Unmasked type I electrocardiographic pattern of Brugada syndrome after SARS COV -2 (COVID 19) vaccine shot: Is there any relationship with the suspected increased risk of sudden death?
CASE REPORT
Unmasked type I electrocardiographic pattern of Brugada syndrome after SARS COV -2 (COVID 19) vaccine shot: Is there any relationship with the suspected increased risk of sudden death?
Article Summary
- DOI: 10.24969/hvt.2022.341
- Page(s): 209-213
- Published: 18/09/2022
- Received: 31/08/2022
- Revised: 12/09/2022
- Accepted: 13/09/2022
- Views: 5398
- Downloads: 4687
- Keywords: Brugada syndrome, COVID-19 vaccine, fever, unmasking, electrocardiogram type 1 pattern, sudden death
Address for Correspondence: Luis A. Arabia, Arrhythmia Unit, Instituto Oulton, Cordoba, Argentina
E-mail: luisarabi@hotmail.com
Luis A. Arabia
Arrhythmia Unit, Instituto Oulton, Cordoba, Argentina
Abstract
The vaccination used for the prevention of COVID-19 could unmask patients with hidden Brugada syndrome even without febrile episodes. We described a case of unmasking or Brugada syndrome in a female patient after vaccination for COVID-19. A possible relationship with sudden death events requires further study. In people with known Brugada syndrome or in their relatives, we recommend serial electrocardiographic monitoring after the administration of the vaccination dose.
Key words: Brugada syndrome, COVID-19 vaccine, fever, unmasking, electrocardiogram type 1 pattern, sudden death
Introduction
Patients with Brugada Syndrome (BrS) are at higher risk of events of malignant ventricular arrhythmias when they present with fever. The unmasking of the type I electrocardiographic pattern of BrS in patients with SARS COV 2 infection during the pandemic has been described(1). That is why in those patients with a previous diagnosis of BrS, presenting with COVID or febrile episodes due to vaccination, close observation is suggested, as well as the administration of antipyretics (2).
The number of people who received vaccines around the planet is enormous, and although it is very rare, it has been linked to death, including sudden death, but the causality of vaccination and death has not been fully proven (3).
We describe a case of unmasking or BrS in a female patient after vaccination for COVID-19.
Case report
We want to present a 38-year-old female patient who, after receiving her third dose of anti-SARS COV 2 (COVID 19), BNT162b2 COVID-19 (BNT) (Pfizer/BioNTech) vaccine, consulted for nonspecific discomfort on the third day, afebrile. She was clinically evaluated, with no pathological findings, her chest X-ray and laboratory tests were within normal limits, but her electrocardiogram (ECG) showed descending ST-segment elevation, suggestive of Brugada type I pattern (Fig. 1)
She was referred to a tertiary level center, arriving 21 days after vaccination with her ECG showing minimal changes in V1-V2.
In her medical records, she has a history of having neurocardiogenic syncope in adolescence, with positive tilt test. Due to a change in the pattern of syncopal episodes, an electrophysiological study was performed at the age of 15 years, inducing sustained syncopal monomorphic ventricular tachycardia, with possible origin in the right ventricular outflow tract (RVOT).
Due to absence of structural heart disease and no history of ventricular arrhythmia (neither personal nor family), it was considered a false positive and she was medicated with atenolol and an implantable loop recorded was implanted, with three years of follow-up, without documenting events of ventricular arrhythmia and the syncopal episodes were compatible with neurocardiogenic events. She has been lost to follow-up for 20 years until developed symptoms after vaccination.
Her mother died of cancer, and sister and father had no history of arrhythmia and their ECGs were normal. She was not taking any medications and had no history of COVID-19 infection.
Her ECG recorded in tertiary center and cardiac magnetic resonance imaging were normal. An electrophysiological study (EPS) and ajmaline test were performed, with the usual protocol (4).
