Predictive significance and diagnostic accuracy of plasma fibrinogen levels for coronary stenting outcomes
ORIGINAL RESEARCH ARTICLE
Predictive significance and diagnostic accuracy of plasma fibrinogen levels for coronary stenting outcomes
Article Summary
- DOI: 10.24969/hvt.2022.365
- Page(s): 34-42
- CARDIOVASCULAR DISEASES
- Published: 20/12/2022
- Received: 04/10/2022
- Revised: 26/11/2022
- Accepted: 28/11/2022
- Views: 5232
- Downloads: 4509
- Keywords: Coronary stent outcomes, major adverse cardiac and cerebrovascular events, plasma fibrinogen, stent diameter
Address for Correspondence: Gaurav Singh, Department of Cardiology, UNMICRC, Civil Hospital Campus, Asarwa, Ahmedabad-380016, Gujarat, India M: +91 757 395 25 10, Fax: +91 792 268 20 92
Email: mdmedgaurav@gmail.com
Tarun Bansal1, Anand Shukla2, Rujuta Parikh2, Gaurav Singh2*, Ashish Mishra4, Lalan Singh3, Krutika Patel4, Iva Patel4, Utsav Patel2
1Apollo Hospital, Lucknow , Gujarat India
2Department of cardiology, U. N. Mehta Institute of Cardiology and Research Centre (UNMICRC), Asarwa, Ahmedabad-380016, Gujarat, India
3Department of cardiology, Shyam Shah Medical College, Rewa-486001, Rewa, India
4Department of cardiology, U. N. Mehta Institute of Cardiology and Research Centre (UNMICRC), Civil Hospital Campus, Asarwa, Ahmedabad-380016, Gujarat, India
Abstract
Objective: The advancement in percutaneous transluminal coronary angioplasty (PTCA) has led to it becoming the predominant mode of revascularization. Post PTCA adverse events in the form of stent thrombosis, recurrent ischemia, unplanned revascularization, recurrent hospitalization etc. result in morbidity as well as mortality. Biomarkers predicting such outcomes can be useful in initiating more aggressive medical therapy and greater modification of risk factors. This study was undertaken to study the predictive significance of periprocedural plasma fibrinogen levels for coronary stenting outcomes.
Methods: 80 patients diagnosed as either chronic stable angina (CSA), unstable angina (UA), Non ST Elevation Myocardial Infarction (NSTEMI) or late presentation ST Elevation Myocardial Infarction (STEMI) undergoing planned PTCA were included in study. Patients were evaluated for clinical history, electrocardiogram (ECG), two dimensional echocardiography (2D-echo) and cardiac biomarkers (Creatinine Phosphokinase-MB isomer (CK-MB) and Troponin I). Serum fibrinogen level was measured 24 hours prior to PTCA along with routine pre-operative investigations; and also 24 hours after coronary stenting. Patients were followed for six months. Outcome measure was taken to be freedom from cardiac related adverse events, including rehospitalization, unplanned repeat revascularization, definite stent thrombosis, transient ischemic attack, stroke and all-cause mortality.
Results: Fibrinogen level ≥393 mg/dL, 24 hours prior to percutaneous transluminal coronary angioplasty, was associated with higher major adverse cardiac and cerebrovascular events (MACCE) rates (60%) as compared to those with fibrinogen level <393 mg/dL (3.6%). Fibrinogen level ≥427 mg/dL 24 hours after percutaneous transluminal coronary angioplasty, was associated with higher major adverse cardiac and cerebrovascular events rates (65%) as compared to those with fibrinogen level <427 mg/dL (6.7%).
Conclusion: The current study demonstrates that higher baseline and post procedural fibrinogen, is an independent predictor of 6 months major adverse cardiac and cerebrovascular events after elective percutaneous coronary intervention.
