What is new in the updated 2022 Coronary Artery Disease-Reporting and Data System (CAD-RADS™ 2.0) consensus document?
EDITORIALS
What is new in the updated 2022 Coronary Artery Disease-Reporting and Data System (CAD-RADS™ 2.0) consensus document?
Article Summary
- DOI: 10.24969/hvt.2022.351
- Page(s): 168-171
- CARDIOVASCULAR DISEASES
- Published: 19/11/2022
- Received: 18/11/2022
- Accepted: 19/11/2022
- Views: 8537
- Downloads: 4852
- Keywords: editorial
Address for Correspondence: Kairgeldy Aikimbaev, Radiology Department, Medical Faculty, Cukurova University, Adana, Turkey E-mail: aikimbaev@gmail.com Phone: +90 542 695 82 32
Kairgeldy Aikimbaev, Ferhat Can Piskin
Cukurova University Medical Faculty, Radiology Department, Adana, Turkey
In recent years, coronary computed tomography angiography (CCTA) has made significant advances in both imaging technology and clinical validation of CCTA-derived interpretations. During this period, imaging protocols were optimized according to image quality, diagnostic accuracy and radiation dose. Indeed, interpretation standards are as important as image quality. In general, standardized reporting helps reduce variability among image interpreters. Because of standardized reporting, it is always expected to be beneficial to link the final opinion in the CCTA report with recommendations for subsequent patient management. The first Coronary Artery Disease Reporting and Data System (CAD-RADS) was launched in 2016 to standardize the reporting system for patients with suspected or known coronary artery disease undergoing CCTA in an outpatient, inpatient, or emergency setting, and was created for the purpose to guide the next possible pathways in patient management (1). The main goal of CAD-RADS was to create standardization of report terminology for CCTA results in order to improve communication between image interpreter and referring physicians in a clear and consistent fashion and to better guide clinical decision-making. The proposed CAD-RADS classification was applied on a per-patient basis and represents the highest-grade coronary artery lesion documented by CCTA. The implementation of the first CAD-RADS system included application in two different clinical settings (patients presenting with stable chest pain and patients presenting with acute chest pain), description of the most severe coronary artery luminal stenosis (for vessels ≥1.5 mm in diameter), and three modifiers (stent, graft, and vulnerability).
In July 2022, a new expert consensus document on Coronary Artery Disease-Reporting and Data System (CAD-RADS 2.0-2022) was published by the Society of Cardiovascular Computed Tomography in collaboration with the American College of Cardiology, the American College of Radiology and the North America Society of Cardiovascular Imaging (2). New additions for the updated expert consensus recommendations include an emphasis on the reporting of ischemia findings and coronary plaque burden on CCTA. Below are key updates from the consensus recommendations.
The emphasis on myocardial ischemia
The consensus panel recommended an ischemia “I” modifier to indicate testing for ischemia via computed tomography fractional flow reserve (CT-FFR) or stress myocardial computed tomography perfusion (SCTP). The consensus panel noted multiple benefits of utilizing SCTP. In addition to enabling radiologists to discern fixed perfusion defects due to prior myocardial infarction, SCTP could prevent unnecessary testing by allowing radiologists to exclude myocardial ischemia in cases of moderate coronary stenosis or severe coronary stenosis in the presence of mixed or densely calcified plaque.
Modifier “I” indicates that computed tomography-based ischemia test was performed with CT-FFR or SCTP. Concerning SCTP interpretation, the consensus experts recommended a positive “I+” modifier to denote myocardial ischemia or peri-infarction ischemia. A negative “I-” modifier could be employed when there is no detected ischemia, a previously detected myocardial infarct or an ischemic segment that does not have a concordant anatomic lesion. Patients with prior myocardial infarction and fixed perfusion defects without evidence of myocardial ischemia by SCTP would be classified as” I-“. The presence of myocardial infarction should be documented in the findings of the report.
When there are indeterminate or questionable findings, or a high likelihood of false-positive results with stress myocardial computed tomography perfusion, the consensus authors recommended an “I±” modifier.
Briefly,
1) A positive “I+” modifier indicates that CT-FFR or CTP demonstrated lesion-specific ischemia or reversible perfusion defect,
2) A negative “I-“ modifier indicates that CT-FFR or CTP is negative for lesion specific ischemia or reversible ischemia,
3) “I±” modifier indicates that CT-FFR or CTP was borderline.