EPS demonstrated no induction of complex ventricular arrhythmia, with reproducible induction of atypical sustained atrial flutter (Fig 2). Ajmaline test reproduced Brugada type I pattern (+) (Fig. 3- 4).
We referred the patient for genetic testing; if it will be negative we will follow-up and if positive - we will offer subcutaneous implantable cardioverter-defibrillator. We instructed the patient on medications that can induce arrhythmia and contraindicated in BrS.
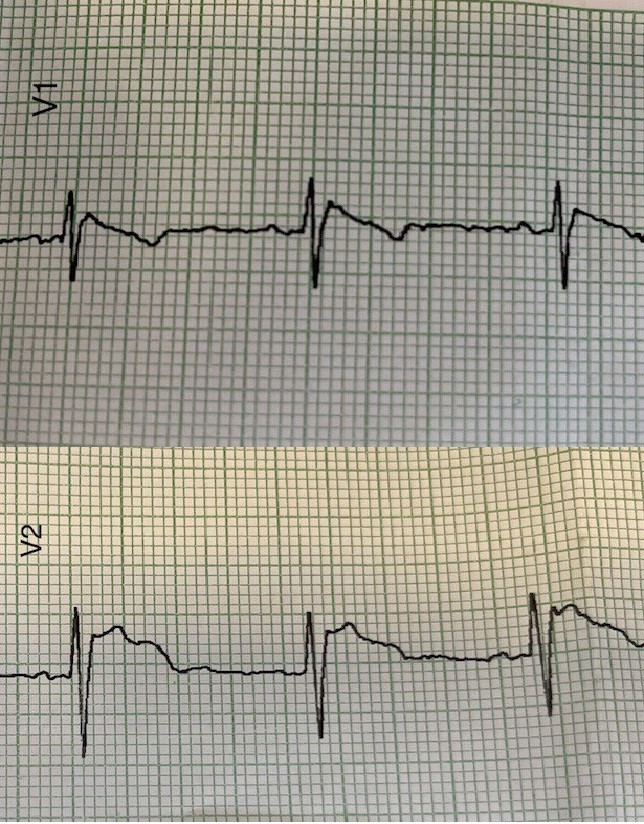
Figure 1. Electrocardiogram demonstrating Brugada type 1 pattern 3 days after vaccination
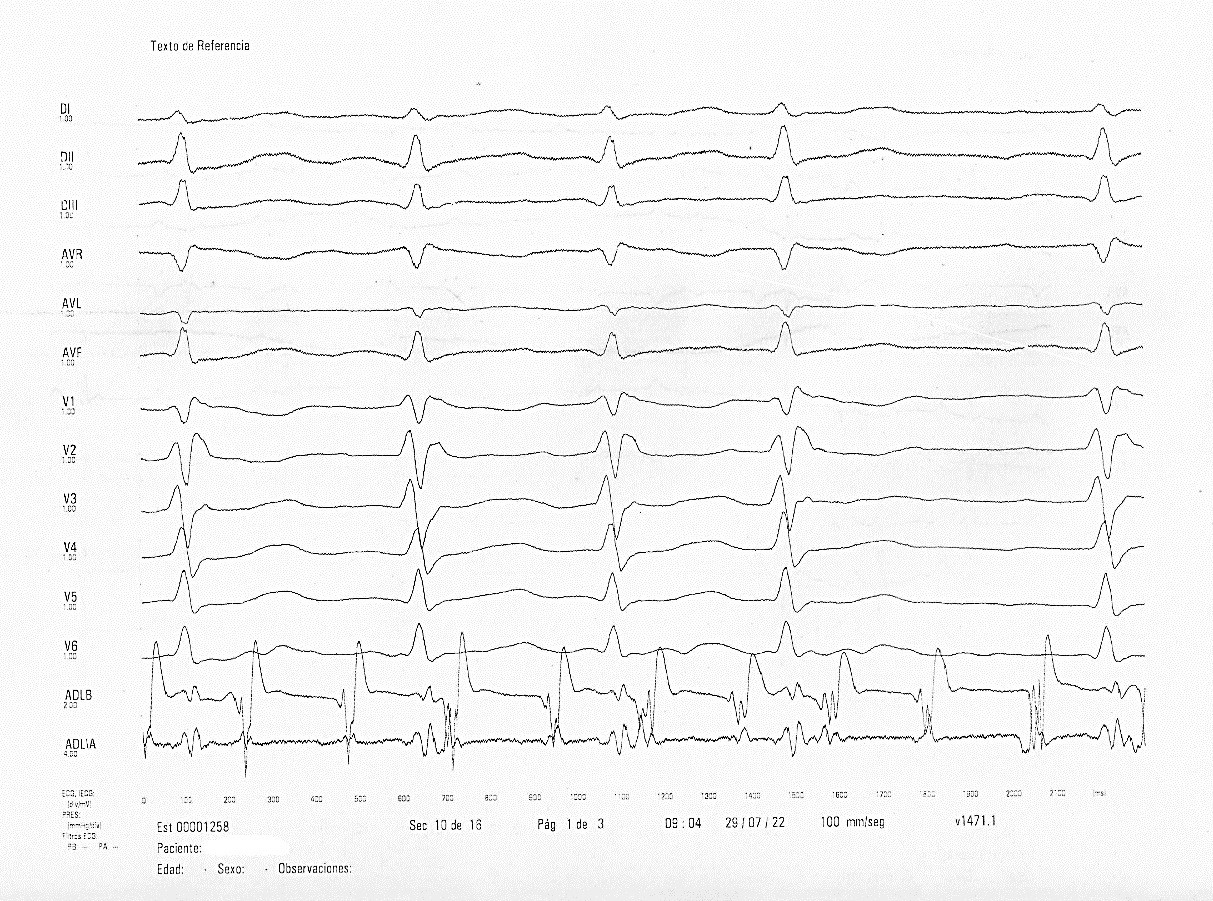
Figure 2. Atrial flutter induced during electrophysiological study
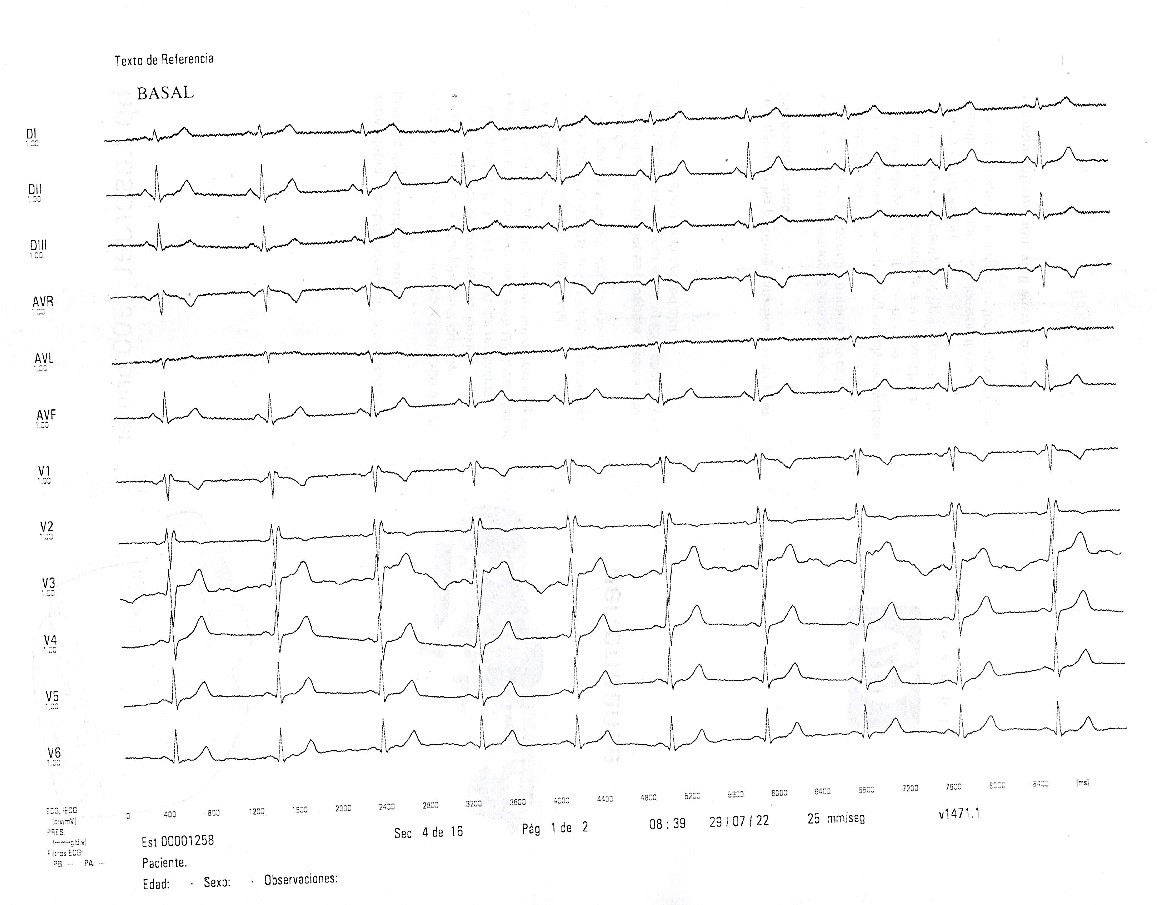
Figure 3. Ajmaline test. Baseline recording. Electrocardiogram speed 25 mm/sec. 21 days after vaccination.
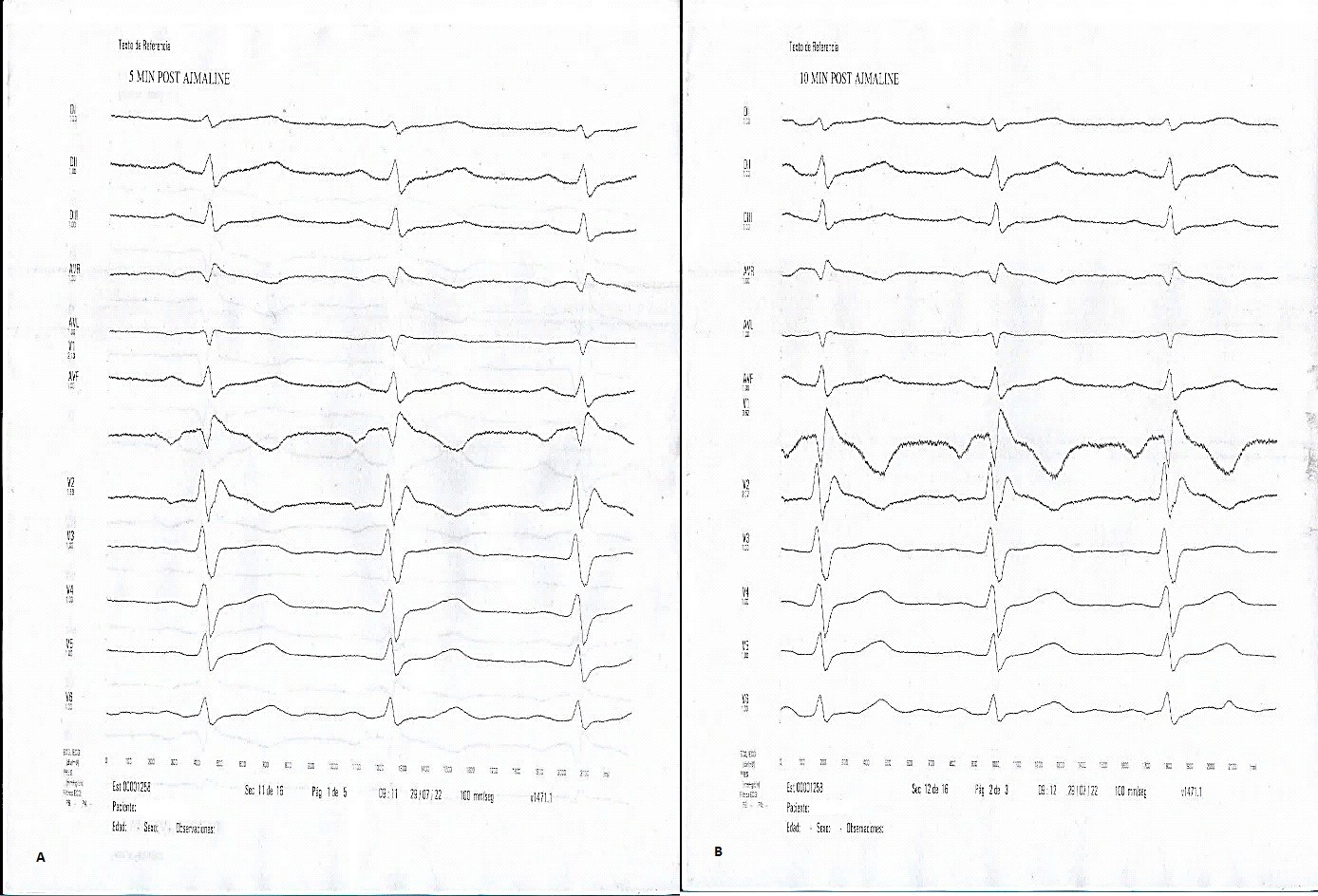
