nerve block, deep sedation or even general anesthesia to allow removal of the sheath (13).
The risk of occlusion of the radial artery after its use as an access route in interventional cardiology is 5%. Factors such as the ratio between arterial diameter / sheath diameter greater than 1, inadequate systemic levels of anticoagulation, prolonged hemostatic dressings and repeated cannulations are associated with the increase in this complication rate (13).
In most patients, occlusion of the radial artery is asymptomatic, and rarely results in ischemia of the hand due to the blood supply provided through the palmar arch (13). However, ischemia of the hand is a potential complication whenever radial or ulnar access is used. Treatment of symptomatic occlusion with low-molecular-weight heparin has been described, with symptom resolution in 86.7% of treated patients compared with 19.1% of untreated patients (p<0.001) (14).
Forearm hematoma formation is usually immediate and clinically apparent during radial approach procedures due to the superficial course of the radial artery. Although severe bleeding complications are rare, prompt identification and treatment are important to minimize the negative impact on these patients. In cases of hematoma extending to the forearm, measures such as reversal of the effect of unfractionated heparin, intermittent inflation of blood pressure cuff in the forearm and analgesia are instituted. In case of extensive hematoma leading to ischemia (compartment syndrome), surgical fasciotomy should be considered (13, 15).
The pseudoaneurysm formation is a rare complication of transradial catheterization and may present late after the procedure. Treatment of a radial pseudoaneurysm is usually successful with prolonged compression; however, thrombin injection and surgical repair may be required in rare cases (13).
Left distal radial access
Described in 2017, the technique consists of puncture of the distal left radial artery, on the back of the hand, at the level of the anatomical snuffbox, positioning the patient's arm more anatomically during the procedure. The great apparent benefit is to provide greater comfort for the patient and the operator, and avoid radial artery occlusions at the site of the forearm (16) (Fig. 1)
Femoral access route
The femoral artery remains one of the main access routes in interventional cardiology, as it requires a shorter learning curve and offers an excellent route in cases of complex angioplasties that require larger sheaths and in studies of grafts of patients with previous surgical revascularization, mainly in cases of double use of the mammary arteries (17).
Femoral artery puncture technique
To perform the procedures in interventional cardiology through the transfemoral route, it is important to puncture the vessel in the middle of the common femoral artery, above the bifurcation of the femoral artery in superficial and deep, and 2-3 cm below the inguinal ligament.

Figure 1. Position of the patient's arm during examination performed by the distal radial route (Authors´ own material)
To reduce these risks, it is recommended to puncture the femoral artery guided by ultrasound or after identification of reference points with the aid of fluoroscopy, such as the lower edge of the femoral head (19) (Fig. 3).
A multicenter, randomized trial, showed that femoral arterial access with ultrasound guidance reduced the number of attempts, improved first pass success rate, reduced the rate of venipuncture, reduced median time to access, and reduced vascular complications (1.4% vs. 3.4%, p=0.04) in comparison with standard fluoroscopic guidance (20).
Complications of the femoral access
The hematoma, a collection of blood within the soft tissues of the upper thigh, is more common than free bleeding, usually occurs through the puncture site, and in most cases both can be controlled by prolonged manual compression (21). Retroperitoneal hematoma is a complication with high morbidity and mortality, usually caused by a femoral artery puncture above the inguinal ligament. The diagnostic suspicion is important to initiate the proper management. Often the only clue is unexplained hypotension (particularly, if it responds only briefly to aggressive volume loading), fall in hematocrit, or ipsilateral flank pain following a femoral catheterization procedure.
