Multidetector computed tomography in the selection of the optimal surgical approach to the replacement of the aortic valve
REVIEW
Multidetector computed tomography in the selection of the optimal surgical approach to the replacement of the aortic valve
Article Summary
- DOI: 10.24969/hvt.2022.313
- Page(s): 22-27
- Cardiac Surgery
- Published: 13/03/2022
- Received: 10/11/2021
- Revised: 02/03/2022
- Accepted: 03/03/2022
- Views: 5503
- Downloads: 4677
- Keywords: multidetector computed tomography, minimally invasive surgery, aortic valve replacement, outcomes, surgical procedures
Address for Correspondence: Azat K. Turgunov, SRI of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan
Email: azatturgunov@gmail.com
Azat K.Turgunov, Taalaibek Z. Kudaiberdiev
SRI of Heart Surgery and Organ Transplantation, Bishkek, Kyrgyzstan
Abstract
More than 100 years have passed since the first successful operation on the aortic valve by expanding the stenotic aortic valve through the invaginated aortic wall by A. Taffer in 1914. Since then, medicine has been continuously developing, revealing new methods not only of diagnosis, but also of surgical treatment. One of these cases is, the role of multidetector computed tomography in the selection of the optimal surgical approach to replacing the aortic valve. We present here a review of current evidence on topic.
Key words: multidetector computed tomography, minimally invasive surgery, aortic valve replacement, outcomes, surgical procedures
Introduction
The relevance of this topic is due to the fact that in the structure of cardiovascular diseases, acquired defects account for up to 25% and are second only to coronary heart disease and hypertension in prevalence (1, 2). There are many acquired heart defects, and a special place is occupied by aortic valve defects, among which calcinated aortic stenosis (AS) is the most common organic lesion of the heart valves found in cardiology practice, which accounts for approximately 25% of all valvular heart diseases. The incidence of this defect in the general population is steadily increasing: in persons older than 65 years - 3-4%, in patients 80 years and older - 7-8% (degenerative, senile aortic stenosis) (3, 4).
Currently, surgical treatment of aortic heart defects includes replacement of valve with an artificial prosthesis. The technique of aortic valve replacement (AVR) has already become a proven, routine procedure performed by accessing the heart through a longitudinal median sternotomy, which is recognized as the "gold standard" in all cardiac surgeries (5,6).
Despite the obvious advantages of longitudinal median sternotomy as access to the heart, in-depth studies in recent years have made it possible to report potential disadvantages of access associated with high invasiveness, the risk of bleeding (7), the development of superficial soft tissue infections and mediastinitis (8), when postoperative mortality reaches up to 50% (6).
Taking in account disadvantages of longitudinal median sternotomy and as the technology of heart surgery improved, cardiac surgeons sought out and developed new surgical techniques that would provide less traumatic operations that exclude longitudinal median sternotomy. Thus, cardiac surgery has changed its direction in the direction of reducing invasiveness (9).
Mini invasive AVR (mini-AVR) was proposed by Cosgrove and Sabik in 1996 (10). Over time, the most common used technique is the upper partial (j-shaped) sternotomy (Fig. 1) (11). The accumulation of experience and the study of the results of interventions have created the conditions for the widespread adaptation of mini-AVR (port access). However, the mini-AVR remains a rare operation, most commonly performed in Germany at 25%. In the United Kingdom and the United States, only 12% of interventions were performed using mini-access (12).
However, some studies have shown that smaller incisions lead to poor visibility, potentially making surgery more complex and dangerous, as well as increasing the time of surgery (13).
Imaging for optimal surgical access
Currently, the use of modern diagnostic methods to prepare the patient for surgery, such as multidetector computed tomography (MDCT), is the most informative in solving the issue of optimal surgical access.
Rapid technical improvement of MDCT has significantly expanded the possibilities of non-invasive diagnosis of heart and coronary artery diseases.