Figure 4. Ajmaline test recording demonstrating Brugada type I pattern: coved ST - segment elevation in V1-V2 leads 5 (A) and 10 (B) minutes after ajmaline infusion. Electrocardiogram speed - 100 mm/sec
Discussion
In the bibliography consulted, we did not find a description of the unmasking association of the electrocardiographic pattern of BrS related to afebrile anti-COVID vaccination in people WITHOUT previous diagnosis or suspicion of Brugada syndrome.
A comparative study between the different vaccines and their potential relationship with severe adverse effects, using the Eudra Vigilance database, showed that the BNT162b2 COVID-19 (BNT) (Pfizer/BioNTech) is the one with the fewest events (5).
The most similar reported case was published by Drs. Keisuke Okawa and Toshihiko Kan, (6). The coincidences with our patient were the detection time, and importantly the absence of fever in both cases. The most obvious differences unquestionably lie in the fact that here we refer to a female person, without suspicion or diagnosis of BrS despite her exhaustive medical evaluation in adolescence. Here it is worth asking about the retrospective significance to be given to the induction of monomorphic ventricular tachycardia originating from RVOT in her first EPS.
Although the prevalence of BrS is estimated at around 5/10,000, this number most likely underestimates the real prevalence due to asymptomatic patients, mainly in women, (7), which may lead us to speculate about whether the feared (although clearly very rare) potential association between anti-COVID 19 vaccination and sudden death could not be due to the unmasking and appearance of fatal events in people with undiagnosed BrS. Although we agree on the theoretical recommendation to perform an electrocardiogram prior to administration of the vaccine and three days after, we also know that in many countries the access to such screening may be unlikely or impossible and the need for vaccination is a public health priority and should not be discouraged by it. We strongly recommend it to those who have relatives diagnosed with BrS.
Conclusions
The vaccination used for the prevention of COVID-19 could unmask patients with hidden Brugada syndrome even without febrile episodes. A possible relationship with sudden death events requires further study. In people with known Brugada syndrome or in their relatives, we recommend serial electrocardiographic monitoring after the administration of the vaccination dose.
Ethics: Written patients consent form was obtained from patient before all procedures
Peer-review: Internal and external
Conflict of interest: None to declare
Authorship: L.A.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||


Perito Moreno glacier in Santa Cruz, Argentina. By Luis Arabia, Cordoba, Argentina
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

