Anatomical risks and complications associated with myocardial bridging
ORIGINAL RESEARCH ARTICLE
Anatomical risks and complications associated with myocardial bridging
Article Summary
- DOI: 10.24969/hvt.2022.331
- Page(s): 108-114
- CARDIOVASCULAR DISEASES
- Published: 30/07/2022
- Received: 03/06/2022
- Revised: 25/07/2022
- Accepted: 26/07/2022
- Views: 9593
- Downloads: 4742
- Keywords:
Address for Correspondence: Rupali Mahajan B, Department of Anatomy, Lokmanya Tilak Municipal Medical College, Mumbai - 400022, Maharashtra, India. Mobile: +91 88058 79733 E-mail: rmsmbt1@gmail.com
Rupali Mahajan B, Preeti Meshram, Nisha Vinod Ranadhir, Shantha Hattangadi
Department of Anatomy, Lokmanya Tilak Municipal Medical College, Mumbai, Maharashtra, India
Abstract
Objective: Myocardial bridging (MB) is an asymptomatic, benign, and congenital coronary anomaly with several possible manifestations. MB is formed by a segment of a coronary artery taking an intra-myocardial course. As of date, huge knowledge gap exists in the literature in terms of MB and its associated complications.
Methods: This single-centre, observational, non-randomised study was conducted over a period of 20 months to identify the rare anomalies such as MB using coronary angiograms.
Results: Eight of 400 cases screened have been found to have MB bridging in mid left anterior descending artery (LAD) segment. The male to female ratio was 7:1 all within an age range of 24 years to 45 years. Most of the patients were asymptomatic with no history of drug usage (6/8) and family history (3/8) of coronary disorders. In symptomatic cases, the most common presenting symptoms were observed to be typical chest pain, dyspnea, nausea, light-headedness, or headaches, diaphoresis, and tachycardia. In most of the patients, MB showed systolic shortening with resultant flow limitation on coronary angiography. The segments were reported to be 1 mm to 10 mm in size and traversed 1 cm to 3 cm length. All the patients were treated symptomatically and were kept on follow-up. No mortality was observed in any case with MB.
Conclusion: Even though MB is a benign condition, but its vast array of related complications was reported to be life threatening and require prompt diagnosis and treatment. This study focus on such MB related risks by highlighting the importance of differential diagnosis and the treatment followed by to avoid all possible complications in all those patients presenting with possible signs and symptoms.
Key words: Coronary vessel anomalies, coronary angiography, myocardial bridging, tunnelled artery, left anterior descending artery
Introduction
Myocardial bridging (MB) is a congenital coronary anomaly reported first by Reyman (1) in 1737 (2, 3). After two centuries for the first time, Geringer (1951) (4) described it in detail, Portsmann and Iwig (5) explored angiographically (1960), and Binet et al. (6) (1975) managed it surgically with myotomy. With the advancement of newer diagnostic modalities and techniques such as fractional flow reserve (FFR), intracoronary Doppler, intravascular ultrasound (IVUS), and coronary computed tomographic angiography (CCTA) have enabled the anatomic and physiologic evaluation of the coronary artery, systolic compression, and pathological effects on coronary flow in detail (3,7).
To be precise, the encasement of coronary arteries by a myocardium tissue is referred as “myocardial bridging” and the artery running within the myocardium is referred to as a “tunnelled artery” (3, 8–14). The prevalence range was largely varied and reported between 0.004% to ~85% and noted mostly on coronary angiography and autopsy (9, 13). The pathophysiological mechanisms leading to MB include Venturi-like effect, branch steal mechanism, accelerated atherosclerosis, and supply demand mismatch, etc. (3). This anomaly is generally confined to the mid LAD (~67% to ~98%),(15) but it also involves epicardial artery and/or secondary branches, especially the septal perforators (14, 15). It is mostly benign and asymptomatic with possible risk of clinical complications and unexpected risks such as transient ventricular dysfunction, exercise-induced atrioventricular conduction blocks, arrhythmia, ventricular dysfunction/stunning, acute coronary syndrome, early death after cardiac transplantation, ischemia and acute coronary syndromes, angina, and sudden death (16, 17).