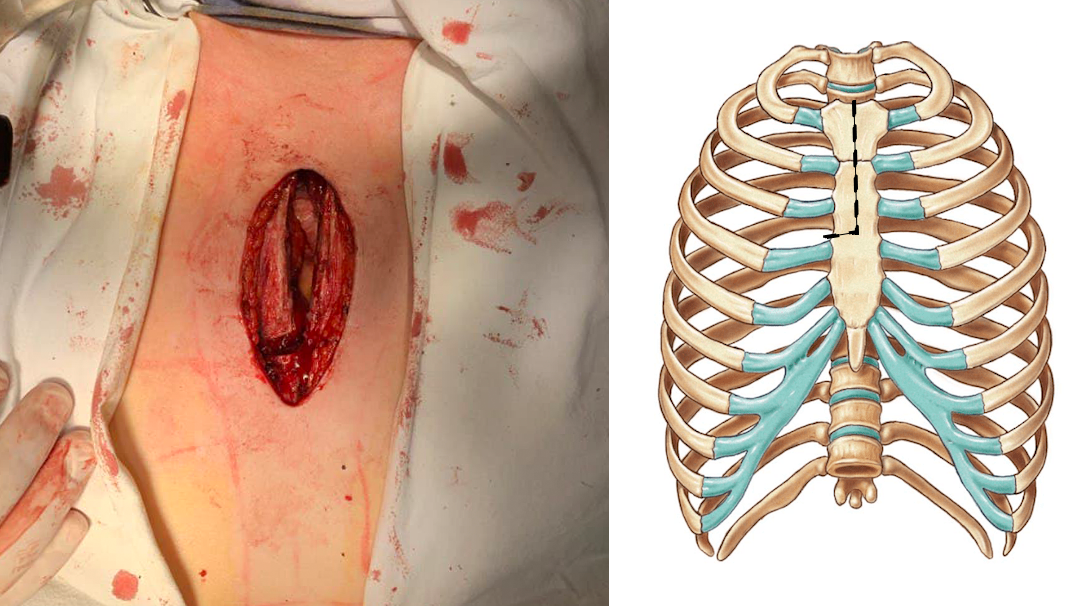
Figure 1. “J” mini sternotomy, minimally invasive aortic valve replacement
The appearance of multi-detector computed tomography systems with 64, 256 and 320 rows of detectors has significantly improved the quality of the images, which makes it possible to assess not only the lumen of the coronary arteries, the condition of the heart cavities and the thickness of the wall, but also to analyze the functions of the chambers, to identify pathological changes in the valves and their location in relation to the sternum (14).
According to MDCT, the clear boundaries of the heart are already known, which are located in the lower front part of the mediastinum, to the left of the median plane by an average of 13.8 (0.9) mm. Transverse dimensions prevail over the anterior and posterior - 100.9 (0.6) mm and 105.1 (1.7) mm, respectively. In relation to the sternum, the heart is located at 7.0 (0.5) mm; relative to the spine - 22.1 (1.0) mm. Heart cavities, as well as partitions between individual chambers, as a rule, can be detected only with bolus contrast. This is due to the fact that the density of blood in the chambers of the heart is approximately equal to the density of the myocardium. The outer contour of the heart is formed by the pericardium and a strip of epicardial fat. The pericardium attaches to large vessels at the level of the aortic arch, forming a kind of "bag", the contents of which are the heart, adipose tissue and parts of large vessels emanating from the heart or flowing into it (15).
To determine optimal surgical access, the most important is to obtain dynamic computed tomography angiography images at70% of the cardiac cycle (mid-diastole) because in this phase the aortic valve is closed (16). The access distance and the angle of access are determined on the basis of the location of three landmarks: the center of the aortic ring, the sinotubular junction and the incision site (periosteal joint) (Fig. 2, 3) (17).
Glauber et al. (18) stated that patients are suitable for minithoracotomy only if the following criteria are met: 1. the distance from the ascending aorta to the sternum should not exceed 10 cm; 2. the angle between the midline of the sternum and the slope of the ascending aorta should be greater than 45°. It has also been suggested that it is important to measure the size of the aortic valve, such as the diameter of the aortic valve ring, the length of the ascending aorta, and the calcification of the aortic valve and ascending aorta during the planning process before the procedure, as this is very important. It is recommended to remove all eccentric calcifications and create a complete decalcification of the aortic ring (18, 19).
