Acute Coronary Syndrome in Older Adults: an Update from the 2022 Scientific Statement by the American Heart Association
REVIEW
Acute Coronary Syndrome in Older Adults: an Update from the 2022 Scientific Statement by the American Heart Association
Article Summary
- DOI: 10.24969/hvt.2023.367
- Page(s): 7-10
- RELEVANT DISCIPLINES
- Published: 14/01/2023
- Received: 10/01/2023
- Accepted: 12/01/2023
- Views: 8647
- Downloads: 4671
-
Citations
- Keywords: Acute coronary syndrome, heart disease, aged, frailty, multimorbidity, polypharmacology, AHA Scientific Statements
PDF PRINT VERSION CommentsAddress for CorrespondenceAddress for Correspondence: Stefano Cacciatore, Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS
L.go A. Gemelli 8, 00168, Rome, Italy Email: stefanocacciatore@live.it ORCID ID: 0000-0001-7504-3775
Stefano Cacciatore, Anna Maria Martone, Matteo Tosato, Francesco Landi
Department of Geriatrics and Orthopaedics, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, L.go Agostino Gemelli 8, Rome, Italy
Abstract
On December 2022, the American Heart Association (AHA) released a new scientific statement on management of acute coronary syndrome (ACS) in older adults. (1) Here we summarize and comment on some of the key points from the paper.
Key words: Acute coronary syndrome, heart disease, aged, frailty, multimorbidity, polypharmacology, AHA Scientific Statements
Acute coronary syndrome (ACS) pathophysiology in elderly
Elderly patients frequently present with a number of age-related changes that increase their risk of ACS (Fig. 1) (1).
Fibrotic degeneration increases arterial stiffness, determining increased impedance to left ventricular (LV) ejection, dysregulation of blood pressure, and a higher myocardial O2 demand. To compensate for increased impedance, hypertrophy develops in cardiac myocytes, resulting in altered LV contraction and increased myocardial stiffness. Potential consequences are higher resistance to coronary perfusion, predisposition to atrial fibrillation and heart failure with preserved ejection fraction. Decreased responsiveness to β-adrenergic stimulation determines downregulation of inotropic, lusitropic, and chronotropic responses. Endothelial dysfunction impairs the self-regulation capacity of coronary arteries, preventing them from increasing blood flow in response to increased demand. A shift towards a pro-thrombotic phenotype increases the risk of both venous and arterial thromboembolism, and chronic inflammation (inflammaging) increases atherogenesis. Furthermore, aging also affects the kidney.
The authors recommend a careful assessment of renal function and proper kidney-saving measures during diagnostic and therapeutic procedures. Due to decreased muscle mass, the estimated glomerular filtration rate calculated using serum creatinine may be overestimated. (1)
ACS and geriatric syndromes
The authors highlight that people with a higher cardiovascular risk frequently present with multiple geriatric syndromes (1). Geriatric syndromes are multifactorial clinical conditions that do not fall under the “disease” category, but are responsible for complex clinical presentation of diseases, physical and cognitive decline, and poor outcomes (2).
Frailty represents the cornerstone of geriatric medicine. It is a measurable state of vulnerability to developing increased dependency and/or mortality when exposed to a stressor.
Measuring frailty can provide prognostic and therapeutic information that eludes many disease-centered measurement tools. Indeed, some authors have emphasized the significance of frailty in predicting major bleeding (3). Boreskie et al. (4) highlight the main issues arising in various clinical settings and list possible frailty assessment methods which may be more appropriate in each context. Clinical Frailty Scale (CFS), for example, is a quick assessment tool that can accurately predict mortality, clinical course, and adverse events. It can be combined with instruments that take into account more variables, such as the Frailty Index or Fried’s Criteria, to provide a more precise evaluation (4).
