Efficacy of shockwave C2 coronary intravascular lithotripsy for management of severely calcified left anterior descending stenosis
CASE REPORT
Efficacy of shockwave C2 coronary intravascular lithotripsy for management of severely calcified left anterior descending stenosis
Article Summary
- DOI: 10.24969/hvt.2022.321
- Page(s): 96-99
- CARDIOVASCULAR DISEASES
- Published: 08/06/2022
- Received: 20/04/2022
- Revised: 31/05/2022
- Accepted: 02/06/2022
- Views: 6239
- Downloads: 4722
- Keywords: Calcifications, drug eluting stent, intravascular, lithotripsy, outcome, coronary artery disease
Address for Correspondence: Sanjay Kumar Sharma Department of Cardiology, Neo Hospital, Noida-201301, Uttar Pradesh, India. Phone: +91-9810286407 Email: drsanjukgautam@hotmail.com
Sanjay Kumar Sharma, Department of Cardiology, NEO hospitals, Noida-201301, Uttar Pradesh, India
Abstract
Severely calcified coronary lesions remain a formidable hurdle for percutaneous coronary intervention as it averts the stent delivery and complete stent apposition. To overcome this Achilles heel of an interventional cardiology, a current US FDA approved method named shockwave intravascular lithotripsy (S-IVL; Shockwave Medical, Inc) is used for its treatment. Herein, we report a case of a 53-year-old dyslipidemic male with severely calcified left anterior descending artery (LAD) lesion that was successfully treated with S-IVL and drug-eluting stent implantation. At first, the patient was presented with complaints of chest pain and breathlessness. His coronary angiogram revealed heavily calcified stenosis in diffuse mid LAD—completely totally occluded mid diagonal 1 (D1) that was checked through retrograde filling via collateral and calcified stenosis in ostial D2, mild stenosis in ostial left circumflex and mild stenosis at distal before crux 50% stenosis in dominant right coronary artery. Following this, it was decided to proceed with primary percutaneous coronary intervention with S-IVL to LAD. After successful delivery of S-IVL to LAD, a Tetriflex sirolimus eluting stent (Sahajanand Medical Technologies Ltd., Surat, India) was successfully implanted at LAD. Finally, the patient’s condition was stabilized and discharged after two days of index procedure.
Introduction
Patients with calcified coronary lesions face an exaggerated clinical risk, as the calcification is linked to more widespread coronary atheroma and a larger burden of comorbidities. In addition, the treatment of these lesions poses a technical burden in percutaneous coronary intervention (PCI) because of the higher chance of inadequate lesion preparation with suboptimal stenting and increased incidence of acute and chronic in-stent restenosis (1). In clinical practice, plethora of techniques including balloon-depended and atherectomy devices have been employed for the appropriate preparation of calcified plaques prior to coronary artery implantation of drug-eluting stents (DES). Nonetheless, these techniques possess few complications (1, 2). To address these issues, a novel balloon-based coronary system for intravascular lithotripsy (IVL)-shockwave C2 intravascular lithotripsy (S-IVL) (Shockwave Medical Inc, Santa Clara, CA, USA), has been introduced for the defragmentation of calcium nodules.
Herein, we described our experience with IVL and DES implantation in a dyslipidemic male with severely calcified left anterior descending artery (LAD) lesion who had good angiographic outcomes.
Case report
A 53-year-old dyslipidemic male was admitted to the intensive care unit due to complaints of chest pain and breathlessness. On admission, his blood pressure was 119/74 mm Hg, pulse rate was 73 beats per minutes and oxygen saturation was 98% on room air.