Key words: Coronary stent outcomes, major adverse cardiac and cerebrovascular events, plasma fibrinogen, stent diameter
Abbreviations:
2D-echo Two-Dimensional Echocardiography
CAD Coronary Artery Disease
CPKMB Creatinine Phosphokinase-MB isomer CRP C-reactive protein
CSA Chronic Stable Angina
FDP Fibrinogen degradation products
Gp IIb/IIIa Glycoprotein IIb/IIIa receptor
ICAM-1 Interaction with Intracellular Adhesion Molecule-1
ISR In-Stent Restenosis
LVEF Left Ventricular Ejection Fraction
MACCE Major Adverse Cardiac and Cerebrovascular Events
NSTEMI Non-ST-Elevation Myocardial Infarction
PCI Percutaneous coronary intervention
PTCA Percutaneous Transluminal Coronary Angioplasty
ROC Receiver operating characteristic curve
STEMI ST - Elevation Myocardial Infarction
Trop-I Troponin I
Introduction
Traditionally, percutaneous coronary intervention (PCI) has become a common treatment of coronary artery disease (CAD). Early recoil, alteration in blood vessels, release of vasoactive and thrombogenic factors and neo-intimal proliferation have been suggested as significant contributors to the restenosis after coronary angioplasty (1, 2).
Plasma fibrinogen is an acute phase reactant with known inflammatory mechanism, but it also affects platelet aggregation and blood viscosity (3, 4). Inflammation leads to development of neo-intimal hyperplasia which results in restenosis of the stented vessels. Many inflammatory molecules have been studied as potential indicators of CAD risk.
These include the cytokines (tumor necrosis factor –alpha (TNF-alpha), interleukin (IL)-1-beta, IL-10 and IL-6), endothelial activation markers (E-selectin and vascular cell adhesion molecule (VCAM)-1), circulating adhesion proteins etc. These are produced in liver and increase or decrease in response to inflammatory stimuli (5). Serum fibrinogen, serum amyloid A, and high sensitivity C-reactive protein (hs-CRP) are among the acute-phase proteins that increase during inflammation and have been studied as predictors of CAD. Certain markers like adiponectin and IL-10 are downregulated in inflammation (6).
Fibrinogen levels have correlated positively with number of diseased vessels as well as the severity of CAD. In addition, in patients with chronic stable angina (CSA) without any known coronary risk factors, fibrinogen was the strongest predictor of global coronary score, number and severity of coronary artery stenosis (7).
Although epidemiological studies have evaluated role of fibrinogen in CAD, there are still aspects that need further investigation.
Hence, this study was undertaken to evaluate predictive significance and diagnostic accuracy of fibrinogen in stent outcomes in patients who underwent elective PTCA for acute coronary syndrome (ACS) or CSA.
Methods
Study design:
This is a prospective observational study of 80 consecutive patients fulfilling the inclusion and exclusion criteria. It was conducted between November 2016 and January 2019 at a tertiary cardiac care hospital in Ahmedabad, Gujarat, India.
Participants:
Inclusion criteria:
-All patients with CSA who underwent elective PCI.
-All patients with ACS including UA and NSTEMI who underwent elective PCI.
-All patients with hemodynamically stable ST elevation myocardial infarction (STEMI) who were late presenters (out of window period) and underwent PCI minimum 72 hours after presentation.
-All patients who gave written informed consent.
CSA was defined as episodes of typical anginal pain of more than 2 months duration (8). ACS refers to spectrum of clinical syndrome compatible with acute myocardial ischemia and includes unstable angina, NSTEMI and STEMI. Unstable angina (UA) was defined as rest angina lasting more than 20 minutes or new onset angina in less than 2 months or crescendo angina increasing in frequency, duration or intensity of symptoms. NSTEMI was defined as evidence of myocardial ischemia and myocardial necrosis in the form of positive cardiac biomarkers (9).
Exclusion Criteria:
-Patients with STEMI of less than 72 hours on presentation
-Patients who were late presenters of STEMI but had any indication for rescue PTCA like arrhythmia or hemodynamic instability.
-Patients with NSTEMI needing urgent revascularization.
-Patients with any active infection.
-Patients with use of intravenous glycoprotein IIb/IIIa inhibitor prior to or during the PCI.
-Patients with extensive CAD requiring more than two stents deployment, chronic total occlusion (CTO) lesion; or use of special hardware like rotablation.
The history of relevant coronary risk factors including hypertension, diabetes mellitus, smoking and family history was recorded. Electrocardiogram (ECG), 2D echocardiography and cardiac biomarkers (CK-MB and Troponin I) were also recorded.
