2022 American Heart Association/American College of Cardiology guidelines for the diagnosis and management of aortic disease: lessons to be drawn
EDITORIALS
2022 American Heart Association/American College of Cardiology guidelines for the diagnosis and management of aortic disease: lessons to be drawn
Article Summary
- DOI: 10.24969/hvt.2023.374
- Page(s): 14-16
- CARDIOVASCULAR DISEASES
- Published: 12/02/2023
- Received: 08/02/2023
- Accepted: 09/02/2023
- Views: 10730
- Downloads: 5495
-
Citations
- Keywords: editorial
PDF PRINT VERSION CommentsAddress for CorrespondenceAddress for Correspondence: Fabio Massimo Oddi, Vascular Surgery Unit, University of Rome “Tor Vergata”, Rome, Italy, Email: Fabio.massimo89@gmail.com ORCID: 0000-0001-8081-807X
Fabio Massimo Oddi1, Giulia Franceschini2, Leonardo Oddi3, Giorgio Fedeli4
1Vascular Surgery Unit, University of Rome “Tor Vergata”, Rome, Italy
2Cardiac and Thoracic Anesthesia Unit, University of Rome “Tor Vergata”, Rome, Italy
3Saint Camillus International University of Health and Medical Sciences (UniCamillus) of Rome, Rome, Italy
4Cardiology department, Guidonia Health District, Asl Roma 5, Italy.
A new guideline has recently been published on the management and diagnosis of aortic diseases by the American College of Cardiology (ACC) and the American Heart Association (AHA); they centered regarding genetic testing and screening, coherent imaging practices, the usefulness of a multidisciplinary aortic team, and the surgical intervention (1).
More than 12 years after the publication of the previous guideline, the ACC/AHA have updated their clinical practice. “2010 ACCF/AHA Guidelines for the Diagnosis and Management of Patients with Thoracic Aortic Disease” and the “2015 Surgery for Aortic Dilation in Patients with Bicuspid Aortic Valves: A Statement of Clarification from the ACC/AHA Task Force on Clinical Practice Guidelines.” have been replaced by this new aortic disease guideline (2, 3). It will be used in addition to “2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease.” (4).
In the last few years, there have been major advances in surgical and endovascular techniques, so there was a real clinical need to provide an updated accumulation of knowledge to guide surgeons, cardiologists and clinicians managing patients with aortic disease.
Among the focal point, the authors target on correct imaging of the aorta and the role of familiar and genetic screening; they define a smaller aortic diameter at which surgical intervention for aneurysms can be considered; and they underline the shared decision-making and the value of a multidisciplinary aortic team.
There are two sections in the guideline devoted to multidisciplinary aortic team and shared decision- making, so much so as to underline how important this is to determine an adequate treatment (surgical or endovascular procedures or medical management), the appropriate timing of intervention and surveillance. The composition of these hospital teams
may differ across centers, but the most-common features, according to the authors, include vascular, endovascular and cardiac surgeons, with experience, specialized in aortic diseases in a center with high- volume interventions of this type; radiologist and imaging specialists with experience in aortic disease who are able to understand the images like computed tomography (CT), magnetic resonance imaging (MRI), or echocardiography; anesthesiologists with experience in aortic disease, especially when there is an acute aortic disease; and intensive care unit specialists able to use their experience that are focused on acute aortic disease. This team should increase a lot the possibility of success for patients with acute aortic disease in particular those requiring an urgent repair or for patients who are pregnant or considering pregnancy.
Another point authors highlighted was the importance of genetics and familiarity in aortic disease. In the previous guideline, only relatives with genetic mutations should undergo aortic imaging. This new guideline recommends family screenings with genetic testing or aortic imaging of first-degree relatives of patients diagnosed with ascending thoracic aortic aneurysm or aortic root aneurysm or aortic dissection to identify individuals most at risk for aortic disease.
There has never been a consistent, agreed-upon way to measure and describe the aorta. There needs to be a consistent method within an institution to both measure and report the aortic diameters, and the methods used to measure those diameters should be included in the report so others reading the report from other institutions know exactly how the measurements were made.
