Surgical treatment of the ascending aorta giant aneurysm
CASE REPORT
Surgical treatment of the ascending aorta giant aneurysm
Article Summary
- DOI: 10.24969/hvt.2022.342
- Page(s): 203-208
- Cardiac Surgery
- Published: 21/09/2022
- Received: 01/07/2022
- Revised: 18/07/2022
- Accepted: 07/09/2022
- Views: 5781
- Downloads: 4448
- Keywords: ascending aorta aneurysm, aortic valve regurgitation, surgical procedures, computed tomography angiography
Address for Correspondence: Khamidulla A. Abdumajidov, Republican specialized scientific-practical medical center of surgery named after acad.V.Vakhidov, Tashkent , Uzbekistan Email: hamidulla06@mail.ru
Saidorifhon Murtazaev, Abrol Mansurov, Khamidulla Abdumajidov, Sherzod Aliev, Khondamir Mirzaev
Republican specialized scientific-practical medical center of surgery named after acad.V.Vakhidov, Tashkent , Uzbekistan
Abstract
We shared our experience of surgical treatment of a giant aneurysm of the ascending aorta (11 cm) in a female patient with bicuspid valve, arterial hypertension and severe obesity. We performed aortic valve replacement and supracoronary prosthetic replacement of ascending aorta. She showed improvement in clinical status, echocardiography, and was discharged and followed up for 5 months after operation. Control computed tomography angiography demonstrated functioning aortic prosthetic graft.
Key words: ascending aorta aneurysm, aortic valve regurgitation, surgical procedures, computed tomography angiography
Introduction
Ascending aortic aneurysm (AAA) is a life-threatening disease that can lead to dangerous complications such as aortic wall rupture, acute aortic dissection, and aortic valve (AV) regurgitation. Surgical treatment of patients with ascending aortic aneurysm with concomitant AV regurgitation is still an urgent and unresolved problem (1).
According to several authors, the incidence of thoracic aortic aneurysms in the population averages 0.16–1.15% (1-4). Ascending aortic aneurysms are responsible for 15 000 deaths in the USA (4, 5). Etiological factors include atherosclerosis, Marfan's syndrome, giant cell arteritis, tuberculosis, syphilis, HIV-associated vasculitis, hereditary hemorrhagic telangiectasia, and medial agenesis (6).
On the one hand, as reported by the Mayo Clinic (USA), the main predictor for an unfavorable outcome is the size of the aneurysm. The risk of rupture, dissection, and death is in the range of 5–6.5% for aneurysm size of below 6 cm and more than 14% - above 6 cm (5). On the other hand, according to IRAD (International Registry of Acute Aortic Dissection), the diameter of the aorta itself is not determining factor, and there are other factors that can cause complications (3).
The first radical treatment of an ascending aorta was performed for acute dissection. The operations proposed at the dawn of the development of aortic surgery consisted in the resection and replacement of the site of dissection with synthetic or biological materials, in combination with the restoration of AV, by fixing its dissected commissures (6).
However, due to the lack of differentiated approach at that time, the results of the operation were unsatisfactory. According to the recommendations for the diagnosis and management of patients with aortic disease, nowadays, if aortic root dissection is present, the most perspective choice is preservation of the native aortic valve. In this case, either supracoronary ascending aortic replacement with concomitant root reconstruction, or valve sparing selective sinus of Valsalva replacement should be performed (2, 4).
In the absence of aneurysm and an intimal defect in the aortic root with the presence of pathology of the cusps of AV and aneurysm of ascending aorta, separate replacement of ascending aorta and AV is recommended (4, 7, 8).
The giant aneurysm of ascending aorta are rare disorder (6, 8, 9).
We aimed to report a severe case of giant ascending aortic aneurysm, results of its surgical treatment and short-time follow-up after operation.
Case report
A A female patient, born in 1988, was admitted to the department of ischemic heart disease with a diagnosis of ascending aortic aneurysm; severe aortic valve regurgitation, concomitant arterial hypertension grade 3; and class III obesity (body mass index of 41 kg /m2). She complained on sharp stabbing chest pain, palpitations, headache, dizziness, nausea, dyspnea and general weakness.