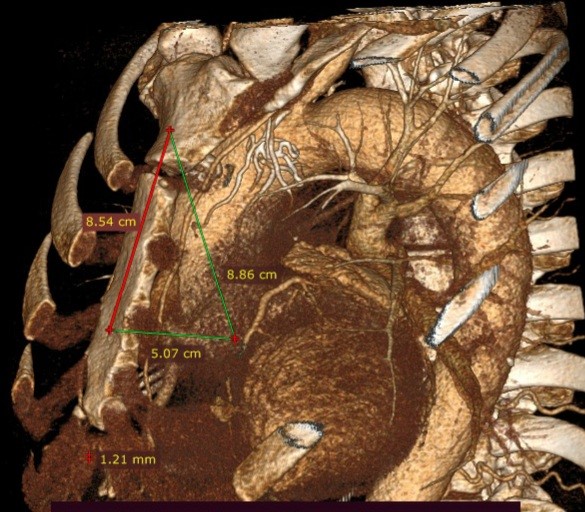
Figure 2. Contrast-enhanced multidetector computed tomography. Mid-clavicular line. Access distance and angle of access are determined based on the location of three landmarks: the center of aortic annulus, the sinotubular junction, and the incision site: 8.54 cm is the proposed skin incision line (2cm below the jugular notch, up to the 4th intercostal space)
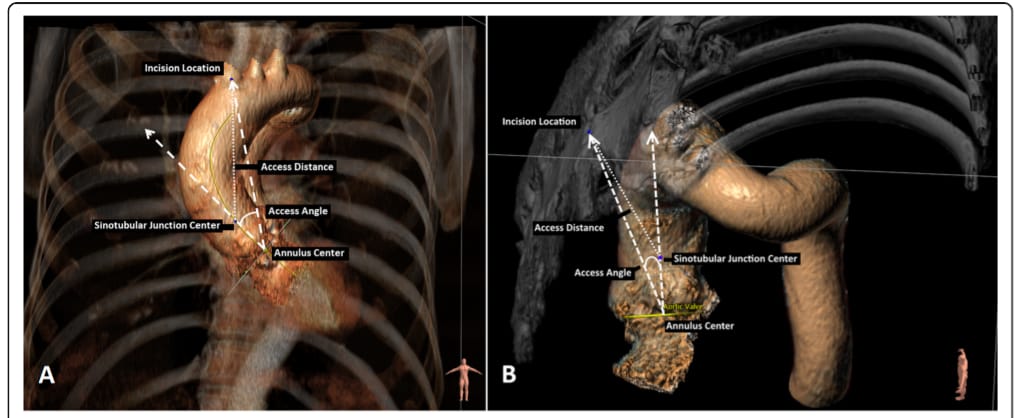
Figure 3. Anterior (surgical) view of the aorta and chest. B) Latero-superior projection of the aorta and part of the thorax. Access distance and angle of access are determined based on the location of three landmarks: the center of the aortic annulus, the sinotubular junction, and the incision site (arm-thoracic joint) (Reproduced from ref 17. Copyright 2019; under CC-BY 4.0 license)
|
Table 1. Outcomes of minimal invasive AVR |
|||||||||||||||||||
|
Study |
Type of AVR |
Preoperative characteristics |
Operative characteristics |
Postoperative outcomes |
|||||||||||||||
|
Male, n |
NYHA |
Age, years |
Duration of surgery, min |
Cross-clamp time, min |
CPB time, min |
Hospital, days |
Packed red blood cells, units |
Resternotomy for major bleeding |
|||||||||||
|
Henryk et al. 201820 |
Full-AVR 126 patients |
51 |
3.0 (1.0) |
70.02 (10.51) |
198.46 ( 47.21) |
70.01 (18.96) |
108.52 (32.77) |
11 |
1.75 (2.73) |
4 |
|||||||||
|
Mini-AVR 91 patients |
69 |
3.0 (1.0) |
69.79 ( 10.38) |
194.13 ( 37.47) |
76.43 (18.85)
|
107.46 (24.02) |
10 |
0.88 (1.35)
|
3 |
||||||||||
|
Snegirev et al. 201926 |
Full-AVR 56 patients |
31 |
3.0 (1.0) |
61.5 (11.3) |
173.2 (3.3) |
62.0 (14.0) |
85.1 (20.9) |
7.7(2.2) |
2.5(1.5) |
2 |
|||||||||
|
Mini-AVR 66 patients |
69 |
3.0 (1.0) |
64.6 (11.6) |
206.0(47.9) |
84.9(23.4) |
117.9 (30.4) |
7.4(2.7) |
2.0(1.3)
|
3 |
||||||||||
|
Multi-detector computed tomography guided AVR |
|||||||||||||||||||
|
Boti et al. 2019 17 |
100 Patients
|
Female, n(%) |
NYHA class ≥ III, n(%) |
Age |
Mean ( standard deviation) |
β-coefficient (95 CI%) |
|||||||||||||
|
34 (34) |
16 (16) |
71 (63, 75) |
Annulus minimum diameter (mm) |
Annulus maximum diameter (mm) |
Annulus area (mm2) |
Calcium volume (mm3) |
Distance from incision (mm) |
Access angle (degrees)
|
|||||||||||
|
23.8 (3.3) |
29.1 (4.1) |
5.5 · 102 (1.8 · 102) |
0.008 (0.000, 0.016) |
0.074 (− 0.28, 0.43) |
−0.090 (−0.50, 0.32) |
||||||||||||||
Planning tool mini-AVR provides both distance and angle of access from potential incision sites to the aortic root based on the geometric location of the landmarks of the aortic root and incision sites (19). These parameters are defined as follows: the access distance is defined as the distance between the location of the incision in the breast bone and the sinus tubular junction of the aorta as for ministerial, and for traditional approaches. The access angle is defined as the angle between the centerline of the aortic root and the incision-ring line. Central axis of the aortic root-it's a vector connecting the centers of the ring and sinotubular connection. The central axis of the cut-ring is a vector that connects the incision to the center of the ring. Other dimensions of the ring space, such as minimum, maximum diameters, area, perimeter and the volume of calcium is calculated on the basis of the previously presented automated method, which automatically determines the landmarks of the aortic root and calculates the size parameters (19). Some parameters are shown in Table 1.