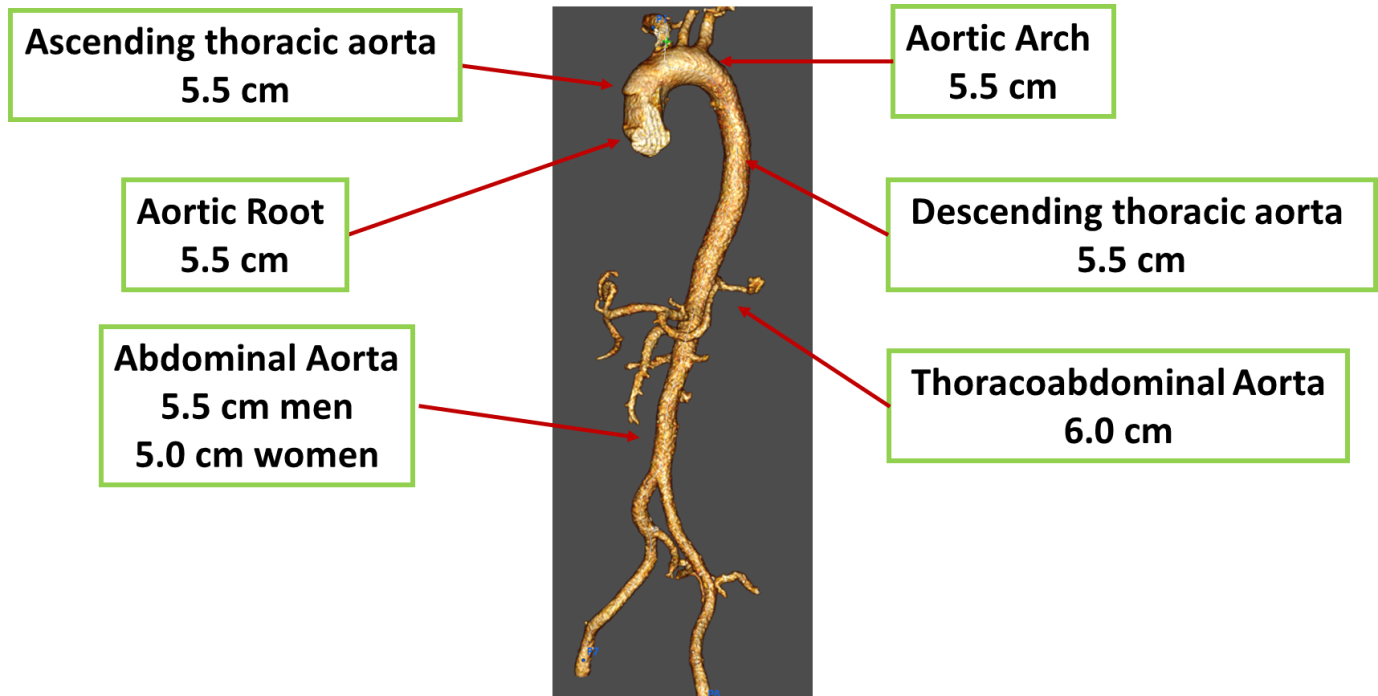
Figure 1. Updated surgical thresholds for sporadic aortic aneurysms in asymptomatic patients
Indeed in this new guideline, there is much more specific guidance on the way CT or MRI are obtained and reported, on the frequency of surveillance before and after intervention by CT, MRI, and echocardiography, on the type of measurement technique (from sinus to sinus and from inner-edge to inner-edge) and on the use of ECG-gated images that decrease motion artifact.
Conventionally, an aneurysm of any artery has been defined as an increase in size of at least 1.5 times what is normal at that zone. The authors report how the term “dilated” should be used for moderate enlargements, with “aneurysm” reserved for more-substantial enlargement.
At centers with experienced surgeons, the guideline include that the threshold for surgery, in asymptomatic patients, has been reduced from 5.5 cm to 5.0 cm for sporadic aortic root and ascending aortic aneurysms (Fig. 1). This threshold may be lower in some patients with heritable thoracic aortic aneurysms, Marfan syndrome, or associated with an increased risk of dissection.