Her medical history is notable by the diagnosis of ascending aortic aneurysm established in 2013. Over the past 6 years, she have received medical treatment and was regularly observed by a cardiologist. Over the past two weeks, she has noted a sudden worsening in general condition with above-mentioned symptoms. She denied any hereditary disease, traumas and abuses.
Her clinical examination and laboratory and biochemical analyzes were within normal limits. Electrocardiogram: sinus rhythm, heart rate of 100 beats/min and signs of left ventricular hypertrophy. Transthoracic echocardiography: left ventricular end-diastolic volume (LVEDV) - 262.0 ml., left ventricular end-systolic volume (LVESV) - 120.0 ml., stroke volume (SV) - 142.0 ml, ejection fraction (EF) - 54%. AV: bicuspid and 3rd grade of regurgitation. The diameter of aorta at the level of AV is 2.4 cm, at the level of sinus of the Valsalva is 3.48 cm, at the level of sinotubular junction is up to 10 cm, and at the level of aortic arch 5.4 cm. Conclusion: aneurysm of the ascending aorta extending into the arch.
Computed tomography angiography of the heart: aorta dimensions: at the level of AV - 26mm, starting from the level of the aortic bulb to the level of the arch, there is an aneurysmal expansion up to 10.0cm, at the level of BCT (brachiocephalic trunk) - 43mm, aortic arch - 28mm, at the isthmus - 20mm, at the level of thoracic diaphragm - 21mm (Fig. 1).
Surgery: a median sternotomy was performed, with exposure of pericardium and visualization of aneurysm of the ascending aorta with a diameter of up to 11 cm, which compressed the adjacent organs (Fig. 2). Cannulation of the femoral artery and right atrium were performed (Fig. 3).
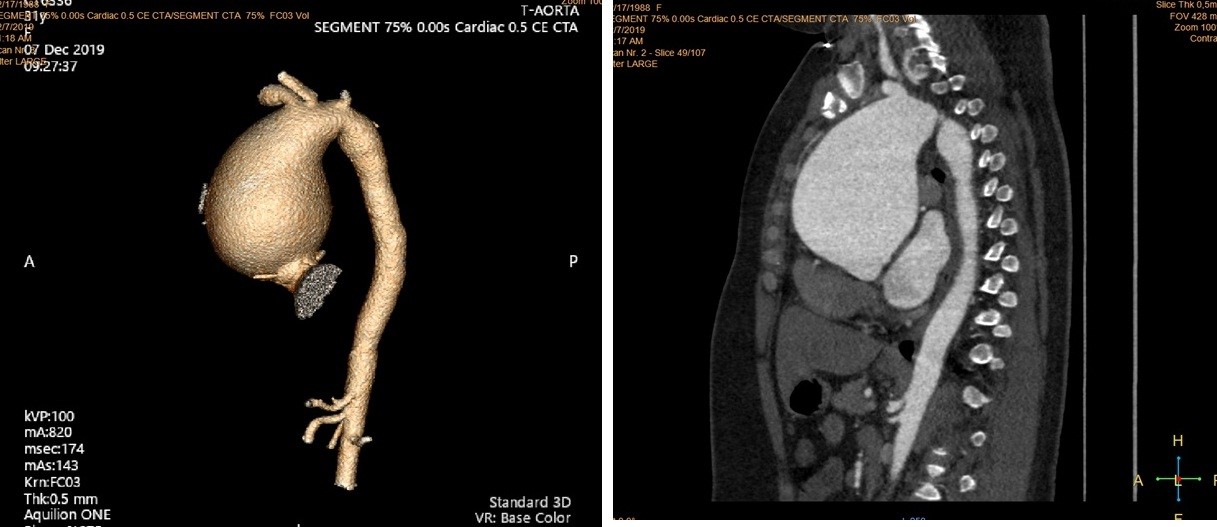
Figure 1. Computed tomography angiography of the thoracic aorta demonstrating giant ascending aorta aneurysm
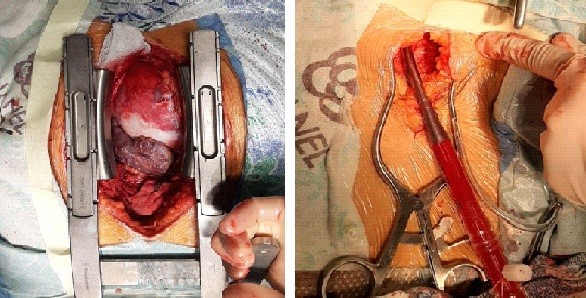
Figure 2. Ascending aortic aneurysm (intraoperative view).