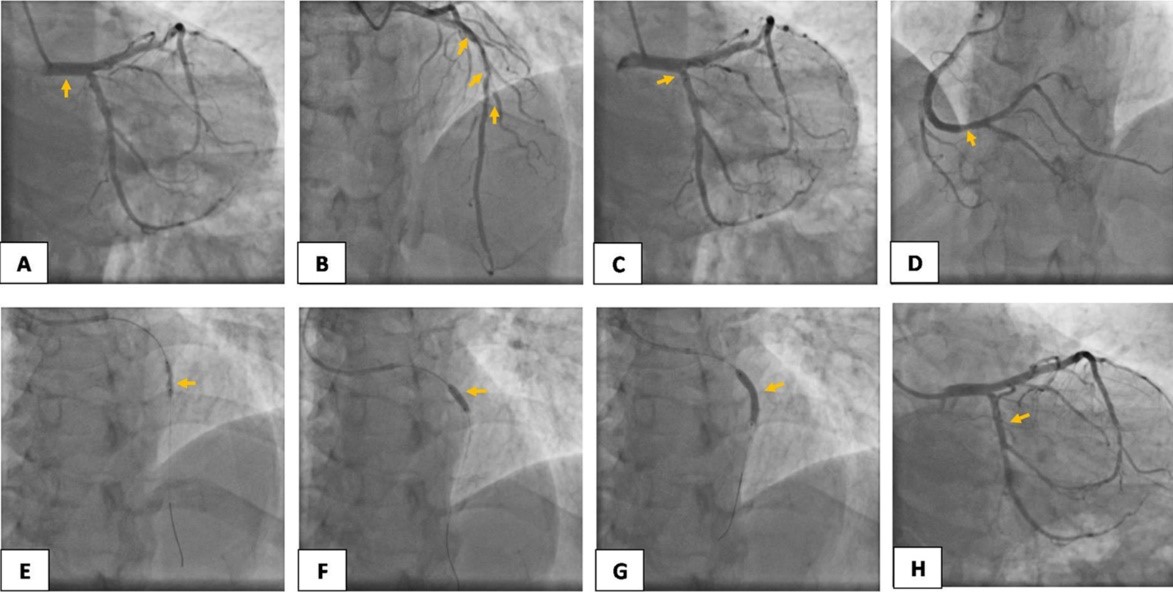
Figure 1. Coronary angiogram showing A) normal LMCA, B) 90% stenosis with heavy calcification in mid LAD, total occlusion in mid D1, 80% stenosis in ostial D2, C) mild diseases in ostial LCx- normal OM1 and OM2, D) mild diseases at distal before Crux 50% stenosis in dominant RCA- normal PDA/PLV, E) & F) wire was crossed and sequential IVL was done, G) A 3.5 x 24 mm Tetriflex stent was negotiated and deployed, and H) final post stent TIMI flow
D1- first diagonal, D2- second diagonal, DES- drug eluting stent, IVL- intravascular lithotripsy LAD- left anterior descending artery, LCx- left circumflex artery, LMCA- left main coronary artery, PCI- percutaneous coronary intervention, PDA- posterior descending artery, PLV- posterior lateral vein, OM1- first obtuse marginal artery, OM2- second obtuse marginal artery, RCA- right coronary artery
Echocardiography showed no regional wall motion abnormalities with 60% left ventricular ejection fraction, normal left ventricular or right ventricular systolic function, mild concentric left ventricular hypertrophy, trivial mitral and tricuspid regurgitations (normal pulmonary artery systolic pressure); no aortic regurgitation or aortic stenosis; mitral inflow pattern=A (late (atrial) diastolic transmitral flow velocity)>E (early diastolic transmitral flow velocity), intact inter-atrial septum/inter-ventricular septum; no left atrial or left ventricular clot, no pericardial effusion, and grade I-diastolic dysfunction. Angiogram revealed normal left main coronary artery (LMCA), 80-90% tubular respectively calcified stenosis with heavy calcification in diffuse mid LAD — 100% completely totally occluded mid diagonal 1 which was checked through retrograde filling via collateral and 80% calcified stenosis in ostial diagonal 2, mild stenosis in ostial left circumflex (LCx) — normal obtuse marginal branches (OM1 and OM2), mild stenosis at distal before crux 50% stenosis in dominant right coronary artery, and normal posterior descending artery (PDA)/posterior lateral vein (PLV). Following this, it was decided to do primary PCI with IVL to LAD. The LMCA was engaged with EBU guide catheter, and the LAD was crossed with BMW guide wire. Then, it was decided to proceed with IVL to assist adequate preparation of the calcified LAD lesion.
The lesion was predilated with non-compliant balloon (2.5×12 mm; 12 atm) that allowed a successful delivery of the shockwave C2 catheter (3.5×12 mm) to LAD. Following shockwave IVL, a 3.5x24 mm Tetriflex sirolimus-eluting stent (Sahajanand Medical Technologies Ltd., Surat, India) was negotiated and deployed at LAD. Post dilation was done with a 3.5 x10 non-compliant balloon at 22 atm. TIMI III flow of the related artery was achieved without residual stenosis. Patient was then hemodynamically stable throughout the procedure and discharged after two days of index procedure.