There is an important difference with the clinical practice guidelines of European Society of Vascular Surgery (ESVS) regarding the treatment for descending thoracic aorta aneurysms (TAA). In this new guideline, in patients with intact descending TAAs, repair is recommended when the diameter is ≥5.5 cm. Instead, in ESVS guideline, in fit and unfit patients with favorable anatomy, endovascular repair may be considered for descending thoracic aorta aneurysms with size between 56 and 59 mm in diameter, but it should be considered for descending thoracic aorta aneurysms >60 mm in diameter (5). This difference is not present regarding the treatment of the aortic arch aneurysms, in both guidelines the treatment is considered at a diameter of 55 mm. (6)
Rapid aortic growth is a risk factor for rupture and the definition for rapid aneurysm growth rate has been updated. The guideline recommends the intervention in patients with rapid aneurysm growth of ≥5 mm in 1 year or ≥3 mm/year in 2 consecutive years for those with sporadic aneurysms and ≥3 mm in 1 year for those with heritable thoracic aortic disease or bicuspid aortic valve.
Guideline emphasizes that surgical thresholds should be modified based on size of patient. In patients who are, significantly taller or smaller than average, surgical thresholds of aortic diameter may vary based on patient`s body surface area or height.
Cases with acute type A aortic dissection, if clinically stable, should be considered for transfer to a high-volume aortic center to ameliorate survival. The intervention of type A aortic dissection should number at least an open distal anastomosis rather than just a simple supracoronary interposition graft. For the operation of uncomplicated type B aortic analysis, there is an important role for thoracic endovascular aortic repair. Clinical trials of repair of thoraco-abdominal aortic aneurysms with endografts are reporting results that suggest an endovascular repair is a viable option for cases with suitable anatomy.
Peer-review: Internal
Conflicts of interest: None to declare
Authorship: F.M.O., G.F., L.O., and G.F. equally contributed to the study and manuscript preparation.
Acknowledgement and funding: None to declare
References
1. Isselbacher EM, Preventza O, Black JH 3rd, Augoustides JG, Beck AW, Bolen MA, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022; 146: e334-e482. doi: 10.1016/j.jacc.2022.08.004 https://doi.org/10.1016/j.jacc.2022.08.004 PMid:36334952 2. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010; 121: e266-369. doi: 10.1161/CIR.0b013e3181d4739e. https://doi.org/10.1161/CIR.0b013e3181d4739e PMid:20233780 3. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM GUIDELINES FOR THE DIAGNOSIS AND MANAGEMENT OF PATIENTS WITH THORACIC AORTIC DISEASE REPRESENTATIVE MEMBERS*; Hiratzka LF, Creager MA, Isselbacher EM, Svensson LG; 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease Representative Members*; Nishimura RA, Bonow RO, Guyton RA, Sundt TM 3rd; ACC/AHA TASK FORCE MEMBERS; Halperin JL, Levine GN, Anderson JL, Albert NM, Al-Khatib SM, Birtcher KK, et al.. Surgery for aortic dilatation in patients with bicuspid aortic valves: A Statement of Clarification From the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2016; 133: 680-6. doi: 10.1161/CIR.0000000000000331 https://doi.org/10.1161/CIR.0000000000000331 PMid:26637530 4. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al.. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021; 143: e35-e71. doi: 10.1161/CIR.0000000000000932 https://doi.org/10.1161/CIR.0000000000000932 5. Riambau V, Böckler D, Brunkwall J, Cao P, Chiesa R, Coppi G, et al. Editor's Choice - Management of Descending Thoracic Aorta Diseases: Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2017; 53: 4-52. doi: 10.1016/j.ejvs.2016.06.005 https://doi.org/10.1016/j.ejvs.2016.06.005 PMid:28081802 6. Czerny M, Schmidli J, Adler S, van den Berg JC, Bertoglio L, Carrel T, et al. Editor's Choice - Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: An Expert Consensus Document of the European Association for Cardio-Thoracic Surgery (EACTS) & the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2019; 57: 165-98. doi: 10.1016/j.ejvs.2018.09.016 https://doi.org/10.1016/j.ejvs.2018.09.016 PMid:30318395 Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.Archive of Issues
AUTHOR'S CORNER
 Authors having problems with submissions please notify editor: editor@hvt-journal.com
Authors having problems with submissions please notify editor: editor@hvt-journal.com
