A rare coronary artery anomaly - type X dual left anterior descending artery: a case report with brief literature review
CASE REPORT
A rare coronary artery anomaly - type X dual left anterior descending artery: a case report with brief literature review
Article Summary
- DOI: 10.24969/hvt.2023.371
- Page(s): 58-61
- CARDIOVASCULAR DISEASES
- Published: 24/01/2023
- Received: 27/12/2022
- Revised: 15/01/2023
- Accepted: 16/01/2023
- Views: 4840
- Downloads: 4303
- Keywords: coronary artery anomaly, left anterior descending artery, type x dual left anterior descending artery, electrocardiography gating coronary CT angiography
Address for Correspondence: Ferhat Piskin, Department of Radiology, Medical Faculty, Cukurova University, Adana, Turkey Email: ferhatcanpiskin@gmail.com
Ferhat Piskin, Duygu Ozgul, Erol Huseyn Aksungur
Department of Radiology, Medical Faculty, Cukurova University, Adana, Turkey
Abstract
Introduction
Type X dual left anterior descending artery (LAD), which is a rare subtype of coronary artery anomalies and newly defined in the literature, usually presents an asymptomatic clinical course and is detected incidentally in diagnostic angiography. However, in the presence of obstructive disease, myocardial revascularization may be required. It is critical to identify the presence of Type X dual LAD in order to prevent misdiagnoses in coronary angiography and to prevent complications during angioplasty or surgical myocardial revascularization. We present a case of rare type X dual LAD coronary anomaly presented with chest pain.
Case presentation: A 66-year-old female patient was admitted to the hospital with the complaints of atypical chest pain and palpitations. Examinations revealed sinus tachycardia, mitral valve calcific degeneration, mild tricuspid valve insufficiency, and left atrial dilatation on echocardiography, hyperlipidemia and normal troponin I value.
Coronary artery disease risk (according to the Framingham risk score) was low (8%), and coronary coronary computed tomography angiography (CCTA). The calcium score was calculated as 1782 Agatston. There were calcified atheroma plaques in the left main coronary artery (LMCA) ostium and distal section causing less than 25% stenosis. A well-developed diagonal branch of LAD was observed. The LAD calibration was thin and terminated at the proximal of anterior interventricular sulcus (AIVS). Therefore, it was evaluated as short LAD. A long LAD was detected, which was arising from the right coronary sinus with a separate ostium, reached the AIVS at the midventricular level after a pre-pulmonic course in front of the right ventricular outflow tract and extended to the apex. The long LAD was located in front of the right ventricle, close to the anterior chest wall.
As there were no signs of myocardial ischemia or injury, calcified lesions in coronary arteries were nonstenotic (excluding thus acute coronary syndrome as cause of chest pain) the medical treatment with antilipidemia and hypertension and atherosclerosis modifying medications has been started and she was discharged with recommendations to continue treatment, modify risk factors for coronary artery disease and follow-up visits were scheduled.
Conclusion: Our case demonstrated that rare dual type X LAD can be detected by CCTA in a patient evaluated for chest pain. CCTA is a useful tool for detection of coronary anomalies, that should be sought in patients with chest pain, absence of acute myocardial injury and low Framingham risk score.
Key words: coronary artery anomaly, left anterior descending artery, type x dual left anterior descending artery, electrocardiography gating coronary CT angiography
Introduction
Coronary artery anomalies are detected with a frequency of 0.3-1.3% in adult patients undergoing coronary angiography (1). These anomalies are classified as origin, course and termination anomalies (2). It is important to detect coronary artery anomalies in patients presenting with chest pain and similar cardiac symptoms, as they may cause myocardial perfusion disorder, arrhythmia, and sudden cardiac death (3, 4). However, most coronary artery anomalies are asymptomatic and detected incidentally.
Right coronary artery origin, course and termination anomalies are more common than left coronary artery anomalies. Dual left anterior descending artery (LAD) is known as a rare coronary artery anomaly. The
frequency of dual LAD in the general population has been reported as 1% (5).