Among the multiple invasive and non-invasive diagnostic modalities available, many centres around the world still prefer to use conventional coronary angiography (invasive) for structural and functional assessment of the MB. It was also reported that the detection rate of MB was relatively low using angiography but still is largely used and preferred because of its multiple advantages such as wide access, portability, low radiation, and low cost. However, recent guidelines encourage invasive methods, especially when non-invasive tests suggest that person is having symptoms that make a heart or coronary artery problem very likely or there is a blood vessel or heart problem (18). One more advantage of invasive methods is that during the test, doctors can also treat various diseases, including coronary artery disease. Typical findings to diagnose MB using these invasive methods such as cardiac catheterization and coronary angiography include systolic narrowing or “milking” of the epicardial artery and a “step down – step up” phenomenon that helps to identify the tunnelled segment rather than direct visualization. Still the debate about MB and its related myocardial problems is an unresolved question.
Always to avoid any such complicated situations, clinical suspicion should remain high for MB in all cases of typical and atypical chest pain, especially in young patients without any coronary risk factors. Other indications to consider coronary angiography in young patients include family history of cardiac diseases, episodes of arrhythmia, comorbidities associated with ischemia like presentations, echocardiography findings suggestive of segmental hypokinesia, high levels of cardiac enzymes during episodes of chest pain, and electrocardiographic (ECG) findings suggestive of ischemia.
Treatment of patients with MB should also be exclusively considered based on the risk factors and symptomatology. It is not yet known how MB contributes to cardiac morbidity and prognostic outcomes in cardiac patients. The treatment is now entirely dependent on the severity of haemodynamic disturbance compromising cardiac function, and depth of MB. Currently, medication is accepted as a first-line of therapy, while surgical de-roofing and coronary artery bypass graft (CABG) are reserved for severe stenosis. Some clinicians even claim MB as a normal variant of coronary artery anatomy due to absence of any conclusive evidences (19).
As of date, multiple MB case reports are published in the literature but data related to multiple cases are limited.
To minimise such knowledge gaps to the existing data, clinical characteristics, coronary anatomies and primary anomalies (MB) were studied in a large group of patients using angiography and its related outcomes were reported and reviewed in our study. This study will also help in understanding the MB and its related rare events of cardiac morbidity and mortality by strongly accounting the importance of differential diagnosis of typical and atypical chest pains, especially in young patients.
Methods
This single-centre, observational cohort study was conducted at Lokmanya Tilak Municipal Medical College and General Hospital, India over a period of 20 months. All the necessary approvals were cleared from Institutional Ethical committee prior to study initiation. An informed consent was obtained from all the subjects, prior to their participation in the study. After collection of data from the patients and from catheterization laboratory, the patients were divided into patients with angiograms having normal coronary artery anatomy (392/400) and abnormal coronary (8/400) artery anatomy.
All the patients demographical, clinical, and laboratory data was collected: age, sex, medical history, clinical presenting symptoms, socio-economic class, risk factors (smoking, obesity, dyslipidaemia, diabetes mellitus, and family history of coronary artery diseases), body mass index, blood pressure, pulse rate, ECG, creatine phosphokinase-MB (CPK-MB), complete blood count (CBC), lipid profile, high-sensitivity C-reactive protein (hs CRP), renal and liver functionality, electrolytes, natriuretic peptides, and troponins.
All patients underwent coronary angiography. A total of 400 patient’s coronary angiograms were identified, analysed, and clinically correlated using Philips Allura - Xcelera Dicom Recorder data system for coronary angiogram (CAG).
Statistical descriptive data are represented as numbers.
