Large patent ductus arteriosus in a 14-month-old girl with low birth weight
CASE REPORT
Large patent ductus arteriosus in a 14-month-old girl with low birth weight
Article Summary
- DOI: 10.24969/hvt.2021.282
- Page(s): 190-193
- Cardiac Surgery
- Published: 06/11/2021
- Received: 20/10/2021
- Accepted: 03/11/2021
- Views: 5779
- Downloads: 5573
- Keywords:
Address for correspondence: Abai K. Turdubaev, Scientific Research Institute of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan Email: abai.turdubaev@gmail.com
Abstract
We present a case of a large patent ductus arteriosus closure with Amplatzer ductal occluder in a 14-month-old girl with low birth weight.
Abai K. Turdubaev, Malika A. Kakharova.
Scientific Research Institute of Heart Surgery and Transplantation of Organs of the Ministry of Health of the Kyrgyz Republic, Bishkek, Kyrgyzstan
Abstract
We present a case of a large patent ductus arteriosus closure with Amplatzer ductal occluder in a 14-month-old girl with low birth weight.
Key words: large patent ductus arteriosus, ductal occluder, congenital heart defects
Introduction
The number of children born with congenital malformations is increasing every year, of which congenital heart defects are in the second place. The average prevalence of congenital heart defects in different countries ranges from 8-12 per 1000 live births. Congenital heart and cardiovascular diseases account for 47% of all causes of death from malformations (12.2 per 10 000 live births) (1-3).
Correction of a patent ductus arteriosus (PDA) percutaneously with a device was first described by Porstmann et al. in 1971 (4). The Amplatzer ductal occluder (ADO) device became widely used and is still the leading method for closure of congenital PDA, atrial septal defects and ventricular septal defects.
The duct occluder is a mushroom-shaped, self-expanding, movable device made of 0.004 inch nitinol wire mesh with Dacron patches inside (5). Despite several advantages of the new duct occluder device using this method, the closure of large defects remains a problem.
In this article, we would like to present a clinical case of successful non-surgical closure of wide ductus arteriosus in a 14- month child with low birth weight.
Case report
A girl aged 14 months weighing 9 kg, from the first full-term pregnancy proceeding on the background of an acute respiratory viral infection, born on time was admitted to our clinic. Patent ductus arteriosus was identified at the age of 6 months. The observation revealed shortness of breath and fatigue when feeding, palpitations, as well as lag in physical development and frequent flu.
Echocardiography data revealed: a dilated pulmonary artery, a duct of 12 mm in diameter with systolic- diastolic continuous flow, a pulmonary artery trunk size of 26 mm, a pulmonary artery pressure peak systolic pressure of 32 mm Hg, dilatation of both ventricles, as well as functional mitral and tricuspid regurgitation, shunt through a foramen ovale with a diameter of 1 mm and the presence of severe pulmonary hypertension. In the presence of clinical indications and instrumental data, it was decided to correct the PDA using the duct occlude device.
On aortography a wide patent ductus arteriosus was visualized (Fig.1). This was a type A defect with a PDA of 4.3 mm in diameter and 8.9 mm in length (6). The guidewire was passed transvenously through the PDA into the descending aorta, and a delivery system was inserted through it to implant the occluder. An ADO of 14-12 mm was implanted with antegrade duct access (Fig. 2, 3).