Dual LAD may accompany congenital heart diseases such as tetralogy of Fallot and transposition of the great arteries. This makes the identification of the presence of dual LAD critically important during the corrective surgery of congenital heart diseases. Spinaldo-Franco et al. (6) proposed an angiographic classification for dual LAD with four subtypes. As a result, of the widespread use of coronary computed tomography angiography (CCTA) and the definition of new subtypes, dual LAD has been started to be evaluated in 9 subtypes (7-9). Celik et al. (10) have proposed a new dual LAD subtype in 2015; this new subtype entered the literature as type X dual LAD.
This case report aims to emphasize the dual LAD entity, which is a rare coronary artery anomaly, to remind its clinical/surgical importance, and to share the third case of Type X Dual LAD in the light of current literature.
Case report
A 66-year-old female patient with a known diagnosis of hypertension was admitted with the complaints of atypical chest pain and palpitations that had been intermittent for 1 month and increased with effort. Her physical effort was within normal limits. Sinus tachycardia was observed on electrocardiography (ECG). Transthoracic echocardiography revealed mitral valve calcific degeneration, mild tricuspid valve insufficiency, and left atrial dilatation. Laboratory tests revealed hyperlipidemia (total cholesterol 277 mg/dL, low-density lipoprotein 165 mg/dL, triglyceride 210 mg/dL). The level of troponin I was in normal value.
Coronary artery disease risk (according to the Framingham risk score) was low as 8%, and coronary CCTA was performed due to ongoing chest pain. Images from different phases were obtained with retrospective ECG gating and these images were evaluated with MPR, MIP and 3D volume rendering techniques (Fig. 1). The calcium score was calculated as 1782 Agatston. There were positively modulated calcified atheroma plaques in the left main coronary artery (LMCA) ostium and distal section causing less than 25% stenosis. A well-developed diagonal branch of LAD was observed. The LAD calibration was thin and terminated at the proximal of anterior interventricular sulcus (AIVS). Therefore, it was evaluated as short LAD. Right coronary artery (RCA) was dominant. A long LAD was detected, which was arising from the right coronary sinus (RCS) with a separate ostium, reached the AIVS at the midventricular level after a pre-pulmonic course in front of the right ventricular outflow tract (RVOT) and extended to the apex. The long LAD was located in front of the right ventricle, close to the anterior chest wall. There were also calcified plaques in the RCA and circumflex coronary artery (LCx) and its branches, which did not cause significant stenosis.
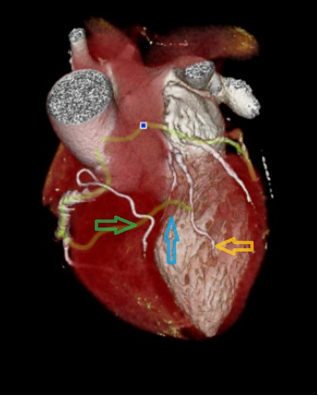
Figure 1. In the three-dimensional volume image of the heart, it is seen in three coronary arteries. The short left anterior descending coronary artery (LAD) terminates proximally in the anterior interventricular groove (AIVS) (Blue arrow). The long LAD from origin left main coronary artery (Yellow arrow) is located to the left of the interventricular groove. The long LAD origin of the right coronary sinus (Green arrow) has a pre-pulmonic course and enters the distal AIVS.
As patient`s electrocardiogram did not show signs of ischemia, there were no signs of myocardial injury – normal troponin I levels and no wall motion abnormalities on echocardiography, and she had dual type X LAD and calcified nonstenotic lesions in coronary arteries (excluding thus acute coronary syndrome as cause of chest pain) the medical treatment with antilipidemia and hypertension and atherosclerosis modifying therapy has been started and she was discharged with recommendations to continue treatment, modify risk factors for coronary artery disease and follow-up visits were scheduled.
Discussion
In patients with low coronary risk, computed tomography angiography (CTA) is a screening method that has come to the fore recently. The frequency of detection of coronary artery anomalies has increased with the use of CTA (11). Coronary artery anomalies, which are mostly asymptomatic and detected incidentally in coronary angiography; may also be associated with atherosclerosis, myocardial perfusion disorder, arrhythmia, and sudden cardiac death (3). Dual LAD is known as a rare coronary artery anomaly (5).