Figure 3. Cannulation of the femoral artery
The aneurysm zone was covered by an adhesion process. With technical difficulties, the ascending part and the aortic arches were mobilized. Сardiolysis. Aortal clamping 1 cm below the BCT. The ascending aorta was exposed, selective antegrade cardioplegia into ostium of the coronary arteries (ostium of the right and left coronary arteries are not involved in aneurysmatic process). Asystole. Revision. The aortic root is not dilated. Transesophageal echocardiography demonstrated severe aortic valve regurgitation. Resection of aorta 1 cm below the clamp. The proximal end was resected above the ostium of the coronary arteries. Further, the cusps of the AV were resected, 12 “П” shaped Etibond 2/0 with TFE pledgets were sutured supraannularly and the St.Jude No. 25 mechanical aortic valve was implanted into the aortic position (Fig. 4).
The next step, proximal and distal anastomosis were formed with the Vascutek vascular prosthesis ( size 30 mm) which was fixed with continuous “Prolene 4/0” suture (Fig. 5). Figure 6 demonstrates postoperative appearance of formed prosthetic ascending aorta.

Figure 4. Aortic valve replacement
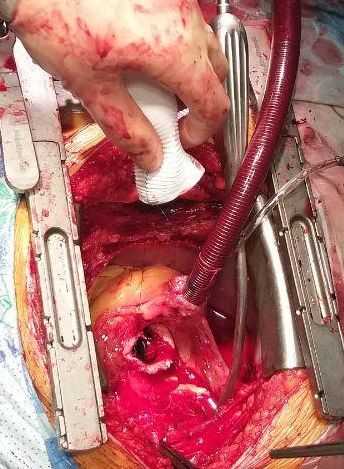
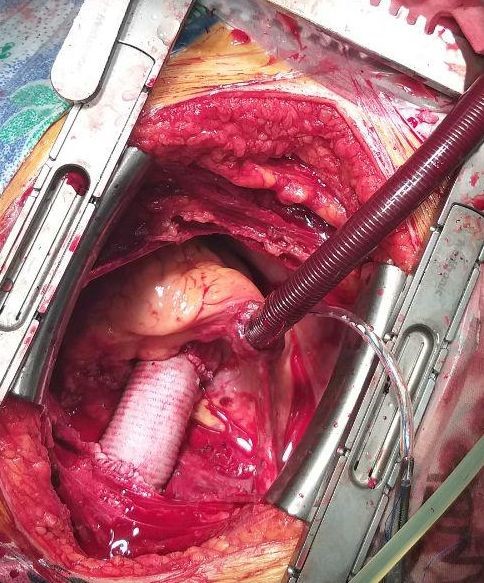
Figure 5. Implantation of vascular prosthesis Figure 6. Prosthetic aorta intraoperative view
After the prevention of air embolism, the clamp was removed from the aorta. Disconnection of cardiopulmonary bypass. Protamine sulfate injection. Hemodynamics was stable. Blood pressure - 100/70mm Hg, heart rate - 80 beats/min. Step by step closure of wound. The patient in a stable condition was transferred into the intensive care unit.
On the second day after the operation, she transferred to department ward. On the control echocardiography there was a reduction of left ventricular volumes: LVEDV was 192.0ml, LVESV- 100.0ml, SV - 92.0ml and EF- 48%. The AV pressure gradient was 10 mm Hg. The patient was discharged on the 6th day after the operation.
On 5-th month of follow-up after the operation, control computed tomography angiography of thoracic aorta was performed showing functioning prosthetic graft (Fig. 7).