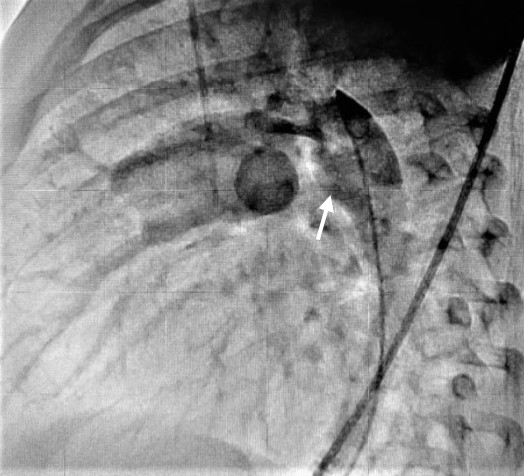
Figure 1. Fluoroscopic image of patent ductus arteriosus
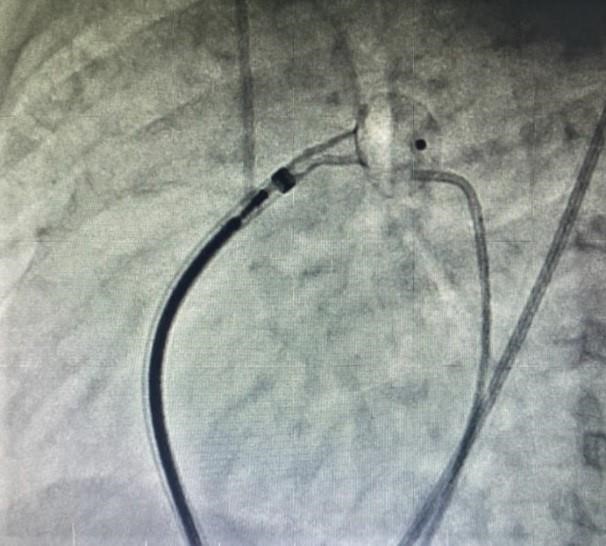
Figure 2. Amplatzer ductal occluder in patent ductus arteriosus position
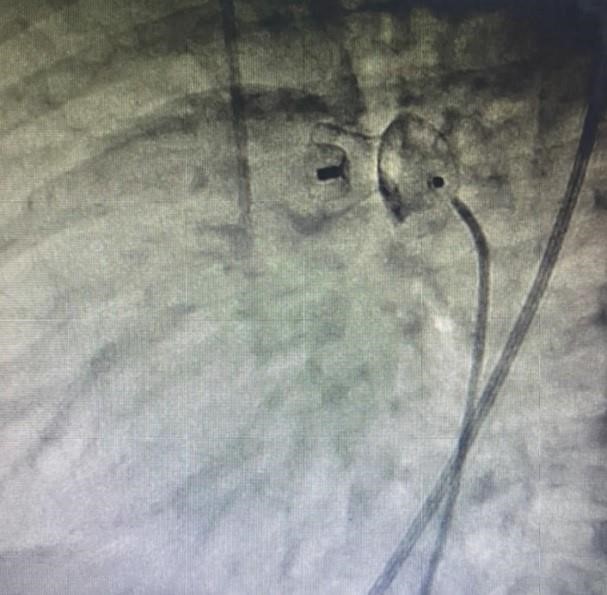
Figure 3. Amplatzer duct occluder device after installation.
Discussion
There are surgical and percutaneous methods for correcting PDA. Surgical ligation uses titanium clamps; early surgical ligation minimizes the side effects of HS PDA and is more commonly used in low birth weight premature infants (7). The method of extrapleural surgical plasty of PDA is inexpensive and effective, with good cosmetic results, and is also more often used in premature infants (8). Gianturco coils have been used for small to medium diameter PDA with good postoperative results.
However, the leading method is the use of an ADO device, which is a low-traumatic and highly effective method. As in other existing manipulations, it has its complications. Thrombotic complications in the postoperative period are an urgent problem, since they retain a potential threat to life in children with congenital heart defects. Children are less prone to thrombosis than adults, as it is believed that thrombosis in pediatrics after surgery is rare (9). Pulmonary obstruction is also considered one of the complications of PDA occlusion, which is used in small children with a large device. Another rare but possible complication is occluder embolization, which is a serious complication that requires immediate surgical intervention.
Therefore, it is important to choose the right size corresponding to the diameter of the PDA, observing the echocardiography in dynamics and general condition of the child and echocardiographic monitoring.
Conclusion
1.With our experience, we illustrate the successful use of Amplatzer duct occluder to occlude large PDA in a 14 months old child.
2.Based on numerous studies and many years of experience of colleagues, it can be said that using Amplatzer duct occluder to close a medium and large size PDA shows good performance, exceeding the expected result.
3.To assess the effectiveness and safety of this method, more experience and long-term follow-up will be required.
Informed consent: Informed consent was obtained from parents of a child before each procedure
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: A.K. T., M. A. K. are equally contributed to patient care, preparation of manuscript and fulfilled authorship criteria
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Dresden castle square, Dresden, Germany 2021. Massimo Romano, Napoli, Italy
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