Discussion
The optimal coronary stent implantation remains a problem in the patients with severe calcifications. Proper lesion preparation prior to stenting is essential to minimize severe procedural issues.
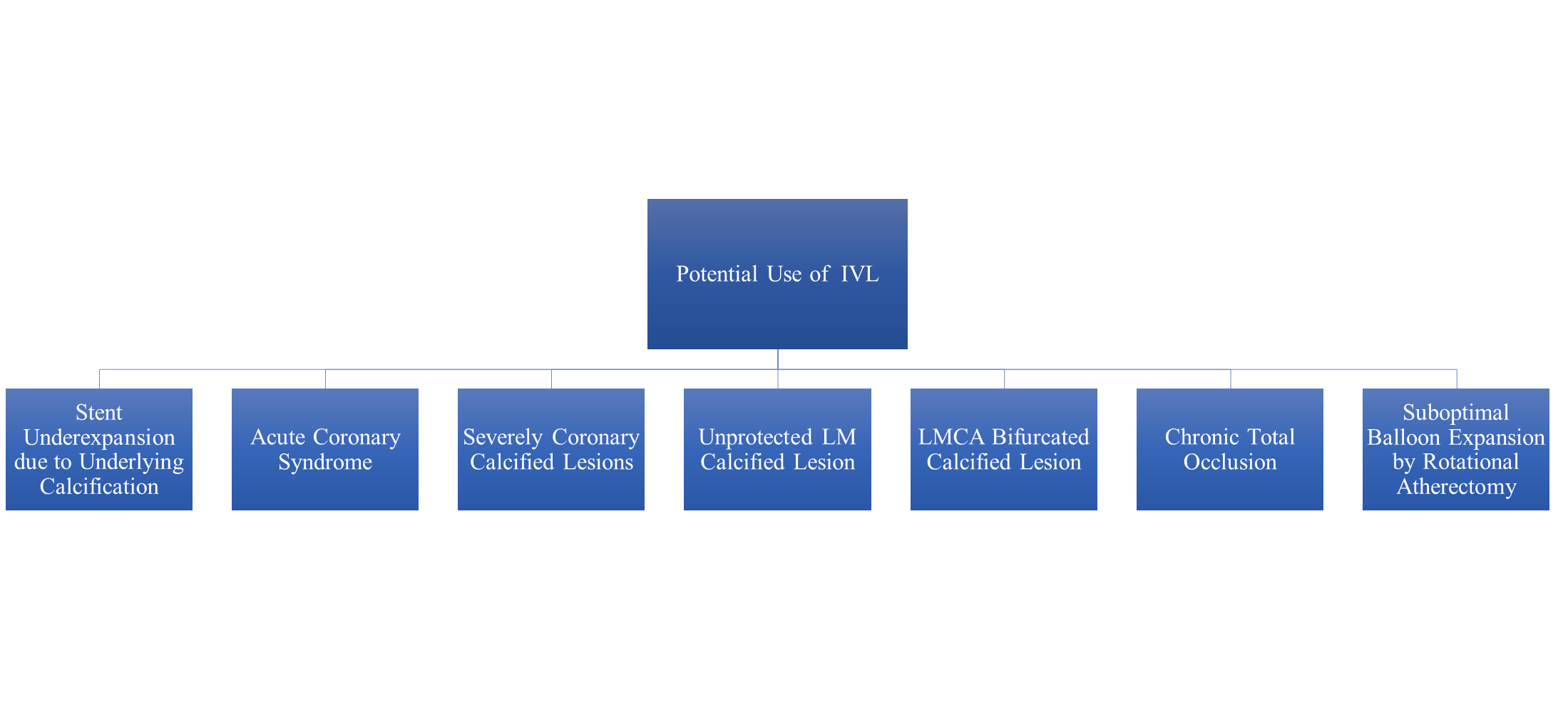
Figure 2. Potential use of intravascular lithotripsy
IVL- intravascular lithotripsy, LMCA - left main coronary artery, LM - left main
The non-compliant, scoring or cutting balloon and rotational atherectomy are used to dilate calcified lesion in clinical practice; nevertheless, these modalities are occasionally constrained by inadequate stent expansion and apposition (3, 4). The S-IVL has been proved to be superior to aforementioned conventional modalities for the treatment of coronary artery calcifications (4).