Fibrinogen measurement
Plasma fibrinogen levels were analyzed by automated hematology analyzer STA-compact MAX reagent kit. Normal plasma fibrinogen levels range from 150 to 450 mg/dl. Two ml of venous blood sample was collected in 3.2% sodium citrate added tubes from the patients 24 hours prior to and 24 hours after the coronary stenting for the analyses of plasma fibrinogen levels in mg/dl.
Percutaneous coronary intervention
Coronary stenting was done either using radial or femoral route under a local anesthetic agent. All patients underwent PTCA with the use of a second-generation drug eluting stent (DES). The stent size was assessed angiographically and depended on the discretion of the interventional cardiologist. Patency of the vessel was assessed by coronary angiography after the procedure was completed. Thrombolysis in myocardial infarction (TIMI) 3 flow was achieved in all.
All patients who underwent PTCA received loading dose of tablet clopidogrel 300 mg and tablet aspirin 300 mg prior to the procedure. Intravenous heparin was given during the procedure. Intravenous or intracoronary glycoprotein IIb/IIIa inhibitor was not used. Post PTCA patient received tablet aspirin 150mg, second antiplatelet drug (either clopidogrel, prasugrel or ticagrelor at the discretion of treating cardiologist) and statin for minimum of six months.
Follow up and outcomes
Patients were followed up for six months with regular OPD visits. Outcome measure was taken to be freedom from cardiac related adverse events at six months. Cardiac related events included major adverse cardiac and cerebrovascular events (MACCE) –re-hospitalization for a suspected ACS, unplanned repeat revascularization, definite or probable stent thrombosis, transient ischemic attack, ischemic or hemorrhagic stroke, or any death. Occurrences of adverse events were collected from the admitted patient's case records and active surveillance by telephonic conversations.
Statistical analysis
All statistical analyses were performed using SPSS v 22.0 software (Chicago, IL, USA). Continuous variables were summarized as mean (standard deviation), whereas categorical variables were expressed as percentage of the sample. Continuous variables were compared using the unpaired student’s t-test and categorical using Chi-square test. Receiver operating characteristic curve (ROC) analysis was used to find the cut-off value of fibrinogen in our study population. Binary logistic regression analysis was used to find follow up outcome association with risk factors. Group differences associated with a p value ≤ 0.05 were considered statistically significant.
Results
Baseline demographic characteristics:
In the study population, mean age was 54.62 (10.94) years with 80% male patients and 20% female patients. Overall 33.8% of patients had diabetes mellitus, 65% had hypertension and 21.3% were smokers; 55% of the patients had CSA, 45% had ACS as mentioned in Table 1. The mean left ventricular ejection fraction (LVEF) of the study population was 48.04 (8.97)%. Maximum patients had NYHA class-II (50%) followed by NYHA Class-I, III and IV (33.75%, 13.75% and 2.5%) respectively. Mean baseline fibrinogen levels 24 hours prior to PCI was 358.33 (107.09) mg/dl and after stenting mean fibrinogen level was 381.55 (94.62) mg/dl. Other cardiac biomarkers like troponin I (6.95 (6.15) ng/L) and CK-MB (55.49 (91.25) U/L) was also measured. Of all cohort, 76.3% patients were treated with one stent and 23.8% were treated with two stents. The highest number of patients had occlusion of left anterior descending artery (LAD) (68.8%), followed by left circumflex artery (LCx) (33.8%) and right coronary artery (RCA) (28.7%).
Follow up characteristics
At six months follow up, 17 (21.2%) patients had MACCE out of which 15 were male and 2 were female patients. The presenting event was not found to be significantly associated with MACCE (p=0.54). Occurrence of MACCE events was not significantly associated with presence of risk factors, clinical parameters, biochemical parameters and procedural parameters as detailed in Table 2. Occurrence of MACCE event was associated with periprocedural fibrinogen level (p=<0.0001) and stent diameter (p=0.004).
