What is new with 2022 European Society of Cardiology guidelines for prevention of sudden cardiac death?
EDITORIALS
What is new with 2022 European Society of Cardiology guidelines for prevention of sudden cardiac death?
Article Summary
- DOI: 10.24969/hvt.2022.344
- Page(s): 159-161
- CARDIOVASCULAR DISEASES
- Published: 28/09/2022
- Received: 24/09/2022
- Accepted: 26/09/2022
- Views: 9181
- Downloads: 4572
- Keywords: editorial
Address for Correspondence: Sok-Sithikun Bun, Pasteur University Hospital, Nice, France,
Phone: +33492037733 Fax: +37797989732 Email: sithi.bun@gmail.com
Sok-Sithikun Bun, Emile Ferrari
Cardiology Department, Pasteur University Hospital, Nice, France
Abbreviations
ARVC : Arrhythmogenic right ventricular cardiomyopathy
BrS : Brugada syndrome
CAD : coronary artery disease
CMR : cardiac magnetic resonance
CPVT : catecholaminergic polymorphic ventricular tachycardia
DCM : dilated cardiomyopathy
ERS : early repolarization syndrome
HCM : hypertrophic cardiomyopathy
ICD : implantable cardioverter defibrillator
LGE : late gadolinium-enhancement
LQTS : long QT syndrome
LVEF : left ventricular ejection fraction
NSVT : non-sustained ventricular tachycardia
OHCA : out-of-hospital cardiac arrest
PES : programmed electrical stimulation
PVCs : premature ventricular contractions
RVOT : right ventricular outflow tract
SCD : sudden cardiac death
SHD : structural heart disease
VA : ventricular arrhythmias
VF : ventricular fibrillation
VT : ventricular tachycardia
During the last European Society of Cardiology Congress in 2022, the new guidelines document for the management of patients with ventricular arrhythmias (VA) and the prevention of sudden cardiac death (SCD) was released (1). We summarize here the key points from this international guidelines document.
New sections have appeared in these recent guidelines, such as the presence of a dedicated paragraph concerning provocative diagnostic tests in the context of Brugada syndrome (BrS) using ajmaline or catecholaminergic polymorphic ventricular tachycardia (CPVT) using epinephrine challenge; a large room is now left for genetic testing in probands for primary electrical diseases: class I indication in long QT syndrome (LQTS), BrS and CPVT. A new specific section has been added concerning the diagnostic evaluation at first presentation with ventricular arrhythmias (VA) in patients without known cardiac disease. A cardiac magnetic resonance (CMR) should be considered (class IIa indication) for instance in patients with newly documented VA [(frequent premature ventricular contractions (PVCs), non-sustained ventricular tachycardia (NSVT)] or sustained monomorphic ventricular tachycardia) and suspicion of structural heart disease (SHD) other than coronary artery disease (CAD). Very didactic algorithm is provided for the management of patients with electrical storm.
Public basic life support
New class I recommendations have appeared insisting on public-access defibrillation available at sites where cardiac arrest is likely to occur such as shopping malls, stadiums, public transport stations or casinos. The importance of prompt cardio-pulmonary resuscitation by bystanders in case of out-of-hospital cardiac arrest (OHCA) is reminded (class I). Mobile-phone-based applications, should be encouraged to assist OHCA victims (class IIa).
More indications for programmed electrical stimulation (PES)
A larger place for PES can be notified in these new recommendations:
1/ CAD with left ventricular ejection fraction (LVEF) between 36 and 40% despite ≥3 months of optimal medical therapy and NSVT or unexplained syncope (class IIa);
2/ Dilated cardiomyopathy (DCM) with LVEF between 35 and 50 % (class IIa);
3/ Cardiac sarcoidosis with LVEF between 35 and 50 % (class IIa as well);
4/ Myotonic dystrophy patients complaining on palpitations highly suspicious for VA if induction of a non-bundle-branch-reentry VT (class IIa);
5/ In patients with arrhythmogenic right ventricular cardiomyopathy (ARVC) and symptoms highly suspicious for VA (class IIb);
6/ PES may be discussed in asymptomatic patients with a spontaneous type I BrS electrocardiogram (class IIb).
Drug therapy
Noticeable points are reported as following:
-The full therapeutic arsenal must be administered in all heart failure patients with reduced LVEF including beta-blockers, angiotensin receptor neprilysin inhibitor/angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, mineralocorticoid receptor antagonist and sodium-glucose co-transporter 2 inhibitors (class I).