Outcomes of mini-AVR
Claims to reduce postoperative complications, length of stay, and mortality were based on studies comparing traditional aortic valve surgery with minimally invasive techniques (20). Small incisions in minimally invasive surgery have the proposed advantage of less surgical trauma resulting in less postoperative bleeding, fewer blood transfusions, and a lower incidence of deep wound infections of the sternum (21-24).
In addition, patients tend to experience less pain and faster postoperative recovery, along with improved cosmetic outcomes, leading to faster recovery and a faster return to normal activities (25).
Finally, avoiding the use of partial sternotomy theoretically allows for a safer re-entry in the event of a second operation. Therefore, many people believe that minimally invasive aortic valve prostheses have become an effective treatment option in experienced centers, providing greater patient satisfaction and a lower complication rate (16, 26).
According to a study by Henryk et al. (14) (Table 1), where 126 patient underwent mini-AVR and 91 patients had complete AVR. Mini-AVR was associated with a decrease in ventilation time (6 h (minimum, min 3 h; maximum, max 76 h) versus 8 h (min 3 h; max 340 h); p = 0.004), shorter stay in intensive care unit (ICU) (2 days (minimum 1 day; maximum 25 days) versus 4 days (min 1 day; max. 35 days); p = 0.031) and reduced transfusion requirements (26.5% vs. 56.0%; p = 0,004). Total length of hospital stay as well as postoperative pain levels were comparable (14).
In a study by Snegirev et al. (24) ministernotomy was accompanied by longer cardiopulmonary bypass and aortic cross-clamp times, but did not affect mortality, however there less bleeding and less transfusion requirement in ministernotomy group.
Conclusion
As a result of reviewing and studying the studies, it can be concluded that the replacement of the aortic valve with minimally invasive methods is more effective. The data obtained on the use of multidetector computed tomography will make it possible to determine the optimal surgical access as accurately as possible. This will reduce the intraoperative time, the duration of artificial circulation and reduce postoperative complications. It should be noted that the postoperative condition of the patient, the fastest recovery, the reduction of physical limitations and pain syndrome also plays a significant role in treatment.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: A.K.T., T.Z.K. contributed equally to the preparation of manuscript
Acknowledgement and Funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Afternoon around the castle of Vorselaar 2022. Christiaan Vrints, Antwerp, Belgium.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