The emphasis on high-risk plaque
Noting a link between characteristics of high-risk plaque (previously referred to as vulnerable plaque) viewed on CCTA and acute coronary syndrome, the consensus experts expressed a need for a “HRP” modifier to denote high-risk plaque. High-risk plaque features include low attenuation plaque (less than 30 Hounsfield units) (Fig. 1), positive remodeling, spotty calcifications (Fig. 2), and the “napkin ring sign” (Fig. 3). On CCTA, a lipid rich necrotic core can be detected as low-attenuation non-calcified plaque (3). Positive remodeling is defined as at least 10% increase in vessel diameter at the site of the plaque compared to a reference segment set proximal to the lesion in a normal-appearing vessel segment. (4). The “napkin-ring sign” is defined according to the presence of a ring of high attenuation around certain coronary artery plaques, and attenuation of the ring presenting higher than those of the adjacent plaque and no more than 130 Hounsfield units (5). Spotty calcification is defined as punctate calcium <4 mm in length within a plaque (6). If CCTA reveals two or more HRP, the consensus panel suggested using the “HRP” modifier in these cases.
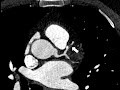
Figure 1. Example of focal non-calcified plaque (arrow) at the orifice of D1 of the LAD detected on CCTA. The plaque displays a high-risk feature, low attenuation (<30 HU).
CCTA - coronary computed tomography angiography, D1- first diagonal branch, HU - Hounsfield unites, LAD - left anterior descending coronary artery

Figure 2. Spotty calcifications (arrow) within low attenuated plaques in proximal LAD detected on CCTA.
CCTA - coronary computed tomography angiography, LAD - left anterior descending coronary artery

Figure 3. Example of “napkin ring sign” (arrow) in the LAD detected on CCTA.
CCTA - coronary computed tomography angiography, LAD - left anterior descending coronary artery
The emphasis on coronary plaque amount
Another key update provided in the CAD-RADS 2.0 statement is that plaque burden should be estimated whenever present. Due to a robust association between the coronary plaque amount found on CCTA and incident coronary heart disease, the consensus authors added the modifiers P1 to P4 to designate mild, moderate, severe and extensive coronary plaque. In general, reporting methods for coronary plaque burden assessment include qualitative visual estimates of plaque in coronary vessels, quantitative assessment of total coronary plaque, a segment involvement score and coronary artery calcium testing. The consensus authors maintained that segment involvement score and coronary artery calcium might provide more reproducible approaches for categorizing the amount of coronary plaque. Based on these methods, the overall amount of plaque (P) descriptor ranges from P1 to P4 (mild, moderate, severe, extensive) to denote increasing categories of plaque burden. The classification P is not required for CAD-RADS 0 (zero). As there is currently no a single method that should be used to identify the overall amount of plaque, CAD-RADS experts recommend the technique most appropriate at a given clinic.
The emphasis of non-atherosclerotic etiologies of coronary abnormalities
While non-atherosclerotic etiologies of coronary abnormalities may be key considerations in the differential diagnosis, the consensus authors recommend using an "E" (exceptions) modifier to document exceptions to CAD-RADS reporting and non-atherosclerotic causes of coronary obstruction. The “E” modifier both helps to monitor these etiologies and may indicate to clinicians that the case in question contains a coronary abnormality that may fall outside the traditional CAD-RADS classification due to non- atherosclerotic coronary artery disease. Examples of non-atherosclerotic causes of coronary abnormalities may include anomalous origin of the coronary arteries, arterio-venous malformation, coronary artery dissection, coronary artery aneurysm or pseudoaneurysm, coronary artery fistula, extrinsic coronary artery compression, vasculitis etc.
Conclusion
In the expert group's opinion, the updated CAD-RADS™ 2.0 classification now follows a framework of stenosis grade, plaque burden, and modifiers, which include assessment of myocardial ischemia with computed tomography fractional flow reserve or stress computed tomography perfusion, where appropriate. With these new updates, CAD-RADS ™ 2.0 will continue to provide an important standardization framework that will benefit education, research and quality assurance whose primary goal is to improve individual patient care.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: K.A. and F.C.P equally contributed to the preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