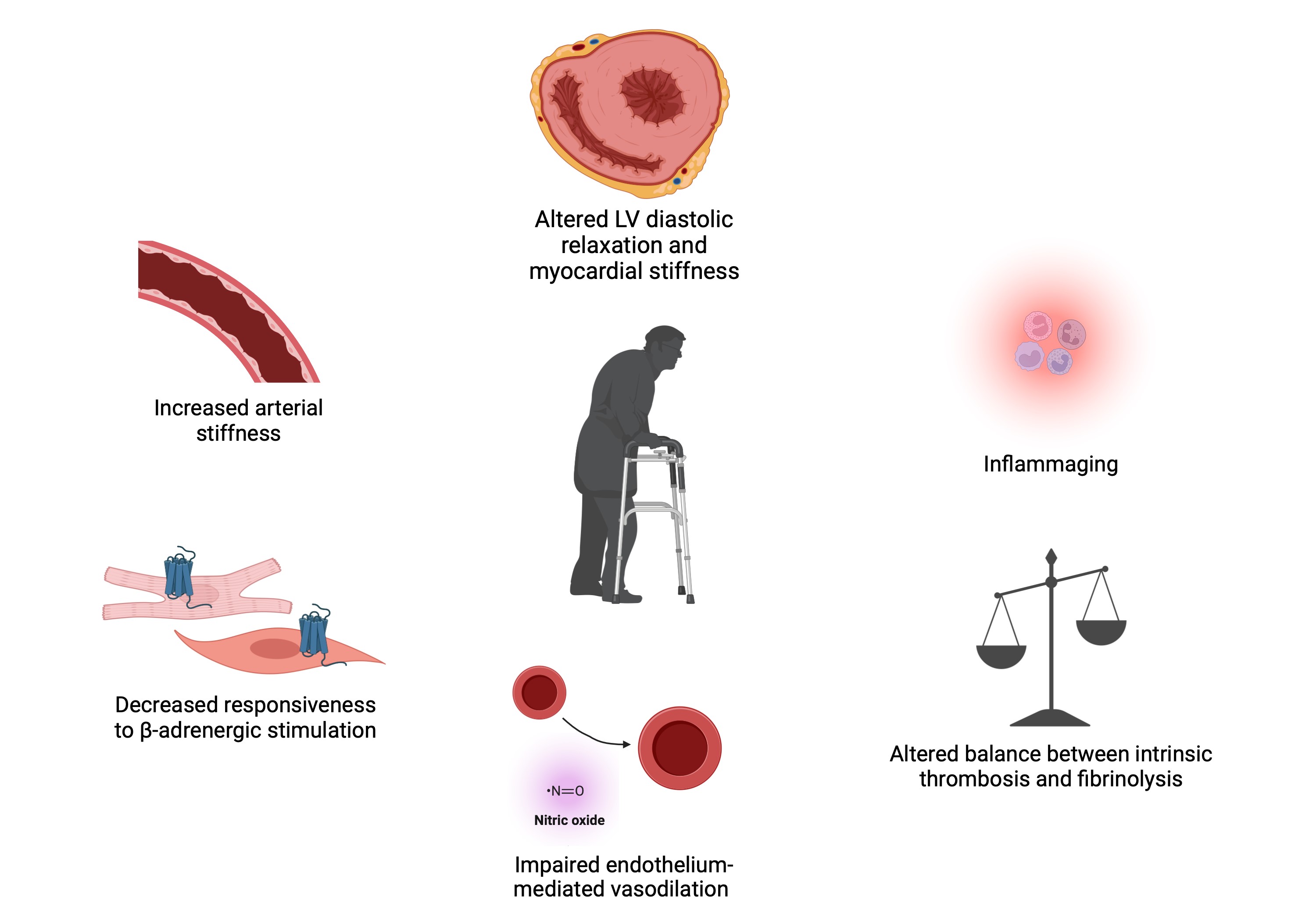
Figure 1. Age-related changes predisposing to acute coronary syndrome (Created with BioRender.com by authors based on recommendations from reference 1)
Frail patients are more vulnerable to delirium. Delirium leads to longer hospital stays, rehospitalization, functional decline, falls, institutionalization, and death. Disorientation, sensory impairment, pain, bed rest, sedation, and medications should all be avoided as delirium-precipitating factors.
Multimorbidity (≥ 2 chronic conditions) is a potential confounder for clinical ACS presentation and a potential predictor of adverse outcomes. Furthermore, polypharmacy (the use of multiple medications, ≥ 5), leads to pharmacological interactions and may compromise the implementation of an optimal treatment (1).
Cognitive decline may present either as mild cognitive impairment (MCI) or dementia. Reduced cognitive function occurs in MCI without loss of function. In dementia, cognitive dysfunction interferes with daily activities and leads to loss of independence. The mere presence of cognitive impairment, according to the AHA, is not an exclusion criterion for denying diagnostic and therapeutic interventions. Nonetheless, it should be taken into account in clinical evaluations and when determining the appropriateness of invasive procedures (1).
Management of ACS in elderly
The AHA statement addressed the dependability of cardiac biomarkers. The standard of care for detecting myocardial injury is high-sensitivity cardiac troponin I (hs-cTn). However, certain conditions, such as myocardial fibrosis or chronic kidney disease, can result in higher baseline values and a lower positive predictive value (1).