![]()
|
Table 1. Baseline characteristics |
|
|
Variables |
N=80(%) |
|
Age, years |
54.63 (10.94) |
|
Male, n(%) |
64(80) |
|
Female, n(%) |
16(20) |
|
Diabetes mellitus type 2, n(%) |
27(33.8) |
|
Hypertension, n(%) |
52(65) |
|
Smoking, n(%) |
17(21.3) |
|
LAD stenosis, n(%) |
55(68.8) |
|
LCx stenosis, n(%) |
27(33.8) |
|
RCA stenosis, n(%) |
23(28.7) |
|
No. of patients with single- vessel disease, n(%) |
62 (77.5) |
|
No. of patients with double-vessel disease, n(%) |
11 (13.75) |
|
No. of patients with triple - vessel disease, n(%) |
7 (8.75) |
|
Electrocardiogram on presentation |
|
|
Sinus rhythm, n(%) |
80 (100) |
|
QRS duration (ms) , n(%) |
92.3 (6.5) |
|
ST elevation with Q waves, n(%) |
9 (11.3) |
|
ST depression, n(%) |
31 (38.75) |
|
T wave inversion, n(%) |
24 (30) |
|
Coronary artery disease types |
|
|
ACS-NSTEMI, n(%) |
8(10) |
|
ACS-UA, n(%) |
7(8.8) |
|
Stable angina, n(%) |
44(55) |
|
STEMI, n(%) |
21(26.2) |
|
Occurrence of MACCE , n(%) |
17(21.3) |
|
NYHA class, n(%) |
|
|
Class-I |
27(33.75) |
|
Class-II |
40(50) |
|
Class-III |
11(13.75) |
|
Class-IV |
2(2.5) |
|
Biochemical parameters |
|
|
Hemoglobin, gr/dl |
12.87 (1.5) |
|
Serum creatinine, mg/dl |
0.85 (0.17) |
|
Troponin I ng/L |
6.95 (16.15) |
|
CK-MB U/L |
55.49 (91.25) |
|
Serum fibrinogen (mg/dl) 24 hrs prior stenting |
358.33 (107.09) |
|
Serum fibrinogen (mg/dl) 24hrs after stenting |
381.55 (94.62) |
|
LVEF, % |
48.04 (8.97) |
|
Patients with one stent, n(%) |
61(76.3) |
|
Patients with two stents, n(%) |
19(23.8) |
|
Stent length, mm |
29.90 (7.2) |
|
Stent diameter, mm |
2.92 (0.36) |
|
ACS- Acute coronary syndrome, CK-MB- creatine kinase-myoglobin binding, LAD- left anterior descending artery, LCx- left circumflex artery, LVEF-left ventricular ejection fraction, NSTEMI- non ST-elevation myocardial infraction; MACCE- major adverse cardiac and cerebrovascular events, RCA- right coronary artery, STEMI- ST-elevation myocardial infraction; SVD, UA-unstable angina |
|

Predictors of MACCE
In patients who had MACCE, mean fibrinogen level 24 hours prior to PTCA was 485.52 (103.14) mg/dl. Receiver operating characteristic curve (ROC) analysis showed that fibrinogen level at cut off >393 mg/dl, 24 hours prior to PCI, was associated with higher MACCE rates with 0.91 area under curve (AUC); 88.2% sensitivity and specificity 85.7(95% CI 0.82 to 0.96; p<0.0001) (Fig.1). In patients who had MACCE, mean fibrinogen level 24 hours after PTCA was 487.53 (103.58) mg/dl 24 hours after the PCI. ROC analysis showed that fibrinogen level at cut off >427 mg/dl 24 hours after PCI, was associated with higher MACCE rates with 0.85 AUC; 76.5% sensitivity and specificity 90.5% (95% CI 0.75 to 0.92; p<0.0001) (Fig.2).