Results
Out of 400 cases examined, 8 cases were identified to have myocardial bridging in mid LAD segment (Fig. 1). Baseline demographic characteristics, ECG and echocardiography data of the patients are presented in Table 1. Seven of eight were male within an age range of 24 years to 45 years. Six of eight patients denied any medication or drug usage and two reported occasional drinking habit. Three of eight patients had family history of coronary disorders, 2 patients had hypertension and diabetes.
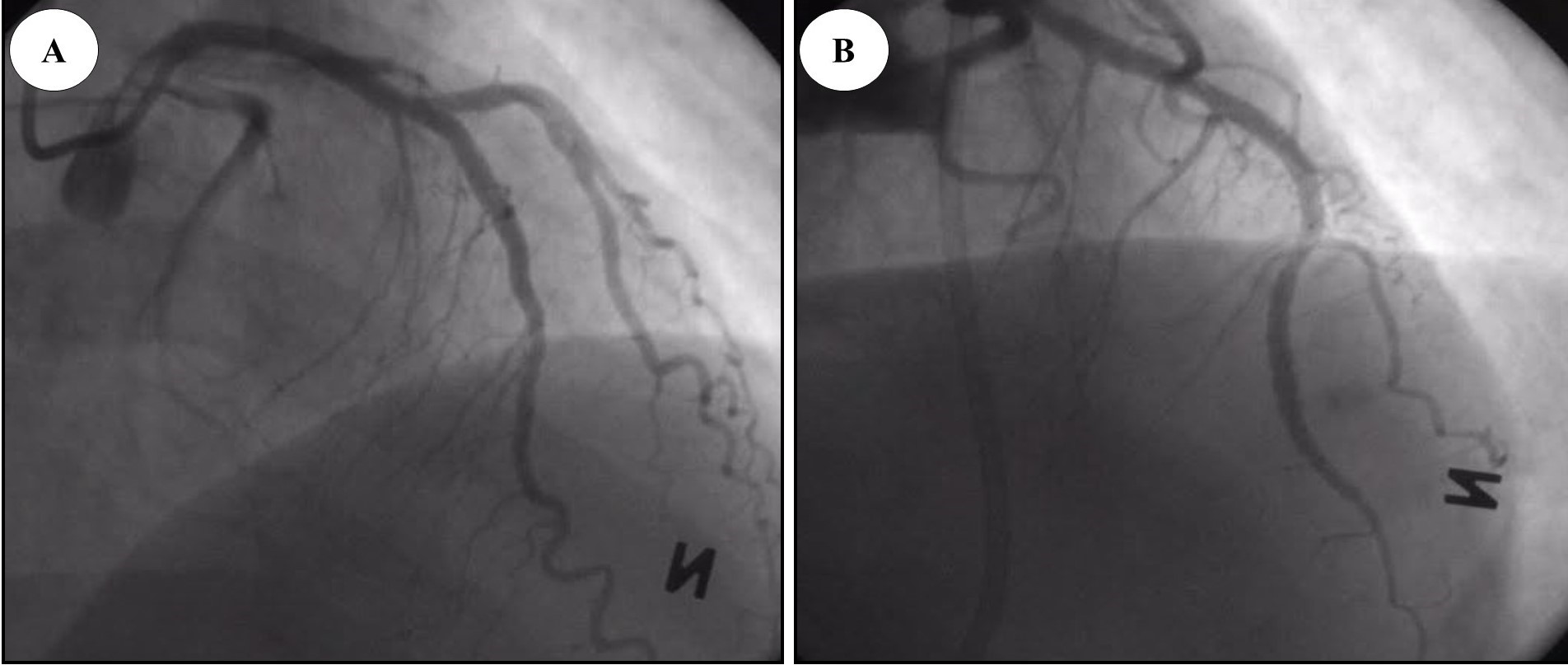
Figure 1. Mid left anterior descending artery myocardial bridging (A & B)
|
Table 1. Baseline demographic characteristics of patients |
||||||||||||
|
Variables |
Patient 1 |
Patient 2 |
Patient 3 |
Patient 4 |
Patient 5 |
Patient 6 |
Patient 7 |
Patient 8 |
||||
|
Sex |
M |
M |
M |
M |
M |
M |
M |
F |
||||
|
Age |
24 |
30 |
34 |
45 |
39 |
36 |
38 |
42 |
||||
|
Socio-economic status |
LMC |
UMC |
LMC |
LMC |
UMC |
LMC |
LMC |
LMC |
||||
|
Smoking |
Yes |
No |
No |
No |
Yes |
Yes |
Yes |
No |
||||
|
Alcohol |
Yes |
No |
No |
No |
Yes |
No |
No |
No |
||||
|
Family history of coronary artery disease |
Yes |
No |
No |
No |
Yes |
No |
No |
Yes |
||||
|
Hypertension |
No |
Yes |
No |
No |
Yes |
No |
No |
No |
||||
|
Diabetes mellitus |
No |
No |
Yes |
No |
No |
Yes |
No |
No |
||||
|
Dyslipidemia |
Yes |
No |
No |
No |
No |
Yes |
No |
No |
||||
|
ECG |
Sinus tachy |
Non-specific ST-T changes |
ERP with sinus tachy |
ST-T changes in inferior leads |
Non-specific ST-T changes |
ERP with sinus tachy |
ST-T changes in anterior lead |
Sinus tachy |
||||
|
Presenting complaints |
||||||||||||
|
Chest pain |
Mild |
