Heart valve disease gender difference in the era of transcatheter treatment
REVIEW
Heart valve disease gender difference in the era of transcatheter treatment
Article Summary
- DOI: 10.24969/hvt.2023.375
- CARDIOVASCULAR DISEASES
- Published: 18/02/2023
- Received: 17/12/2022
- Revised: 06/02/2023
- Accepted: 08/02/2023
- Views: 7595
- Downloads: 4484
- Keywords: gender, heart valve, transcatheter treatment, aortic valve, mitral valve, tricuspid valve
Address for Correspondence: Cristina Aurigemma, Institute of Cardiology Fondazione Policlinico Universitario A. Gemelli IRCCS Università Cattolica del Sacro Cuore, L.go A. Gemelli 1, 00168 Rome, Italy
Fax: + 39-06-3055535 Phone: +39-06-30154187 Email: aurigemma.cristina@gmail.com
Cristina Aurigemma1, Francesco Burzotta1,2, Carlo Trani1,2
1Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
2Universita Cattolica del Sacro Cuore, Rome, Italy
Abstract
Available data have demonstrated important sex-related differences in patients with valvular heart disease, regarding clinical presentation, treatment, and outcomes. Although the calcific aortic stenosis (AS) is more frequent in men compared to women, the majority of AS patients over 80 years old are women, in whom fibrotic remodeling of aortic valve is typically found. Mitral valve disease is more common in women. However females are under-referred or delayed referrals to treatment, probably due to the absence of sex-based LV dimension values guiding surgical timing. The development of transcatheter devices have revolutionized the treatment of valvular heart disease and increased the interest in this topic.
In this context, the consideration of gender differences in presentation, diagnosis, treatment success, and prognosis is of great importance.
Key words: gender, heart valve, transcatheter treatment, aortic valve, mitral valve, tricuspid valve
Introduction
The majority of valve heart disease (VHD) is diagnosed in patients greater than 65 years old, indeed the incidence of VHD increases with age. VHD may equally affect men and women, but sex specific differences in prevalence of valve disease type are described in literature (1-3). Furthermore available data have demonstrated a different risk profiles in women and men affected by heart valve disease, with a significant impact on treatment outcomes and prognosis (4-5). Recently the development of transcatheter devices offers new treatment options for VHD. In this context, although women have been historically underrepresented in most trials investigating transcatheter treatment, the consideration of gender differences in treatment success, and prognosis is of great importance.
This review is an overview of gender-related differences in patients with VHD, regarding incidence, clinical presentation, treatment, and outcomes in the era of transcatheter treatment.
Aortic valve disease
In developed countries, the more common treated VHD is the aortic valve, with the majority of aortic valve disease represented by aortic stenosis. In these countries calcific degeneration of tricuspid aortic valve represents the more common mechanism of aortic stenosis.
In women aortic valve calcium, even after indexing to body surface area or aortic annulus area, is lower compared to men (6-8). Sex-specific hormonal differences are proposed as possible explanation of more calcified aortic valve stenosis in men, in particular testosterone may be involved in greater calcific deposition in the aortic sinus (9). Instead valvular fibrosis is involved in women with hemodynamically severe aortic stenosis, in which a lower degree of aortic valve calcification is typically found (10).
The intramyocardial fibrosis is also more frequent in women compared to men (Fig. 1).
Some gender differences are also found in clinical presentation of aortic stenosis. In particular at presentation, women are older and have worse symptom burden, including more exercise dizziness and more advanced New York Heart Association class (11) (Fig. 1).
The aortic regurgitation has more marked sex differences than aortic stenosis and is more common among men (12), probably due to the higher incidence of bicuspid aortic valve in male (male- female sex ratio 2:1) (13) and endocarditis (14) (Fig. 1). Similarly to aortic stenosis, a trend of greater symptomatology has also been found in women with aortic regurgitation compared to men (15) (Fig. 1).
Echocardiographic assessment based on sex specific criteria (stroke volume index, size specific left ventricular dimensions and aortic regurgitation) should be considered in order to avoid an underestimation of the severity of valve disease and undertreatment of female patients (Fig. 1).
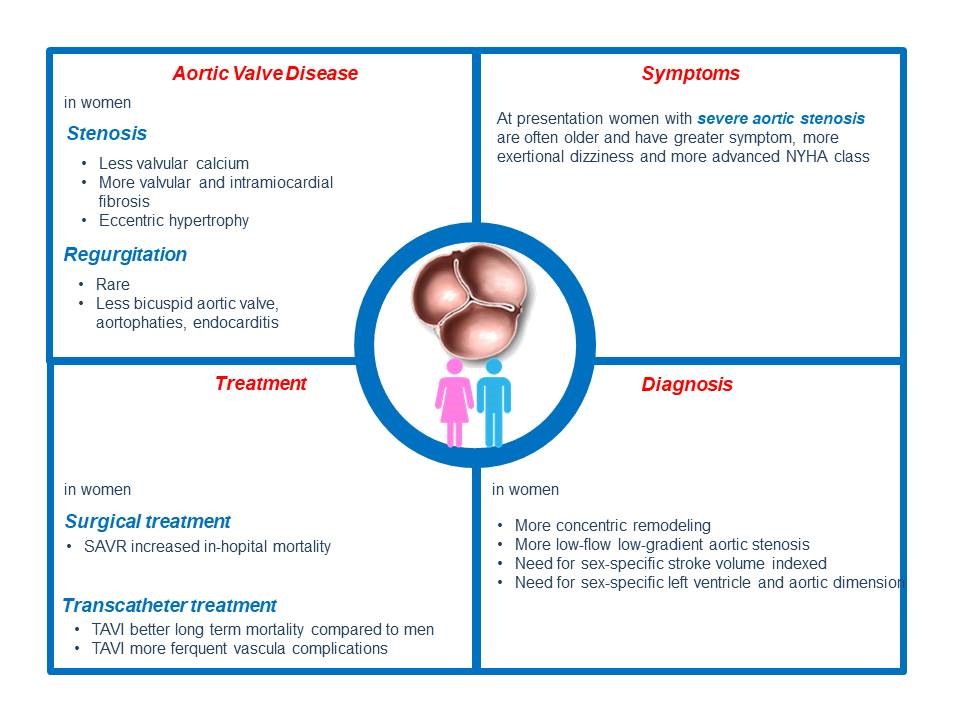
Figure 1. Gender differences in aortic valve disease. Gender-related differences in aortic valve disease regarding incidence, clinical presentation, treatment, and outcomes
SAVR - surgical aortic valve replacement; TAVI - transcatheter aortic valve implantation
Furthermore the fibrotic remodeling of the aortic valve typically of aortic stenosis in women highlights the importance of sex-specific thresholds of aortic valve calcification by cardiac imaging. Historically the gold standard treatment of aortic stenosis was surgical aortic valve replacement (SAVR).