Compared with the first scientific statement on Acute Coronary Care in the Elderly published in 2007, (5, 6) the latest document reported that more randomized controlled trials (RCTs) have involved older adults (1).
Both the After Eighty (2016) (7) and the SENIOR-NSTEMI (2020) (8) studies included patients over the age of 80, and both found that invasive treatments outperformed conservative treatments for non-ST-elevation (NSTE)-ACS and non-ST- elevation myocardial infarction (NSTEMI). The Italian Elderly ACS (2012, patients aged ≥ 75 with NSTE-ACS) (9), the MOSCA trial (2016, patients aged ≥ 70 with NSTEMI) (10), and a RCT by Hirlekar et al. (2020, patients aged ≥80 years old with NSTE-ACS) (11) found no long-term differences in invasive vs conservative treatments.
RINCAL (2021) (12) concluded that an invasive approach was not superior to optimized medical therapy alone in treating patients aged ≥80 with NSTEMI. Unpublished data from the recently concluded MOSCA-Frail trial (2019) (13) revealed no benefit of invasive strategy on primary or co-primary end-points in older adults with NSTEMI (1).
Interestingly, AHA Scientific Statement points out that among those trials, only the MOSCA-Frail and Hirlekar et al. (11, 13) conducted frailty assessment. MOSCA-Frail enrolled patients with a CFS score of 4 or higher (13). Hirlekar et al. (11) used the Canadian Study of Health and Aging Clinical Frailty Scale, reporting a low prevalence of frailty in their sample and not stratifying results based on frailty status. The lack of a widely used assessment of frailty represents a significant limitation for trials on the therapeutic management of ACS in the elderly.
Cardiovascular diseases are often associated with progressive disability. AHA identifies incorrect management and suboptimal transition of care as potential causes of loss of independence (1).
Management of ACS in elderly patients should be tailored to the patients' preferences, quality of life, and life expectancy. This includes deciding whether to use invasive or noninvasive treatment for isolated coronary artery disease (CAD) or a combination of CAD and other conditions (e.g., aortic stenosis) (14), as well as medical treatment after the acute phase. In this regard, Sabouret et al. (15) recently questioned the long-term use of antiplatelet therapy. In fact, in older patients, the benefit of preventing ischemic events does not always outweigh the risk of major bleeding. For this reason, the authors recommend keeping a critical eye on medication reviews and tailoring interventions to the individual patient.
An important section focuses on patients approaching the end-of-life. For them, AHA recommends focusing on outcomes such as avoiding re-hospitalizations and relieving pain and discomfort. A multidisciplinary discussion may aid in determining a treatment's lack of medical efficacy (futility). Before invasive procedures, do-not-resuscitate orders should be carefully discussed with the patient, family, or power of attorney (1).
A proper discharge from the hospital and continuity of care are essential for improving outcomes and reducing disability. A RCT conducted by Sanchis et al. (16) discovered that intensive cardiac rehabilitation was beneficial in older survivors of an acute myocardial infarction. Again, as Bencivenga et al. (17) point out, assessing frailty is critical for determining prognosis and treatment goals in the elderly after the acute phase. At discharge, the AHA Statement suggests considering a medication review and de-prescribing, lifestyle modifications and cardiac rehabilitation, comorbidity management, psychosocial support, socioeconomic factors, and education of both patients and caregivers. All of these domains are part of the comprehensive geriatric assessment. Furthermore, at follow-up, the AHA recommends focusing on symptom burden, functional status, and quality of life.
The two sides of ACS management in geriatric patients
A recent paper by Roth et al. (18) highlighted that cardiovascular risk has grown globally from 1990 to 2019. According to the authors, one of the main demerits in this regard is not having effectively translated prevention knowledge into practice.
The situation may be even worse after COVID-19 pandemic. In recent years, elderly population saw a dramatic deterioration in quality-of-life and well-being (19). The Pandemic showed also that longevity does not always come with "healthy aging" and "healthy frailty" (20). For this reason, one could provocatively say that proper management of ACS in the elderly begins in childhood (21). The Longevity Check-up 7+ initiative conducted by our group (2015 - ongoing) showed that in community-dwelling population the presence of poorly controlled risk factors is often accompanied by low awareness (22). One point that needs to be strongly emphasized is that all forms of prevention may help reducing the burden of cardiovascular diseases. An example is influenza vaccination in the elderly. Albeit not directly acting on cardiovascular risk, it can be effective in reducing influenza-related cardiovascular complications (23).
Although not further explored by the AHA Scientific Statement, frailty is related to sarcopenia. Sarcopenia is a decrease in muscle quality and quantity and represents a powerful predictor of adverse outcomes, including for ACS. (24). an intervention based on physical exercise and proper nutrition could bring about a more robust generation of older adults (25).