On comparative analysis, significantly more patients with baseline serum fibrinogen more than 393 mg/dL experienced rehospitalization for UA (p<0.0001), unplanned revascularization (p=0.003) and stent thrombosis (p=0.003) as compared to patients with serum fibrinogen less than 393 mg/dL 24 hours before PTCA (Table 3). Similar results were seen when comparing patients with fibrinogen levels less than and more than 427 mg/dL, 24 hours post stenting.
|
Table 3. Major adverse cardiac and cerebrovascular events according to fibrinogen level before and after stenting |
||||||
|
Variables |
24 hours before stenting |
p |
24 hours after stenting |
p |
||
|
<393 mg/dl (n=55) |
≥393 mg/dl (n=25) |
<427 mg/dl (n=60) |
≥427 mg/dl (n=20) |
|||
|
Rehospitalization for UA, n(%) |
1(1.8%) |
9(36%) |
<0.0001 |
3(5%) |
7(35%) |
0.002 |
|
Rehospitalization for NSTEMI, n(%) |
0 |
1(4%) |
0.68 |
0 |
1(5%) |
0.56 |
|
Re-vascularization, n(%) |
0 |
5(20%) |
0.003 |
0 |
5(25%) |
0.0005 |
|
Stent thrombosis, n(%) |
0 |
5(20%) |
0.003 |
0 |
5(25%) |
0.0005 |
|
TIA/ Ischemic Stroke/ Hemorrhagic stroke, n(%) |
1(1.8%) |
0 |
0.68 |
1(1.7%) |
0 |
0.56 |
|
Death n(%) |
0 |
0 |
- |
0 |
0 |
- |
|
NSTEMI- non ST-elevation myocardial infraction, TIA- transient ischemic attack, UA-unstable angina |
||||||
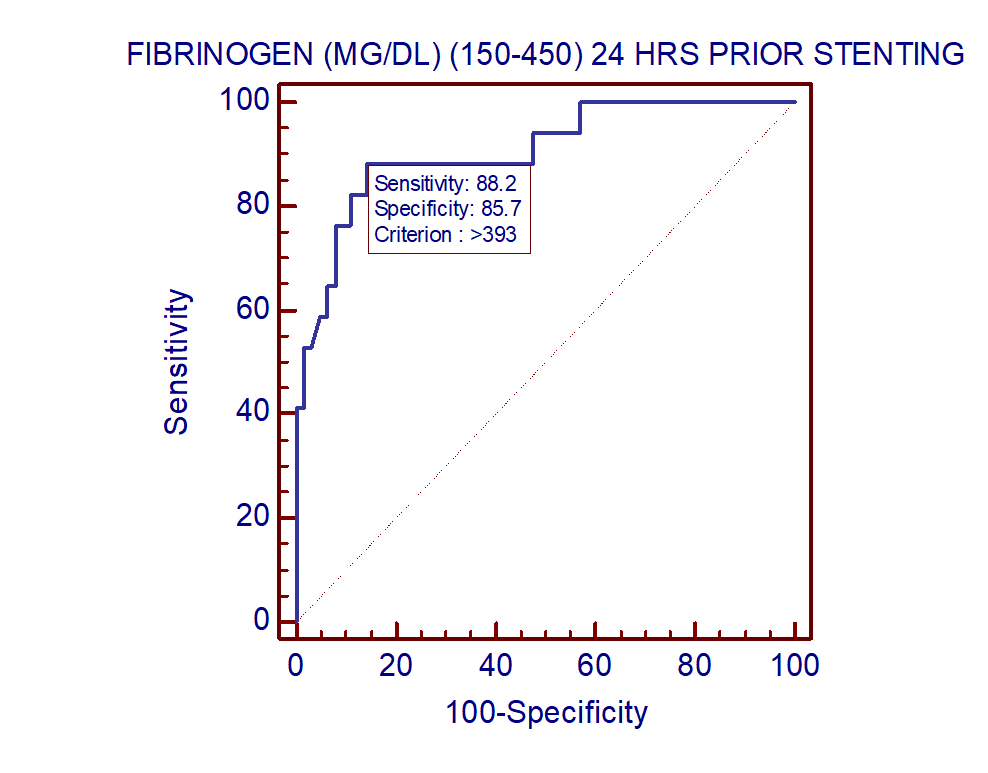
Figure 1. Receiver operating characteristic curve (ROC) of fibrinogen level 24 hours prior to percutaneous coronary intervention associated with MACCE shows 0.91 AUC (95% CI 0.82 to 0.96; p<0.0001) with 88.2% sensitivity and specificity of 85.7%
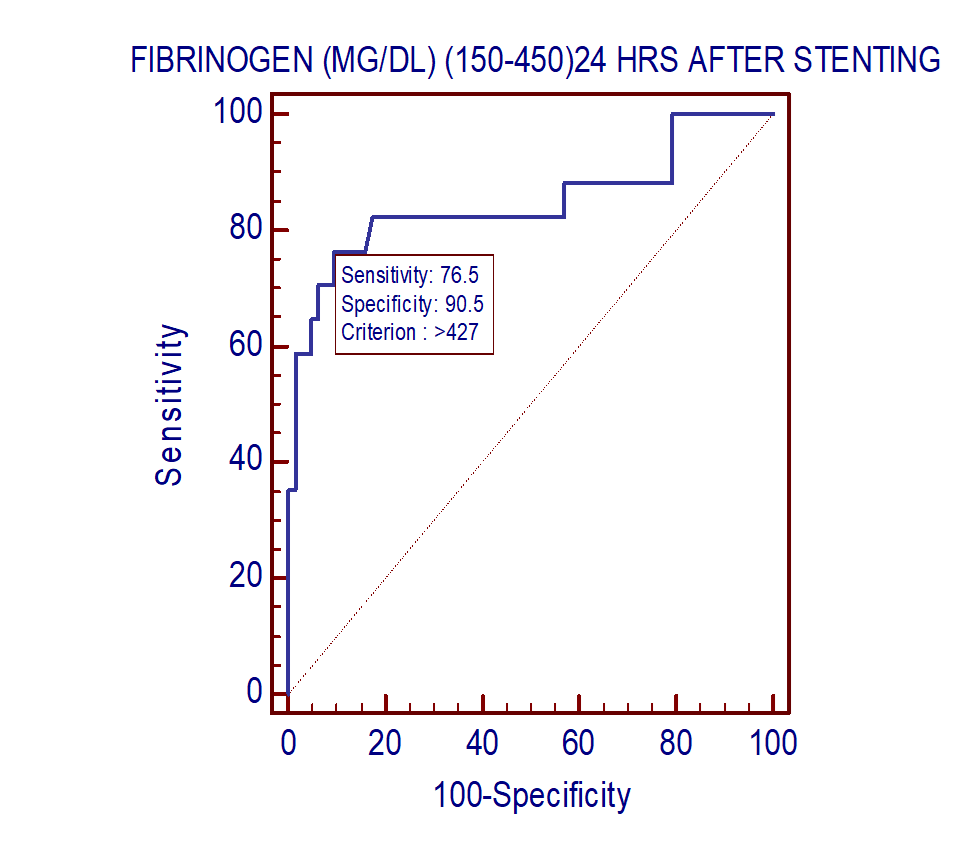
Figure 2. Receiver operating characteristic curve (ROC) of 24 hours fibrinogen level post percutaneous coronary intervention associated with MACCE shows 0.85 AUC (95% CI 0.75 to 0.92; p<0.0001) with 76.5% sensitivity and specificity of 90.5%