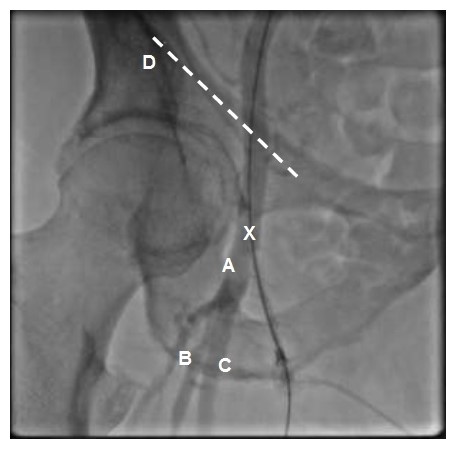
Figure 2. Relevant regional anatomy for femoral artery catheterization: A: Common femoral artery. B: Deep femoral artery. C: Superficial femoral artery. D: Inguinal ligament (dashed line). The illustration shows the femoral artery running under the inguinal ligament. The arterial puncture site (indicated by the X) should be performed approximately 3 cm below the inguinal ligament. (Authors´ own material)
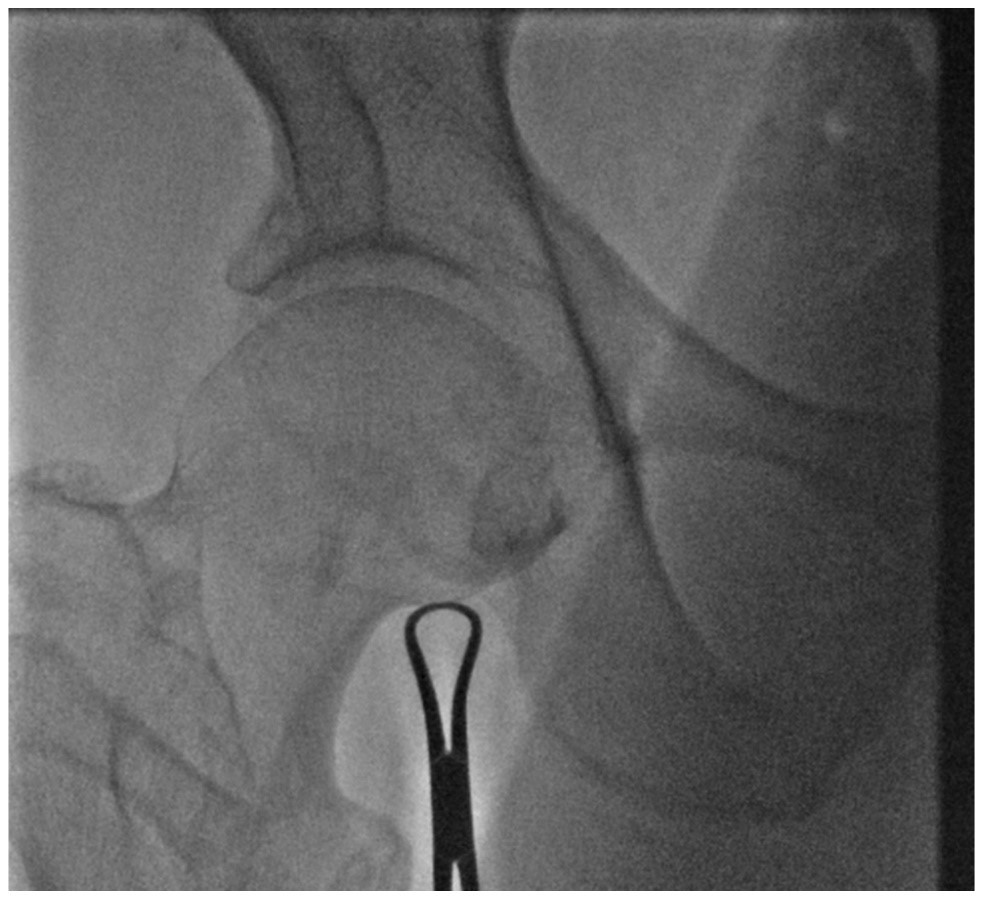
Figure 3. Identification of the lower edge of the femur head with fluoroscopy as a reference point. (Authors` own material)
Pseudoaneurysm is a continued connection between the arterial lumen and a saccular expanding hematoma. This often results from femoral access obtained from a low puncture of the superficial or profunda femoral artery. The incidence of a femoral pseudoaneurysm has been reported from 1 to 6%. Smaller (2-3 cm), asymptomatic pseudoaneurysms can be conservatively managed with spontaneous resolution in most cases. In some cases, the treatment consists of external compression or thrombin injection guided by ultrasound (22).