Mild |
Moderate |
Moderate |
Atypical patterns |
Moderate |
Moderate |
Mild |
||||
|
Dyspnoea |
Yes |
Yes |
No |
No |
No |
Yes |
No |
No |
||||
|
Palpitations |
Yes |
No |
No |
No |
No |
Yes |
No |
Yes |
||||
|
Sweating |
No |
No |
Yes |
No |
No |
No |
Yes |
Yes |
||||
|
Nausea |
No |
No |
No |
No |
No |
No |
No |
Yes |
||||
|
Echocardiography |
||||||||||||
|
Regional WMA |
Yes |
No |
No |
Yes |
No |
No |
No |
Yes |
||||
|
Ejection fraction |
60 |
65 |
65 |
60 |
55 |
65 |
60 |
45 |
||||
|
ECG – electrocardiogram, ERP - early repolarization pattern, LMC –lower middle class, tachy –tachycardia, WMA – wall motion abnormalities, UPM – upper middle class |
||||||||||||
Dyslipidemia was found in one patient. Presenting symptoms in most of the patients were dyspnea, recurrent episodes of oppressive retrosternal pain with radiation to the interscapular region, typical chest pain, nausea, lightheadedness, or headaches, diaphoresis, and tachycardia. ECG was characterized by presence of sinus tachycardia and ST segment changes, 2 patients had wall motion abnormalities and 1 patient had reduced ejection fraction on echocardiography.
Angiographic data are presented in Table 2. Non-obstructive coronary artery disease was revealed in 2 patients, other had intact coronary vessels in terms of stenosis. MB was registered in mid LAD in all patients. In most of the patients, MB showed systolic shortening with resultant flow limitation. The segments were 1 mm to 10 mm in size and traversed 1 cm to 3 cm length. All the symptomatic patients were treated as per protocols (symptomatic treatment) and were kept on follow-up. No mortality was observed in cases with MB.