Distribution of risk factors like DM-II (p=0.43), hypertension (p=0.53) and smoking (p=0.22) was not associated with fibrinogen level. Fibrinogen level was associated with presenting event. There were more patients in ≥393 mg/dl group (24%), who presented with NSTEMI as compared to <393 mg/dL group (3.6%) (p=0.02). Also, patients with CSA had lower level of serum fibrinogen levels (p=0.01). Biomarkers like troponin I and CK-MB were also elevated in ≥393 mg/dl fibrinogen level group (p=0.02) likely due to higher patients with NSTEMI in this group. ![]()
|
Table 4. Distribution of risk factors, presenting events and biochemical parameters according to levels of fibrinogen before and after stenting |
||||||
|
Variables
|
24 hours before stenting |
p |
24 hours after stenting |
p |
||
|
<393 mg/dl (n=55) |
≥393 mg/dl (n=25) |
|
<427 mg/dl (n=60) |
≥427 mg/dl (n=20) |
||
|
Male, n(%) |
42(76.4) |
22(88) |
0.37 |
45(75) |
19(95) |
0.05 |
|
Female, n(%) |
13(23.6) |
3(12) |
|
15(25) |
1(5) |
|
|
Diabetes mellitus type 2, n(%) |
17(30.9) |
10(40) |
0.43 |
18(30) |
9(45) |
0.22 |
|
Hypertension, n(%) |
37(67.3) |
15(60) |
0.53 |
40(66.7) |
12(60) |
0.59 |
|
Smoking, n(%) |
10(18.2) |
7(28) |
0.22 |
12(20) |
5(25) |
0.98 |
|
Coronary artery disease types, n(%) |
||||||
|
ACS-NSTEMI |
2(3.6) |
6(24) |
0.02 |
4(6.7) |
4(20) |
0.2 |
|
ACS-UA |
6(10.9) |
1(4) |
0.56 |
7(11.7) |
0 |
0.25 |
|
Stable angina |
36(65.5) |
8(32) |
0.01 |
37(61.7) |
7(35) |
0.07 |
|
STEMI |
11(20) |
10(40) |
0.11 |
12(20) |
9(45) |
0.06 |
|
MACCE |
2(3.6) |
15(60) |
<0.0001 |
4(6.7) |
13(65) |
<0.0001 |
|
Biochemical parameters |
|
|
|
|
|
|
|
Hemoglobin, mg/dl |
13.08 (1.16) |
12.41 (2.01) |
0.06 |
13.18 (1.34) |
11.93 (1.6) |
0.001 |
|
Creatinine, mg/dl |
12.41 (2.01) |
0.82 (0.19) |
0.2 |
0.84 (0.15) |
0.9 (0.21) |
0.18 |
|
Troponin I, ng/L |
3.69 (13.00) |
13.19(19.74) |
0.02 |
5.12 (14.25) |
11.78 (19.97) |
0.12 |
|
CK-MB, U/L |
38.42 (72.84) |
89.6(114.09) |
0.02 |
49.65(90.77) |
71.55(92.96) |
0.36 |
|
ACS- acute coronary syndrome, CK-MB- creatine kinase-myoglobin binding, NSTEMI- non ST-elevation myocardial infraction, UA- unstable angina, STEMI- ST-elevation myocardial infraction,
|
||||||