An arteriovenous fistula results from a persistent arterial connection with a vein and has been reported in 1% of transfemoral approach. Like a pseudoaneurysm, an arteriovenous fistula results from femoral access obtained from a low puncture of the superficial or profunda femoral artery. Management is often conservative. For larger or symptomatic arteriovenous fistula, manual compression is the primary approach, and surgical intervention is reserved for rare cases (20).Femoral artery thrombosis can occur in patients with a small common femoral artery lumen (peripheral vascular disease, diabetes, female gender), in whom a large-diameter catheter or sheath. This requires urgent vascular assessment (for exploration and correction of any local dissection or plaque avulsion and Fogarty embolectomy of the distal vessel as needed to restore distal pulses)(21).
Comparison between femoral and radial accesses
A meta-analysis of 24 randomized studies, totaling 22,844 patients, comparing coronary intervention via transradial and transfemoral access, showed a reduction in the risk of all causes of death (1.55 x 2.22, p = 0.001), a lower rate of major cardiovascular events (5.56 x 6.67, p = 0.002), major bleeding (1.07 x 2.07, p≤0.001), and major vascular complications (0.24 x 1.12, p ≤0.001) in the transradial group. The rates of acute myocardial infarction (AMI) and stroke were similar in both groups, with an AMI odds ratio of 0.92 (0.80 - 1.05) and a stroke of 1.05 (0.70 - 1.59)(23).
The costs were lower when compared to the radial and femoral accesses, mainly due to the lower rates of vascular and hemorrhagic complications, shorter length of stay in the intensive care unit and small differences in the cost of the procedure, reaching a difference of U $ 1,621.00 in patients at high risk of bleeding (24).
Brachial access route
One of the first access routes to be used in interventional cardiology, the brachial artery dissection technique (Sones) is in disuse, due to the option of safer access and with a shorter learning time curve. Its use is restricted to cases of anatomical adversities through the radial and femoral routes (25).
Comparison between brachial, radial and femoral accesses
An analysis of a registry published in 1982 evaluated 53,581 patients who underwent interventional cardiology procedures for 14 months in 66 hemodynamic laboratories in the USA. The procedures were performed mostly through the femoral approach (54%), followed by the brachial approach (43%). The study showed a rate of thrombosis or decrease in brachial pulse of 0.42% (98 patients), requiring surgical correction in 93.8% of cases. The rate of laceration or brachial dissection was 0.15%, with 55.5% being treated surgically (26).
Between 1965 and 1980, 73,750 cardiac catheterizations were performed using the brachial dissection technique (Sones) at a single center in the USA. The complication rate requiring thrombectomy or arterial reconstruction was 1.5% (1,108 patients), due to post-procedure brachial artery occlusion (27).
In general, the percutaneous puncture technique of the brachial artery (Seldinger) tends to be discontinued, favoring radial access, since the control of bleeding in the post-procedure period is often difficult. Compared to the femoral approach, the brachial approach also carries a slightly higher risk of vascular complications (28).
A randomized study, which compared different access routes in coronary artery angioplasty, showed that the rate of major bleeding, defined as a fall of hemoglobin ≥ 2 mmol / L, necessity of blood transfusion or surgical repair, was 2.3% in the group by brachial approach, 2.0% by femoral approach and none by radial approach (p = 0.035)(28).