|
Table 2. Angiography findings |
||||||||||||
|
Pt |
Number of ostia |
Diameter of main trunk |
Level of termination |
Branches to |
Origin of PDA |
Domi-nance |
SPECIAL |
CAD |
||||
|
RCA |
LCA |
RCA |
LAD |
RCA |
LAD |
SAN |
AVN |
|||||
|
1 |
1(RT CUSP) |
1(LT CUSP) |
4.2 |
5 |
At right border |
III |
LCA |
LCA |
LCA |
Left |
Mid LAD MB |
Nil |
|
2 |
1(RT CUSP) |
1(LT. CUSP) |
4.2 |
4.5 |
At right border |
III |
LCA |
LCA |
LCA |
Left |
Mid LAD MB |
Nil |
|
3 |
1(RT CUSP) |
1(LT CUSP) |
4.5 |
5.4 |
Beyond crux |
III |
RCA |
RCA |
RCA |
Right |
Mid LAD MB |
Nil |
|
4 |
1(RT CUSP) |
1(LT CUSP) |
3.1 |
4.5 |
At crux |
III |
RCA |
LCA |
RCA + LCA |
Co-domi-nance |
Mid LAD MB |
Non obstru-ctive CAD |
|
5 |
1(RT CUSP) |
1(LT CUSP) |
3.5 |
5.1 |
At right border |
III |
RCA |
RCA |
RCA + LCA |
Co-domi-nance |
Mid LAD MB |
Nil |
|
6 |
1(RT CUSP) |
1(LT. CUSP) |
4.5 |
5.5 |
Before right border |
II |
LCA |
LCA |
LCA |
Left |
Mid LAD MB |
Nil |
|
7 |
1(RT CUSP) |
1(LT CUSP) |
3.5 |
4.5 |
At crux |
III |
RCA |
RCA |
RCA |
Right |
Mid LAD MB |
Nil |
|
8 |
1(RT CUSP) |
1(LT. CUSP) |
4.3 |
5.1 |
Before right border |
II |
LCA |
LCA |
LCA |
Left |
Mid LAD MB |
Non obstru-ctive CAD |
|
AVN - atrioventricular node, CAD - coronary artery disease, LT– left, RT – right, RCA - right coronary artery, LCA – left coronary artery, LAD - left anterior descending artery, MB- myocardiial bridge, SAN - sinoatrial node, PDA - posterior descending artery, Pt - patient |
||||||||||||
Discussion
Although MB is benign, but its involvement in various cardiac related issues is still a question for debate and to be concerned off (17). Possible mechanism behind such risks associated with MB can be due to the tunneled artery and its associated disturbances in the blood flow. It was also evidently observed from multiple cases that MB is benign and normal until the myocardial compression happens on the vessels leading to disturbance in blood flow and worsening of symptoms. Its severity was observed to be fatal with increase in age, co-morbidities, and inactive life style. Such disturbance of blood flow to the rest of the myocardium mainly occurs during systole and is resolved in the diastolic phase (9). This transient hypoperfusion was noted to be the main cause for all the cardiac related issued due to MB. In these patients with MB in the LAD, an increased amount of oscillatory wall shear stress was reported due to the inherent nature of the tunneled artery and its related vasospasms.
Due to this mechanical trauma to the vessel wall, increase in overexpression of pro-atherogenic endothelial cells, reactive oxygen species production, and vascular cell adhesion molecules was noted. Which may lead to stimulation of cells to injure endothelial cells and plaque formation leading to multiple fatal disorders such as ischemia, dysrhythmias, chest pain, and death in rare cases.
Effort-induced tachycardia is another cause for severe complications in patients who do strenuous exercises, where such high physical activity increases flow velocity, contractility, myocardial oxygen demand due to reduced coronary flow. As observed in our patient cohorts, in patients presented with MB in LAD can be an another major risk factor for ≥ 50% coronary artery stenosis in proximal LAD, with or without co-morbidities such as hypertension. During exercise or extreme stressful activity, ischemia is mediated by effort-induced tachycardia, which increases myocardial oxygen demand, contractility, and flow velocity causing reduce in coronary blood flow (4, 5). At this point, due to the increased compression of the tunneled artery (‘milking’) during systolic phase, retrograde flow at the proximal segment of the myocardial bridge is observed and anterograde flow is significantly hampered eventually leading to increased risk of sudden ischemia of that specific region of coronary circulation (9, 10, 14, 22). MB are also known to have higher propensity to develop atherosclerosis in coronary arteries. MB milking might also cause ischemia by an ‘branch steal’ or ‘intramural steal’ mechanism linked to decreased perfusion pressure of the blood suction and septal branches. In some studies, MB was also shown to be a protective (23, 24) or predictive (25–27) factor of atherosclerosis. Especially, proximal segment of the bridge was considered to be a major risk factor of atherosclerosis (23, 24, 26, 27).