In patients who had MACCE, mean stent diameter was 2.69 (0.38) mm and mean stent length was 32.0 (5.83) mm. ROC analysis showed that coronary stent diameter with a cut off 2.75 mm was associated with higher MACCE rates with AUC 0.75; sensitivity of 76.5% and specificity of 66.7% (95% CI 0.64 to 0.84; p=0.001). 23.5% of patients with coronary stent diameter >2.75mm was associated with MACCE, as compared to 76.5% of patients with stent diameter <2.75 mm.
Binary logistic regression was used to find out the predictors of MACCE (Table 5). Regression analysis for baseline fibrinogen level showed odds ratio 1.68 (95% CI 0.82-3.44; p=0.15), and 1.24 for fibrinogen level 24 hours post PTCA (95% CI 0.59-2.58; p=0.57). Stent diameter < 2.75 mm had odds ratio 5.02 (95% CI 2.50-10.05; p<0.0001). According to multiple regression analysis higher fibrinogen level was seen in patients suffering from MACCE but association for same could not be established and requires further investigation. However, stent diameter independently predicts MACCE.
Discussion
The current study demonstrates that higher level of periprocedural plasma fibrinogen is seen more in patients with MACCE after elective PTCA. Also, use of small calibre stents was associated with higher MACCE, but neither the stent length nor the presenting event for PTCA was associated with MACCE. ![]()
|
Table 5. Regression analysis for the predictors of MACCE |
|||
|
Variables |
Odds ratio |
95% CI lower-upper |
p |
|
Serum fibrinogen 24 hours prior stenting |
1.68 |
0.82 to 3.44 |
0.15 |
|
Serum fibrinogen 24 hours after stenting |
1.24 |
0.59 to 2.58 |
0.57 |
|
Stent diameter |
5.02 |
2.50 to 10.05 |
<0.0001 |
|
MACCE - major adverse cardiac and cerebrovascular events |
|||
Similar to us, Kavitha et al. (10) reported the mean baseline plasma fibrinogen levels to be higher in patients who developed repeat angina and myocardial infarction post stenting. Also, serial measurements of fibrinogen levels remained higher in patients with adverse events (p=0.003) (10).