Ulnar access route
Limitations of the ulnar access
The limitations of the transulnar approach are explained by the deeper path in the forearm, making palpation more difficult and the most laborious hemostasis as a result of the absence of compression under a rigid surface such as bone structure (30, 31). Local complications can be the same through the radial approach, associating the ulnar nerve injury.
Comparison between the ulnar and radial accesses
A randomized study evaluated 2,532 patients who underwent radial (n = 1,262) or ulnar (n = 1,270) procedures in interventional cardiology, performed by experienced operators (defined as at least 50 procedures performed by the transulnar route). The primary outcome consisting of major cardiovascular events, crossover of the access route, major vascular complications (extensive hematoma with a fall in hemoglobin> 3mg / dl or need for blood transfusion) and arterial occlusion was 14.4% by the transradial route and 14.6 % by transulnar route (p = 0.92). The crossover rate was 4.4% by the ulnar route and 3.8% by the radial route (p = 0.44), major bleeding (0.9% x 1.0%; p = 0.69) and hematoma of the forearm (3.24% x 3.07%; p = 0.64)(32).
A meta-analysis published in 2018 analyzed six randomized studies, totaling 5,299 patients, comparing the transradial and transulnar access route in coronary angiography or percutaneous coronary intervention. The study showed no difference in major cardiovascular events (3.3% x 3.0%, p = 0.53), bleeding or hematoma (2.0% x 2.5%, p = 0.23%), fluoroscopy time or contrast volume between the two groups. Although the access failure with the necessity to choose another route tended to be greater by the transulnar technique, there was no statistical significance compared to the transradial group (3.8 x 9.4%, P = 0.09) (33). The findings of the meta-analysis suggested ulnar access is a safe alternative to radial access, but more laborious to perform.
Safety of ipsilateral ulnar access in case of impossibility or failure of transradial access
Kedev et al. prospectively evaluated 476 patients who underwent percutaneous coronary intervention by the ulnar route, in which in 240 patients the ipsilateral radial artery was occluded and in 98.7% of the patients with occluded radial artery, procedures had already been performed by this route. Coronary intervention by the ulnar approach showed to be viable and safe, with high success rates and low incidence of vascular complications. At the 30-day follow-up, there was no difference in complications in patients with patent or occluded radial artery (34).
A retrospective study, in a single center in Asia, analyzed 87 patients who underwent coronary intervention via the ulnar route, with ipsilateral radial occlusion confirmed by forearm angiography. In that study, 80% of patients had a previous history of cannulation or surgery of the radial artery. At 33-month follow-up, no ulnar artery occlusion, hand ischemia or serious complications requiring surgery or blood transfusion were observed, only 2.3% of patients had a hematoma >5 cm. The pre-procedure angiographic review of the forearm showed that 95.7% of the patients had significant collaterals from the interosseous artery to the distal portion of the radial artery, after the occlusion segment. Thus, blood circulation in the palmar arch and digital vessels was maintained even with the ulnar artery temporarily occluded by the ulnar arterial sheath (35).
Conclusion
Despite the longer learning curve, the radial access is the first route of choice in interventional cardiology in several countries, showing a reduction in vascular complications, major cardiovascular events, death and hospital costs, in addition to providing greater comfort for the patient when compared with the femoral access.
The femoral access offers an excellent route of choice in cases of complex angioplasties such as bifurcation lesions with two-stent techniques and chronic occlusions, as it allows the use of larger caliber sheaths and in studies of grafts of patients with previous surgical revascularization, especially in cases of use double mammary arteries.
The ulnar approach is a good option when the radial artery presents adversities such as a loop or reduced caliber, with higher rates of puncture attempts and crossover. The ipsilateral ulnar access in the absence of a radial approach (occlusion or spasm after attempting a radial puncture) is a feasible and safe alternative, showing low rates of local complications.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: P.V.F.D. and A.D.L. are equally contributed to article preparation
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Bedford river, United Kingdom. Naren Kumar, Blackpool, UK
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