Therefore, the final paragraph of this editorial would like to serve as a little addition to the AHA Scientific Statement. The geriatric approach today cannot but be two-sided. Respect for individual expectations, human dignity, and death assume an ever more holy significance as one approaches the end of life. However, in order to achieve more sustainable health care, ensure a higher quality of life, and truly make a difference, a careful assessment of the patient in order to set commensurate goals becomes a critical aspect at all stages of life.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: All authors participated in manuscript design and drafting. All authors read and approved the final version.
Acknowledgement and funding: None to declare
Authors’ disclosure: The authors have not declared a specific grant for this work from any funding agency in the public, commercial or not-for-profit sectors.
References
1.Damluji, A.A., Forman DE, Wang TY, Chikwe J, Kunadian V, Rich MW, et al., Management of acute coronary syndrome in the older adult population: A Scientific Statement From the American Heart Association. Circulation, 2022; doi:10.1161/CIR.0000000000001112 https://doi.org/10.1161/CIR.0000000000001112 PMid:36503287 2.Inouye SK, Studenski S, Tinetti ME, Kuchel GA.. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 2007; 55: 780-91. https://doi.org/10.1111/j.1532-5415.2007.01156.x PMid:17493201 PMCid:PMC2409147 3.Spadafora L, Bernardi M, Galli M, Biondi-Zoccai G, Sabouret P. Which future for aspirin in acute coronary syndromes treated with percutaneous coronary intervention? An overview on aspirin-free strategies. Arch Med Sci 2022; 18: 1689-92. https://doi.org/10.5114/aoms/155411 PMid:36457983 PMCid:PMC9710287 4.Boreskie KF, Hay JL, Boreskie PE, Arora RC, Duhamel TA. Frailty-aware care: giving value to frailty assessment across different healthcare settings. BMC Geriatr 2022; 22: 13. https://doi.org/10.1186/s12877-021-02722-9 PMid:34979966 PMCid:PMC8722007 5.Alexander KP, Newby KL, Armstrong PW, Cannon CP, Gibler WB, Rich MW, et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation 2007; 115: 2549-69. https://doi.org/10.1161/CIRCULATIONAHA.107.182615 https://doi.org/10.1161/CIRCULATIONAHA.107.182616 6. Alexander KP, Newby KL, Armstrong PW, Cannon CP, Gibler WB, Rich MW, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation 2007; 115:2570-89. https://doi.org/10.1161/CIRCULATIONAHA.107.182615 https://doi.org/10.1161/CIRCULATIONAHA.107.182616 PMid:17502591 7. Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, Aakhus S, et al. Invasive versus conservative strategy in patients aged 80 years and older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): an open-label randomized controlled trial. Lancet 2016; 387: 1057-65. https://doi.org/10.1016/S0140-6736(15)01166-6 PMid:26794722 8. Kaura A, Sterne JAC, Trickey A, Abbott S, Mulla A, Glampson M, et al. Invasive versus non-invasive management of older patients with non-ST elevation myocardial infarction (SENIOR-NSTEMI): a cohort study based on routine clinical data. Lancet 2020; doi: 10.1016/S0140-6736(20)30930-2 https://doi.org/10.1016/S0140-6736(20)30930-2 PMid:32861307 9.Savonitto S, Cavallini C, Petronio AS, Murena E, Antonicelli R, Sacco A, et al. Early aggressive versus initially conservative treatment in elderly patients with non-ST-elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovas Interv 202; 5: 906-16. https://doi.org/10.1016/j.jcin.2012.06.008 PMid:22995877 10.Sanchis J, Nunez E, Barrabes JA, Marin F, Consuegra-Sanches L, Ventura S, et al. Randomized comparison between the invasive and conservative strategies in comorbid elderly patients with non-ST elevation myocardial infarction. Eur J Intern Med 2016; 35: 89-94. https://doi.org/10.1016/j.ejim.2016.07.003 PMid:27423981 11. Hilrekar G, Libungan B, Karlsson T, Back M. Percutaneous coronary intervention in the very elderly with NSTE-ACS: the randomized 80+ study. Scand Cardiovasc J 2020; doi: 10.1080/14017431.2020.1781243 https://doi.org/10.1080/14017431.2020.1781243 