Answer to the Quiz: Imaging and case discussion
QUIZ
Answer to the Quiz: Imaging and case discussion
Article Summary
- DOI: 10.24969/hvt.2022.334
- Page(s): 155-159
- Published: 21/08/2022
- Received: 31/07/2022
- Revised: 18/08/2022
- Accepted: 18/08/2022
- Views: 4589
- Downloads: 4490
- Keywords:
Address for Correspondence: Yuriy Ivaniv, Department of Diagnostic Radiology
Danylo Halytsky National Medical University, Lviv, Ukraine Email: yivaniv@gmail.com
Answer to Quiz –Imaging on page and case discussion: A patient with heart failure symptoms and continuous murmur
Correct answer is sinus of Valsalva aneurysm dissecting interventricular septum with rupture into the right ventricle
Transthoracic echocardiography (TTE) showed normal left ventricular systolic function (ejection fraction - 65%), left ventricular hypertrophy (interventricular septum 1.5 cm, posterior wall 1,5 cm), left atrial dilatation (4.8 cm), right ventricular dilatation (3.2 cm), normal left ventricular end-diastolic diameter (5.2 cm) and a cystic-like structure (aneurysm) in the right ventricle adjacent to the interventricular septum (see Fig. 1, 2 – p. XX), located from the base of the septum to its mid-ventricular portion. In color Doppler imaging, turbulent flow was seen from the aorta into the aneurysmatic sac and from its cavity into the right ventricle (RV) (see Fig. 1, 3 pXX). Continuous-wave Doppler revealed continuous high-velocity flow from the aorta into the aneurysm and from its cavity into the RV during both phases of the cardiac cycle (systole and diastole) (see Fig. 4 – page XX). The estimated Qp/Qs ratio was 1.54. Systolic pulmonary artery pressure was 60 mm Hg. Aortic valve was tricuspid with mild regurgitation.
Right sinus of Valsalva aneurysm (SVA) with interventricular septum dissection and rupture into the RV was suspected. Contrast-enhanced multidetector computed tomography (MDCT) confirmed the diagnosis (Fig. 1, 2). Syphilis and other infections were excluded during differentiation between congenital and acquired sinus of Valsalva aneurysm. The patient had a fall from height 2 years earlier, which could be a trigger for rupture of his congenital malformation. Coronary angiography showed normal coronary arteries. Surgical repair of the aneurysm and dissection with a patch was performed successfully.
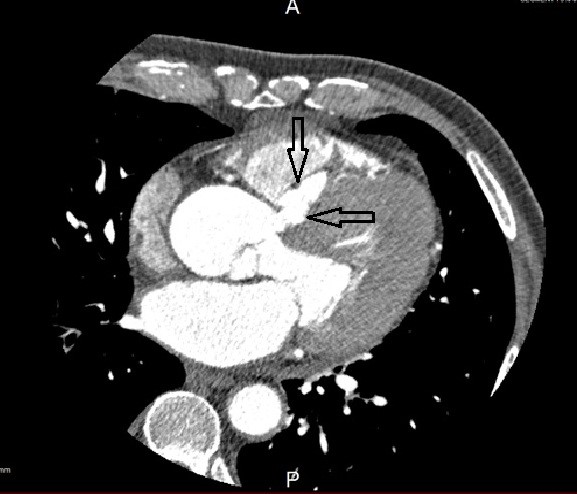
Figure 1. Multidetector computed tomography, arrows show the entrance orifice of sinus of Valsalva aneurysm with interventricular septal dissection
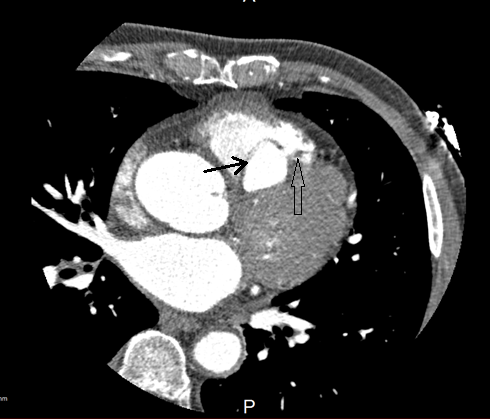
Figure 2. Multidetector computed tomography, black arrow shows the chamber of sinus of Valsalva aneurysm with interventricular septal dissection, empty arrow shows the outlet orifice into the right ventricle
SVA is a rare mostly congenital cardiac anomaly, caused by the defect in the aortic wall structure. The most common site of the SVA is the right coronary sinus (77 – 90%), followed by non-coronary sinus (in 10 – 22%) and left coronary sinus (1). Until rupture of an aneurysm occurs, echocardiography in SVA shows out-pouching of one of Valsalva sinuses, which could reach large dimensions and cause coronary artery compression, left or right ventricular outflow tract obstruction, interventricular septal (IVS) dissection, etc. (1)
The main complication of SVA is a rupture into a heart chamber, which causes its volume overload and leads to acute or progressive chronic heart failure (1-5, 7). Loud machinery continuous murmur along the left side of the sternum is a main clinical presentation of SVA rupture, as in the case of our patient (6). Since tachycardia with shortened diastolic duration often accompanies SVA rupture, it is sometimes difficult to distinguish between continuous and systolic murmur, as it was in our case. Thus, a spectrum of cardiac abnormalities needs differentiation, among which postinfarction IVS rupture with a systolic murmur is the most probable diagnosis. Other probable diagnoses are congenital IVS defect, coronary artery to heart chamber fistula (6).
