Primary percutaneous coronary intervention in hyperacute inferior STEMI
IMAGE
Primary percutaneous coronary intervention in hyperacute inferior STEMI
Article Summary
- DOI: 10.24969/hvt.2022.301
- Page(s): 34-36
- Electrocardiography
- Published: 14/02/2022
- Received: 27/01/2022
- Revised: 10/02/2022
- Accepted: 11/02/2022
- Views: 5958
- Downloads: 4967
- Keywords:
Address for Correspondence: Juan Guzman Olea, Interventional Cardiology Department, SMART HEART. Periferico Ecologico No. 3507, Piso 14, Puebla, Mexico. E-mail: dr.juanguzmanolea@gmail.com
Juan Guzman Olea, Daniel Ivan Perez Vasquez, Hector Hugo Escutia Cuevas, Ana Hizel Barba Garcia, Jorge Guillermo Arenas Fonseca, Gabriel Guzman Olea, Miguel Angel Rojas Carrera, Juan Francisco Rodriguez Alvarado
Interventional Cardiology Department, SMART HEART, Periferico Ecologico, Puebla, Mexico
Primary percutaneous coronary intervention (PCI) is the preferred reperfusion therapy for ST elevation myocardial infarction (STEMI) patients in the first 12 hours after symptom onset, provided it can be performed quickly (120 minutes from STEMI diagnosis) by an experienced team (1, 2).
A 54-year-old male, with gender, physical inactivity and family history as cardiovascular risk factors, and without cardiovascular history was admitted to our hospital. He experienced severe typical oppressive chest pain lasting more than 20 minutes in addition to diaphoresis. He came immediately to our center, with Levin's sign and an electrocardiogram (ECG) was recorded (time from symptoms onset to medical contact and ECG recording – 25 minutes) documenting hyperacute changes of inferior STEMI: hyperacute T waves peaked in II, III aVF leads, early ST elevation and loss of R wave height in the leads II, III, aVF with reciprocal changes in leads I and aVL (Fig.1). Initial biomarkers were negative. The patient underwent primary PCI - door-to balloon time of 50 minutes.
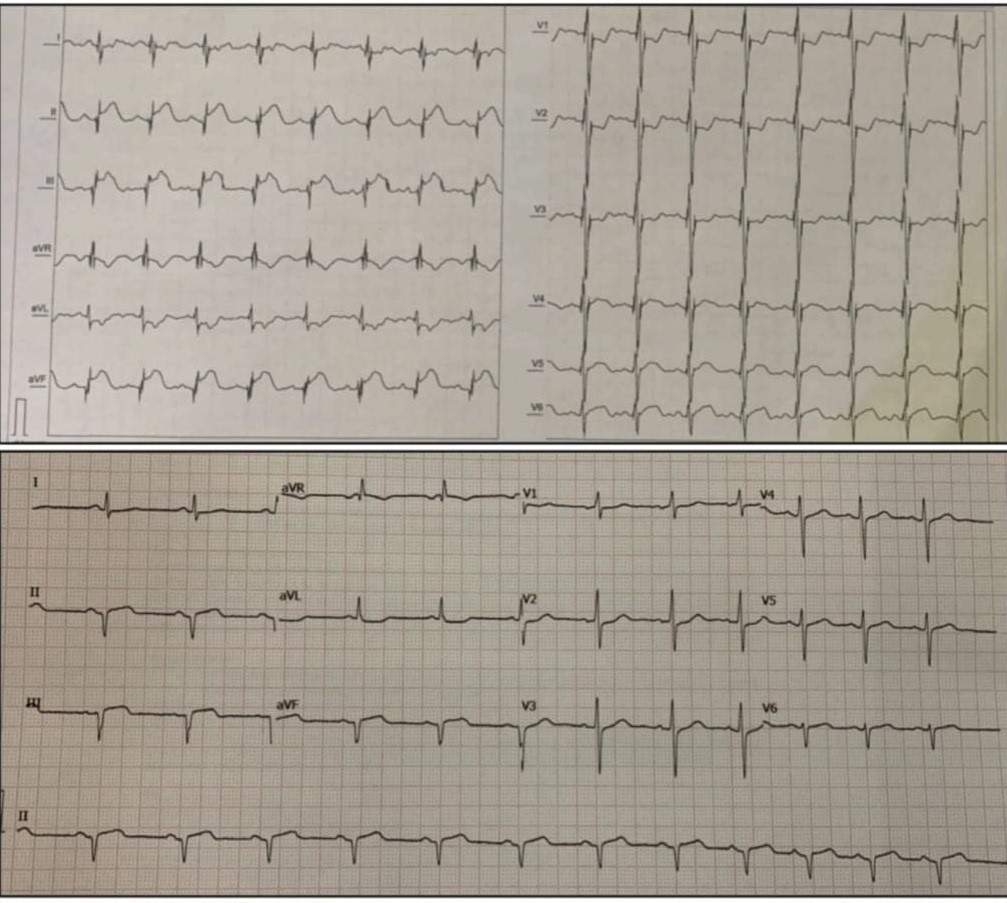
Figure 1. Initial electrocardiogram showing superacute changes of inferior STEMI and post-PCI electrocardiogram.
PCI – percutaneous coronary intervention, STEMI – ST-elevation myocardial infarction
A right proximal radial approach was performed and a Slender 6Fr introducer sheath was placed. We used JL 3.5 6 Fr catheter and the coronary angiogram revealed normal left main, left anterior descending, ramus and left circumflex coronary arteries. Then the right coronary artery ostium was cannulated with a JR4 6 Fr guide catheter and ectatic vessel was observed with acute total occlusion and a grade 5 thrombus at the junction of the middle segment with the distal one. A 0.014” Whisper guidewire was advanced towards the PD, atropine was used due to sinus bradycardia, the occlusion site was predilated with 2.0x20mm and 3.0x20mm balloons with adequate luminal gain and improvement of the flow. Due to embolization of the distal part with thrombus and slow flow, it was decided to use intracoronary glycoprotein IIb/IIIa inhibitor tirofiban bolus and continued infusion. Two Biolimus A9-drug-eluting stents 3.5x38mm and 4.0x28mm were implanted with final flow TIMI3, TMP3 (Fig. 2, Video 1).

Video 1 (see video images at www.hvt-journal.com). Coronary angiography showing RCA with acute total occlusion and a grade 5 thrombus. The second image shows final result.
Later he was transferred to the intensive care unit to continue medical treatment and phase 1 cardiac rehabilitation. Primary PCI is unequivocally the treatment of choice to achieve timely reperfusion of the infarct-related artery in STEMI. In this case, with an ectatic vessel and a high thrombus load, the adjuvant therapy including load of platelet antiaggregants (aspirin and clopidogrel), unfractionated heparin and tirofiban provided a good result. Advancements in STEMI care over the years, including antithrombotic approaches have contributed to the improvements in short and long term outcomes.
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: J.G.O., D.I.P.V., H.H. E.C., A.H.B. G., J. G.A.F., G.G.O., M.A.R.C., J.F.R. A. are equally contributed to the study and preparation of article
Acknowledgement and funding: None to declare
References
- 1. Borja Ibanez et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST- segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST- segment elevation of the European Society of Cardiology (ESC) Eur Heart J 2018; 39: 119-77.
- 2. Franz-Josef Neumann et al. 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur Heart J 2019; 40: 87-165.

Seagulls on Bari seacoast, Adriatic Sea. Bari Italy. Paolo Amico, Italy
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