Dual LAD is defined as the presence of two LADs, one of which is poorly developed, in different parts of the anterior interventricular sulcus (AIVS). Spinaldo-Franco et al. (6) proposed an angiographic classification for dual LAD with four subtypes. In types I and II, short LAD progresses to AIVS and originates from major proximal septal perforators and long LAD. In type I, the long LAD runs parallel to the short LAD, on the left ventricular side of the AIVS, and in type II, on the right ventricular side, the AIVS reaches the apex and re-enters the AIVS distally. In type III, the origin of the long LAD is the same as in types I and II. It has an intramyocardial course proximal to the interventricular septum, and epicardial outcome in distal AIVS. In Type IV, unlike the first three types, the long LAD originates from the RCA. In this type, short LAD gives septal and diagonal branches and ends in the middle part of AIVS. The long LAD enters the AIVS after a short pre-pulmonic course and continues to the apex. Type IV dual LAD is very rare compared to the other three subtypes (6, 12). In type X dual LAD, the last defined subtype among other LAD types, which is less common compared to these four better known types in the literature, the short LAD originates from LMCA and ends in the proximal AIVS. The long LAD originates with a separate ostium from the RCS and enters the AIVS distally after the pre-pulmonic course anterior to the RVOT and extends up to the apex. During the long course of LAD, it can travel in front of the right ventricle, just behind the sternum and close to the anterior chest wall (13).
If the long LAD is overlooked during invasive coronary angiography or considered as the conus branch of the RCA, the type X dual LAD variation may be misdiagnosed as an occlusion in the mid-distal segment of the LAD. It should be kept in mind that the long LAD gives septal and diagonal branches. Failure to detect possible atherosclerotic disease in an overlooked long LAD may result in inadequate treatment during surgical revascularization and angioplasty. In addition, the long LAD whose presence and/or course is unknown may be injured during sternotomy due to its course close to the anterior chest wall. Therefore, awareness on the use of coronary CTA and emerging classifications of coronary arteries anomalies is a crucial point for the detection of dual LAD and other possible coronary artery anomalies.
In our case, there was an underdeveloped/short LAD originating from the LMCA and a well-developed diagonal branch belonging to it. The long LAD originates from the RCS, reaches the AIVS after the pre-pulmonic course from the front of the RVOT, and continues to the apex. Although our case was first evaluated as type IV dual LAD, when the images were re-evaluated after re-scanning the current literature, it was seen that long LAD was compatible with type X dual LAD in the current classification, since it originated with an ostium separate from the RCS and, had a pre-pulmonic course and it reached the AIVS. Calcified plaques with positive modulation and no significant stenosis were observed in the LMCA ostium, LCx and RCA. Since there was no indication for invasive coronary angiography and/or coronary angioplasty, the patient was discharged after medical treatment including arrangement for hyperlipidemia, hypertension and coronary artery atherosclerosis, with recommendations and control examinations were planned.
Conclusion: Although coronary artery anomalies are a very broad class, dual LAD is a rarer group and evaluated in 10 subtypes with newly defined subtypes in the current literature. Type X Dual LAD is a fairly newly defined dual LAD subtype that has been reported twice in the literature review. In the absence of stenosis, dual LAD is of little clinical significance. However, in the presence of obstructive disease, surgical or interventional revascularization may be required.
Missing a long LAD or evaluating it as an RCA conus branch during invasive coronary angiography may incorrectly diagnose LAD occlusion and lead to aggressive intervention. In addition, the course of the overlooked long LAD in front of the right ventricle may result in injury during sternotomy. Considering all these reasons together, remembering the rare dual LAD variation in the presence of short or poorly developed LAD in catheter angiography and/or coronary CT angiography examinations will be very helpful in terms of accurate diagnosis and appropriate treatment.
Our case demonstrated that rare dual type X LAD can be detected by CCTA in a patient evaluated for chest pain. CCTA is a useful tool for detection of coronary anomalies, that should be sought in patients with chest pain, absence of acute myocardial injury and low Framingham risk score.
Ethics: Informed written consent was obtained from patient before all procedures
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: F.C.P., D.O. and H.E.A. equally contributed to the case management and manuscript preparation
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