The S-IVL produces pulsatile sonic pressure waves that are converted to mechanical energy via a balloon inflated in the coronary vessel, which may alter vascular calcium by inducing calcium fractures, thereby permitting appropriate stent expansion (5). The S-IVL offers following benefits when compared to traditional atherectomy:
1) This device does not necessitate specific training because it is delivered similar as standard catheter-based PCI.
2) S-IVL, being a balloon-based device, may lower the peril of atheromatous embolization.
3)Modification of calcified plaque with the aid of S-IVL is not affected by the guidewire bias. Sonic pressure waves produced by this device are equally spread throughout the lithotripsy emitter, tackling calcified lesion regardless of its circumferential existence.
4) In contrast to traditional balloon technology that relied on high-static barometric pressure for vessel
preparation, the S-IVL provides circumferential ultra-short pulses of high-intensity acoustic energy that could last less than two μs in a balloon inflated at low pressures, leading to reduce mechanical vascular trauma and offers appropriate and efficient circumferential modification of calcific atheroma.
5) S-IVL may allow the side-branch protection with the help of a guidewire, avoiding the likelihood of wire entrapment or severing that can emerge while using rotational or orbital atherectomy (6, 7).
However, the S-IVL possess a few complications that are categorized into two categories: a) procedural complications (slow flow, lack of reflow, distal embolization, perforation, and arterial dissection), and b) post-procedural complications (major cardiac adverse events (MACE) include death, myocardial infarction, and coronary revascularization) (8).
The safety and feasibility of S-IVL for remodeling of severely calcified coronary vessels was validated by Disrupt Coronary Artery Disease (CAD) I study (6), Disrupt CAD II study (7), Disrupt CAD III study (9), Disrupt CAD IV study (IV) (10) and Lower-Silesia Shockwave Registry (LSSR) (2). The outcomes of these studies and registry exhibited that the lithoplasty balloon-based therapy resulted in 98% device success and facilitated 100% stent delivery with low rates of significant adverse cardiac events and minor vascular sequelae.
Despite overwhelming clinical evidence with promising outcomes, there is a lack of convincing clinical evidence in the Indian context. To the best of our knowledge, this is the first case of severely calcified stenosis of LAD lesion successfully treated with S-IVL in dyslipidemic Indian patient. Previous researchers had found that coronary artery calcification worsens with age and is more frequent in men than in women. In addition, people with dyslipidemia are more likely to develop coronary artery calcification (11), which is in consistent with our case. The higher incidence of dyslipidemia in India may be related to the lack of information about the significance of exercise, poor diet habits, and limited access to healthcare and genetic susceptibility. Furthermore, S-IVL outperformed the conventional approaches with its improved clinical success rates in the event of stent under expansion (12, 13). Legutko et al. also performed successful S-IVL for a severely calcified and undilatable LAD lesion in a patient with recurrent myocardial infarction (4). Similarly, Pineda et al. discovered that the efficacy of S-IVL for the treatment of severely calcified LAD stenosis was confirmed in optical coherence tomography (OCT), which showed a considerable increase in acute area gain and satisfactory stent expansion (14). However, in the present case, due to the unavailability of intravascular ultrasound or OCT at our center, we had not performed any advanced invasive imaging modality after S-IVL.
Moreover, S-IVL was demonstrated to be feasible approach for treating femoroiliac stenosis and allowing the introduction of a transfemoral Impella CP (15). The potential use of S-IVL is delineated in Figure 2.
Thus, in line with all previous studies, our case has shown that S-IVL may be an appealing modality for the management of severely calcified complex lesions, specifically in the context of increased calcified burden in the elderly population.
Conclusion
This case illustrates an example of successful S-IVL to facilitate stent expansion in a dyslipidemic patient with severely calcified LAD stenosis.
Ethics: Written patient consent form was obtained.
Peer-review: internal
Conflict of interest: None to declare
Authorship: S.K.S. has contributed to the preparation of manuscript and management of patients
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