PMid:32586153 12. de Belder A, Myat A, Blaxill J, Haworth P, O'Kane PD, Hatrick R, et al. Revasularisation or medical therapy in elderly patients with acute angina syndromes: the RINCAL randomized trial. Eurointervention 2021; 17: 67-74 https://doi.org/10.4244/EIJ-D-20-00975 PMid:33226000 13. Sanchis J, Ariza-Sole A, Abu-Assi E, Alegre O, Alfonso F, Barrabes JA, et al. Invasice versus conservative strategy in frail patients with NSTEMI: the MOSCA-FRAIL clinical study trial design. Rev Esp Cardiol 2019; 72; 154-9. https://doi.org/10.1016/j.rec.2018.02.007 PMid:29525724 14.Spadafora L, Bernardi M, Giuseppe Biondi-Zoccai, Giacomo F. Coronary artery bypass grafting added to surgical aortic valve replacement in octogenarians. Interact Cardiovasc Thorac Surg 2022; 35: doi: 10.1093/ijvts/iva191 https://doi.org/10.1093/icvts/ivac191 PMid:35876811 PMCid:PMC9338703 15.Sabouret P, Spadafora L, Fischman D, Ullah W, Zeitoni M, Gulati M, et al. De-escalation of antiplatelet therapy in patients with coronary artery disease: Time to change our strategy? Eur J Intern Med, 2022; doi: 10.1016/j.ejim.2022.12.008 https://doi.org/10.1016/j.ejim.2022.12.008 PMid:36575107 16. Sanchis J, Sasatre C, Ruescas A, Ruiz V, Valero E, Bonanad C, et al., Randomized comparison of exercise intervention versus usual care in older adult patients with frailty after acute myocardial infarction. Am J Med 2021; 134: 383-9.0 https://doi.org/10.1016/j.amjmed.2020.09.019 PMid:33228950 17.Bencivenga L, Femminella GD, Ambrosino P, Bosco Q, De Lucia C, Perrotta G, et al., Role of frailty on cardiac rehabilitation in hospitalized older patients. Aging Clin Exp Res 2022; 34: 2675-82. https://doi.org/10.1007/s40520-022-02220-x PMid:36065074 PMCid:PMC9675689 18.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour E, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol 2020; 76: 2982-3021. https://doi.org/10.1016/j.jacc.2020.11.010 PMid:33309175 PMCid:PMC7755038 19.Tosato M, Ciciarello F, Zazzara MB, Janri D, Pais C, Cacciatore S, et al. Lifestyle changes and psychological well-being in older adults during COVID-19 pandemic. Clin Geriatr Med 2022; 38: 449-59. https://doi.org/10.1016/j.cger.2022.05.002 PMid:35868665 PMCid:PMC9080082 20.Zahran S, Altringer L, Prasad A. The longevity-frailty hypothesis: evidence from COVID-19 death rates in Europe. Int J Environ Res Public Health, 2022. 19(4). https://doi.org/10.3390/ijerph19042434 PMid:35206622 PMCid:PMC8872087 21.McGill HC Jr, McMahan CA, Herderick EE, Malcom GT, Tracy RE, Strong JP. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr 2000; 72 (5 Suppl): 1307S-15S. https://doi.org/10.1093/ajcn/72.5.1307s PMid:11063473 22.Marzetti E, Calvani R, Picca A, Sisto A, Tosato M, Martone Am, et al., Prevalence of dyslipidaemia and awareness of blood cholesterol levels among community-living people: results from the Longevity check-up 7+ (Lookup 7+) cross-sectional survey. BMJ Open 2018. 8: e021627. https://doi.org/10.1136/bmjopen-2018-021627 PMid:29961030 PMCid:PMC6045760 23.Vardeny, O. Influenza vaccine in cardiovascular disease: time to move the needle. Eur Heart J 2022; 43: 4389-91. https://doi.org/10.1093/eurheartj/ehac491 PMid:36030399 24.Kim CH, Rhee TM, Park KW, Park CS, Kang J, Han JK, et al., Association between low muscle mass and prognosis of patients with coronary artery disease undergoing percutaneous coronary intervention. J Am Heart Assoc 2021; 10: e018554. https://doi.org/10.1161/JAHA.120.018554 PMid:33372526 PMCid:PMC7955465 25.Bernabei R, Landi F, Calvani R, Cesari M, Del Signori D, Anker SD. et al., Multicomponent intervention to prevent mobility disability in frail older adults: randomised controlled trial (SPRINTT project). BMJ 2022. 377: p. e068788. https://doi.org/10.1136/bmj-2021-068788 PMid:35545258 PMCid:PMC9092831 Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.Archive of Issues
AUTHOR'S CORNER
 Authors having problems with submissions please notify editor: editor@hvt-journal.com
Authors having problems with submissions please notify editor: editor@hvt-journal.com