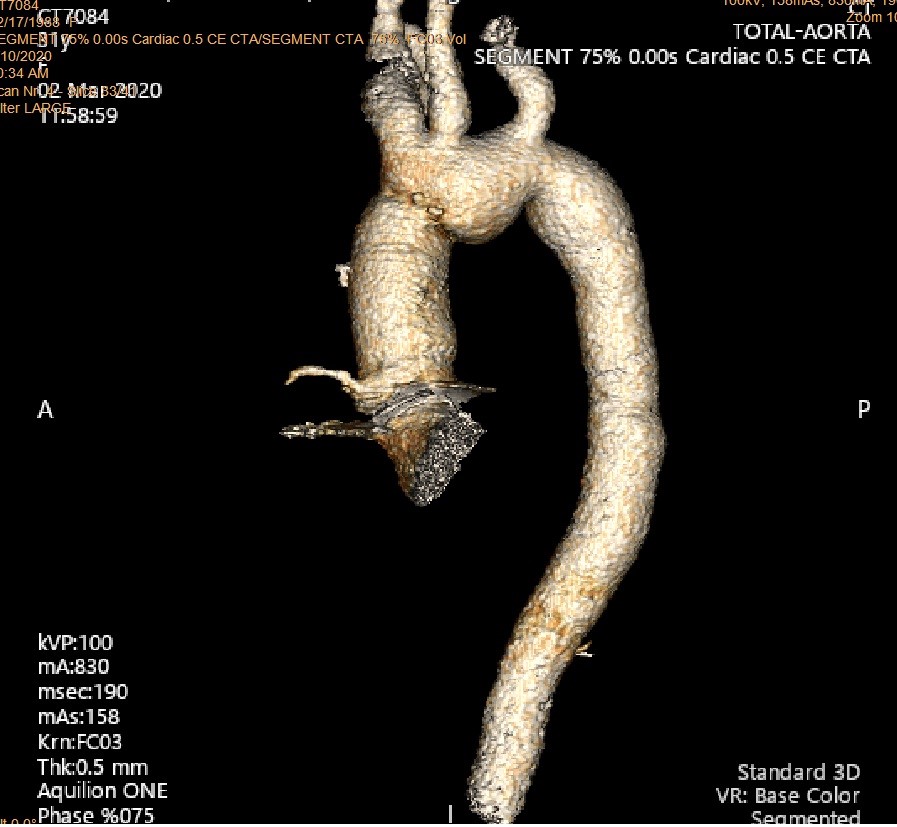
Figure 7. Computed tomography angiography view of prosthetic ascending aorta 5 months after implantation
Discussion
Surgical management of a giant AAA is still challenging, as it poses some complication risks such as bleeding, end- organ ischemia, burden of underlying disease and staged repairs. During the operation, performing median sternotomy may lead to aortic injury since the aneurysmal wall is very close to sternum. Therefore, the exploration and cannulation of femoral vessels for the establishment of cardiopulmonary bypass before the median sternotomy are recommended (8).
In this case, we successfully performed a prompt open surgical repair of a giant AAA and AV (aortic valve replacement + suprocoronary replacement of ascending aorta), and obtained a satisfactory result without any morbidity and mortality during postoperative period. To the best of our own experience, our case is one of the largest AAA reported to date in the existing literature (6, 8, 9). The difference of our case from another cases, we mostly made an accent to the surgical treatment of this pathology and described step by step stages of the whole operation. Similar case was reported by Shah et al (6) on surgical treatment of giant aortic aneurysm, authors performed aortic valve replacement and placed Vascutek graft as in our case, however aneurysm size was larger in our case. Another case of giant aortic aneurysm was reported by Shah P et al. (9), their case was distinguished by asymptomatic large proximal aneurysm of 13 cm and they performed Bentall procedure with aortic valve replacement, reconstruction of aorta and re-implantation of coronary arteries.
Conclusion
Our patient had congenital heart disease -bicuspid aortic valve and giant ascending aortic aneurysm. Our experience showed that open heart surgical correction of giant aneurysms of the ascending aorta with placement of prosthetic graft and aortic valve replacement demonstrates good results in the short and long-term follow up periods, thereby reducing risk of sudden death.
Ethics: Informed consent was obtained from patient before all procedures.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: S.S.M, A.A.M, Kh.A.A., Sh.M.A., Kh.A.M. equally contributed to the management of patient and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

Floralis Generica by Argentinian architect - Eduardo Catalano. Photography by Pablo Roura, Buenos Aires, Argentina
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