-At first intention, intravenous procainamide should be considered in case of hemodynamically tolerated sustained monomorphic VT and known or suspected SHD (class IIa).
-Mexiletine is a class I indication in case of LQT3 syndrome. Beta-blockers and/or flecainide with or without acetazolamide should be considered in patients with Andersen-Tawil syndrome to treat VA (class IIa).
-It is finally interesting to notice also that quinidine is a class IIa indication for electrical storm in BrS, early repolarization syndrome (ERS) and idiopathic ventricular fibrillation (VF); class IIb indication for polymorphic VA triggered by unifocal PVC.
Catheter ablation
New specific indications for catheter ablation in different situations should be emphasized. Catheter ablation may now be proposed as a first-line therapy (class I) for symptomatic idiopathic VT/PVCs from the right ventricular outflow tract (RVOT) or the left fascicles (Fig. 1). This strategy may be an alternative to implantable cardioverter defibrillator (ICD) therapy in patients with CAD and hemodynamically well-tolerated sustained monomorphic VT with LVEF ≥ 40 %, if only successful endpoints are achieved (VT non-inducibility and elimination of electrograms consistent with conduction delay). In patients with repaired Tetralogy of Fallot undergoing surgical or transcutaneous pulmonary valve replacement, pre-operative transection of VT-related anatomical isthmuses before the intervention may be considered (class IIb).
Dilated cardiomyopathies
Genetic testing (class I) is now recommended if atrioventricular conduction delay before the age of 50, or in case of family history of DCM or SCD in a first-degree relative (at age < 50 years). It is very interesting to notice that the experts have provided a new recommendation for ICD implantation in patients with LVEF between 35 and 50% and ≥ 2 risk factors: syncope, late gadolinium enhancement on CMR, inducible sustained monomorphic VT during PES, and pathogenic mutations in LMNA, PLN, FLNC, and RBM20 genes (class IIa).
Hypertrophic cardiomyopathy (HCM)
Beyond the well-known HCM SCD score, significant LGE at CMR above 15% of left ventricular mass, and finally the presence of sarcomeric pathogenic mutations should now be taken into account for considering ICD implantation in patients aged 16 years or more (class IIa). A specific HCM Risk-Kids score may now be proposed for children < 16 years for considering prophylactic ICD implantation (class IIa).
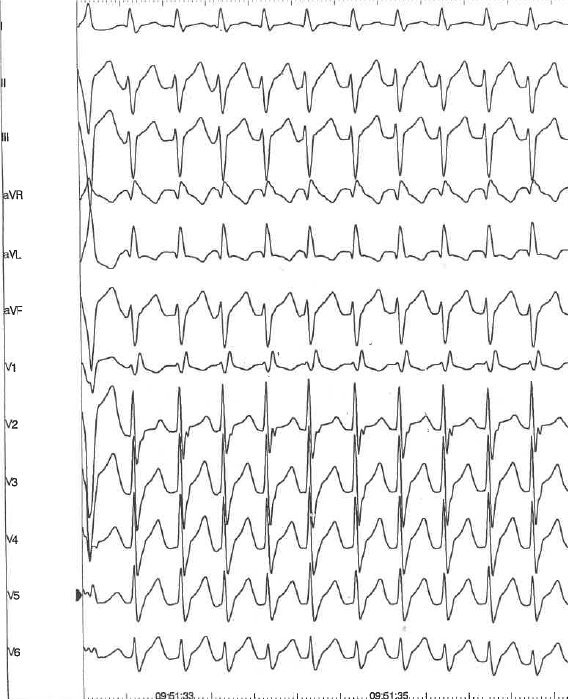
Figure 1. Fascicular ventricular tachycardia (S.S.B. own collection)
Finally, these new guidelines provide several comprehensive flowcharts in different clinical scenarios, with an important place for management strategies facilitating everyday clinical decision-making. Genetic testing and counselling should now be largely integrated in the global management of patients with DCM, ARVC, HCM, neuromuscular diseases, primary electrical diseases, or after sudden cardiac arrest.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: S.S.B and E.F. equally contributed to the preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||

More and more like heaven in the water of Veerse lake. Zeeland, Netherlands. By Christiaan Vrints, Antwerp, Belgium
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