Transthoracic echocardiography is a first-line method of diagnosis of SVA rupture. Color Doppler echocardiography reveals turbulent flow from aorta (from SVA) through the defect to the termination chamber. Continuous wave Doppler-echocardiography confirms its systolic and diastolic duration (1). Most SVA ruptures occur from the right coronary sinus aneurysm to the RV (67.9%), other entry sites of rupture are the right atrium (27, 4%), rarely the left atrium, the left ventricle, the pulmonary artery (1).
SVA rupture with IVS dissection occurs extremely rare (8–10). IVS dissection is diagnosed by echocardiography as an echo-negative cavity close to the IVS, which has an entrance orifice from SVA, and an outlet orifice in one of the heart ventricles (rarely both) (8-10). While an echolucent camera is easily detected by transthoracic echocardiography, more sophisticated methods of imaging (MDCT, cardiac magnetic resonance imaging, MRI) are needed for the visualization of entrance and outlet orifices. Gu et al., the authors of the largest cohort of patients with IVS dissection, reported 13 cases, the right SVA been the most frequent cause of the dissection (6 cases, 46% of patients) (9).
There is a need to distinguish SVA with IVS dissection and rupture into the right ventricle and postinfarction IVS rupture or congenital IVS defect, or coronary artery aneurysm and fistula
Congenital perimembranous IVS defects are often associated with IVS aneurysms presenting as thin membranous pouches that bulge from the margin of the defect. Such aneurysms arise from the IVS below aortic valve whilst SVA with IVS dissection arises from the sinus of Valsalva above the aortic valve. If we consider postinfarction IVS rupture, regional wall motion abnormalities are the hallmark of myocardial infarction. Postinfarction IVS rupture, which occurs in the basal inferior region, is a complication of aneurysmatic IVS thinning, in rare cases with IVS dissection or aneurysmatic bulging (11). But, similarly to congenital IVS defect, in postinfarction IVS rupture, the turbulent flow is seen in color Doppler-echocardiography from the left ventricle to the RV below the aortic valve annulus, and in the case of SVA rupture, as in our patient, it is detected from the aortic sinuses (or SVA) to the RV. Moreover, the duration of the turbulent flow is systolic in IVS rupture or congenital defect, and continuous systolic-diastolic in SVA rupture (as is seen in continuous-wave Doppler-echocardiography in our patient).
Coronary artery fistula (CAF) and aneurysm are the next entities to distinguish in our case. CAF produces continuous murmur, similarly to SVA rupture. More than 50% of CAF arise from the RCA and drain into a low-pressure structure, most commonly the RV (12). Termination of coronary artery to a low-resistance camera often causes aneurysmatic dilation of the artery, aneurysm occurs in 19-26% of CAF. In case of large CAF volume overload of the terminating camera causes heart failure symptoms (12). Transthoracic echocardiography is a first-line diagnostic method in the detection of CAF, especially in the case of a proximally dilated coronary artery. Color Doppler shows turbulent flow in the proximal portion of the dilated vessel around the aortic root. The main difference between CAF and SVA rupture is that TTE shows dilated and tortuous vessels at the level of the aortic root, and a bulging chamber in our case was located closely to IVS, intraventricularly. Finally, more sophisticated methods of imaging are needed, such as MDCT or MRI (12-14).
In conclusion, multimodality imaging with echocardiography and MDCT is the main diagnostic tool in SVA rupture diagnosis and assessment (14). Contrast-enhanced MDCT is used for verification of the SVA rupture diagnosis, especially in the case of IVS dissection, because it enables assessment of sinuses of Valsalva, interventricular septum, exact location of SVA entry orifice and location of its rupture. While cardiac MRI has a high resolution, it is less available and time-consuming procedure, so MDCT has advantages in SVA rupture imaging. Surgical resection is recommended as optimal care for ASV rupture. Surgical repair of SVA with rupture has low mortality rates and long-term survival is good (15).
Nelya Oryshchyn, Yuriy Ivaniv
Department of Diagnostic Radiology
Danylo Halytsky National Medical University, Lviv, Ukraine
Ethics: Informed consent was obtained from patient before procedures
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: N.O. and Y.I. equally contributed to case management and preparation of manuscript
Acknowledgement and Funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Glaciar Perito Moreno. Calafate. Santa Cruz. Argentina

Ushuaia, Beagle. Tierra del Fuego. Argentina
Santa Cruz and Tierra del Fuego aré two Provincias of south Argentina. Tierra del Fuego is known as the southernmost city in the world. Miguel Amor,
Buenos Aires, Argentina
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