In a study by Otsuka et al. (11), patients with pre-procedural fibrinogen level >345 mg/dL had greater occurrence of cardiac death, target vessel myocardial infarction and target lesion revascularization after undergoing PTCA. They concluded that higher pre-procedural fibrinogen level was an independent predictor of coronary stent outcome (11). Another study by Mahmud et al. (12) showed that baseline fibrinogen value greater than 360.2 (135.5) mg/dL was associated with higher MACCE after PCI in the form of periprocedural myocardial infarction, re-hospitalization for ACS, urgent revascularization, stroke and death (12). The Dual Antiplatelet Therapy (DAPT) study also identified multiple factors predicting late ischemic events including the use of smaller-diameter stents, similar to the current study (13). Studies by Germing et al and Rahel et al, also suggested increased levels of fibrinogen to be associated with adverse cardiac events after intracoronary stenting (14, 15) Song et al. (16) also reported higher fibrinogen level to predict death or nonfatal re-infarction in patients who underwent PCI (16). Long term outcome of fibrinogen was also assessed in a study by Yuan et al. (17). Elevated fibrinogen levels were associated with all-cause mortality and cardiac mortality at median follow up of 5.1 years. It is possible that a higher fibrinogen threshold predicts ischemic risk during PTCA due to administration of potent antiplatelet and anticoagulant therapy, while a lower threshold might be associated with longer-term MACCE.
Proposed mechanism of fibrinogen role in athero-thrombosis
Fibrinogen has several effects in the event of atherosclerosis. It can infiltrate into the arterial wall and bind low-density cholesterol and other clotting factors. Fibrinogen degradation products (FDP) stimulate smooth muscle cell proliferation in tunica media and loading of cholesterol in macrophages. It elevates plasma viscosity due to higher molecular weight and asymmetricity. Fibrinogen binds to red cells and stimulates red cell accumulation further increasing plasma viscosity. Fibrinogen increases adhesion of leukocytes and platelets to coronary plaques by interaction with ICAM-1 on leukocytes and endothelial cells. It increases platelet aggregation by binding to platelet Gp IIb/IIIa. It also increases platelet reactivity. It also participates in later stages of coagulation cascade leading to thrombosis (3, 4).
A better understanding of other fibrinogen characteristics such as concentration variation with age or clinical presentation, variation in isoforms, intracellular storage and release and binding characteristics may further refine the relations between an elevated fibrinogen level and MACCE after PTCA.
Stent characteristics predicting MACCE
Plitt et al. found stent diameter less than 2.5 mm to be associated with higher events of target vessel revascularization and myocardial infarction at 1 year follow up (18). Small vessel diameter of reference vessel <2.5 mm is usually associated with female gender, diabetes mellitus, calcification and more extensive CAD. Hence, stenting of such lesions is associated with lower success rates (19). A study by Xu et al. (20) also suggested that “bigger was better” and stent diameters more than 2.5 mm were associated with lesser target vessel revascularizations.
Study limitations
Only incidence of adverse events during six-month follow- up was assessed. Longer outcomes need to be assessed. Angiographic follow-up was not done and hence percentage of restenosis was not determined. Post-PCI dual antiplatelet therapy and thienopyridine selection was determined at time of discharge after index procedure and may have been subsequently modified.
Conclusion
The current study demonstrates that baseline fibrinogen, post procedural fibrinogen and stent diameter are independent predictors of 6-month major adverse cardiac and cerebrovascular events after elective percutaneous coronary intervention.
Ethics: Informed consent was obtained from all individual participants
The study has been approved by the institutional ethics committee (UNMICRC/CARDIO/2016/14).
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: T.B., A.Sh., R. P., G.S., A.M., L.S., K.P., I.P., U.P. equally contributed to preparation of manuscript and fulfilled authorship criteria.
Acknowledgement and funding: This work was supported by U. N. Mehta Institute of Cardiology and Research Centre itself and received no specific grant from any funding agency, commercial or not for profit sectors
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