Overall, MB related symptoms and complications are observed to be highly dependent on various clinical and pathophysiological factors such as age of the patient, degree of systolic narrowing, hear rate or diastolic perfusion time, intrinsic and extrinsic factors (coronary vasoconstriction, sympathetically driven myocardial contraction, transmural perfusion gradients, diastolic flow, arterial/myocardial compression, and aortic pressure), biochemical factors (led to intimal injuries developing into coronary dissection, vasospasticity, and plaque vulnerability/thrombosis), number of tunneled segments, depth of tunneled artery, presence of coronary atherosclerosis, left ventricle (LV) hypertrophy, and the length of the tunneled artery or location of the bridge (21).
In the end in asymptomatic patients with LAD MB, patients will be initially relieved from all potential triggers by modifying potential risk factors and along by considering antiplatelet therapy in patients with atherosclerosis. Whereas in symptomatic patients, standard of care will be given using pharmacological therapy (beta-blockers, calcium channel blockers, nitrates, ivabradine, anti-platelet therapy, etc), percutaneous coronary revascularization (PCI), myotomy, stents, or CABG (3, 13, 15, 21).
To avoid any possible risks in these MB patients, antiplatelet therapy was considered to avoid the risk of developing atherosclerosis. Other drugs were also used frequently to maintain the hemodynamic balance (beta-blockers), and vasodilatory effects (calcium channel blockers and nitrates) (28). Other treatment modalities were also considered based on the treatment goals such as reinforcing of intramural coronary artery (PCI), bypassing the compressed arterial segment (CABG), and removal of overlying MB (surgical myotomy) (11).
As most of the patients were asymptomatic and had no family history of coronary disease, our patients were treated medically. In future, it can be worth continuing to recruit patients and address issues of both medical and interventional, and possibly minimally invasive (transthoracic) methods of treatment. To determine the best treatment, long-term large randomized trials are needed, to identify and develop the best treatment strategy for patients with MB.
Study limitations
The key limitations include small number of patients, single-center study, non-randomized, observational nature of the study, where treatment options, and outcomes were not compared.
Conclusion
Till date multiple studies were conducted on MB, yet many questions remain unanswered. Extant literature indicates MB as a common, benign condition. However, recent studies have highlighted various clinical complications associated with MB and its role in the etiology of other cardiovascular conditions and increasing the risk of developing other diseases in the future. To avoid any such risks and life threatening situations, MB should be considered during the differential diagnoses in all the patients presenting with typical symptoms as discussed earlier.
If required, invasive and non-invasive diagnostic modalities should be considered to identify the pathophysiology of MB and symptomatic treatment should be initiated due to lack of any MB specified standard of care. To determine the best treatment approach, long-term large randomized trials are required to identify and elaborate the best treatment strategy for patients with MB.
Ethics: The authors declare that they have followed all the ethical guidelines for publication.
Ethical approval and consent to participate: Ethics committee approval (IEC/DISS/52/12) was received for this study from the Ethics Committee of Lokmanya Tilak Municipal Medical College and General Hospital, India.
Informed consent was obtained from all patients before procedures.
Peer-review: external and internal
Conflict of interest: None to declare
Authorship: Study concept and design: RM and SH. Acquisition of data: RM. Analysis and interpretation of data: RM and SH. Drafting of the manuscript: RM. Administrative, technical, and material support: PM, NVR, and SH. Statistical analysis: RM and SH. Study supervision: SH.
Acknowledgements: the authors would like to thank Dean of the institute, colleagues, and all the participants contributed to our work.
Funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