In the past decade the clinical outcomes of SAVR have improved significantly, but conflicting results on differential sex impact on outcomes are reported by several studies. Data from Nationwide Inpatient Sample, including 166.809 patients (63% male and 37% female) underwent SAVR between 2003 and 2014 have demonstrated a worse in-hospital mortality following SAVR in women compared to men (5.6% versus 4%, p<0.001). After propensity matching, in-hospital mortality remained significantly higher in women than in men (3.3% versus 2.9%, p=0.001) (16).
The introduction and widespread adoption of transcatheter aortic valve implantation (TAVI) have revolutionized the treatment of aortic stenosis. The clinical outcomes of the 353 women enrolled in the CoreValve US High Risk Pivotal Trial have demonstrated a lower 1-year cardiovascular mortality and a lower 1-year all-cause mortality or major stroke in women undergoing TAVI compared with women undergoing SAVR. Furthermore, as expected, the mean gradient was lower (8.92 (4.17) mmHg vs 12.24 (5.39) mm Hg; p <0.001) and the effective orifice area (EOA) was greater (1.80 (0.53) cm2 vs 1.44 (0.47) cm2; p <0.001) in TAVI compared with SAVR. The rate of prosthesis-patient mismatch was lower in female TAVI versus SAVR at 30 days (8.8% vs 29.3%), 6 months (8.1% vs 24.5%), and 1 year (6.9% vs 29.8%) (17).
Several studies have reported superior outcomes with TAVI in women compared to men, partially due to longer life expectancy in women. In SAPIEN 3 Aortic Bioprosthesis European Outcome (SOURCE 3) registry all-cause mortality trended lower in women than men at 4 years post TAVI (18).
An analysis of a contemporary cohort of patients treated with balloon-expandable and self-expandable transcatheter valves found similar rates of in-hospital mortality, stroke, moderate/severe paravalvular leak and pacemaker implantation in women and men (19). Data from Transcatheter Valve Therapy (TVT) registry of the STS/American College of Cardiology (ACC), including 11.808 (49.9%) women and 11.844 (51.1%) men underwent TAVI from 2011-2014 have demonstrated a different risk profile between woman and men and 1-year adjusted survival was superior in female patients, notwithstanding a greater adjusted risk for in-hospital vascular complications (20). Indeed, in TAVI procedure major vascular complications are experienced more frequent in women, probably related to low body surface area and smaller peripheral vessels (21). In WIN TAVI (Women’s International Transcatheter Aortic Valve Implantation), an international, multicenter, prospective observational registry of 1019 female patients undergoing TAVI, the Valve Academic Research Consortium 2 (VARC-2) early safety end point (composite of mortality, stroke, major vascular complications, life-threatening bleeding, stage 2 or 3 acute kidney injury, coronary artery obstruction, or repeat procedure for valve-related dysfunction) is reported in 14% and it is manly driven by vascular complications (7.7%) (22) (Fig. 1).
Further information will come from the ongoing Randomized Research in Women All Comers With Aortic Stenosis (RHEIA) trial, a prospective, randomized multicenter study that tests non inferiority and, eventually, the superiority of TAVI versus surgical aortic valve replacement in women with severe aortic stenosis (NCT04160130) (23).
Mitral valve disease
Mitral valve disease represents a quarter of valve heart disease in the developed countries, with mitral regurgitation more common than mitral stenosis. Globally the most common valve disease is the mitral regurgitation, which affected 1-2% of world’s population. Rheumatic and non-rheumatic degenerative mitral valve disease is also more common in women compared to men (24). Furthermore women are predisposed to bileaflet mitral valve prolapse, due to more myxomatous valve related to sex-based differences in extracellular matrix remodeling. The posterior mitral valve prolapse with flail is more common in men. Due to these valve morphology differences women with mitral valve prolapse have less frequently severe mitral valve regurgitation (25). Conversely, secondary mitral regurgitation, as a consequence of myocardial infarction or coronary artery disease, occurred more frequent in women compared to men (26).
Gender difference have also been reported in the pathophysiology of mitral apparatus calcification, with posterior leaflet calcification more common in men and mitral annular calcification in women (27) (Fig. 2). Available data have demonstrated gender difference in clinical presentation of mitral valve disease. Postcapillary pulmonary hypertension as expression of adverse pulmonary vascular remodeling is more common in women affected by mitral stenosis (28). Although less dilated ventricles and less severe mitral regurgitation worse heart failure symptoms are more common in women with mitral regurgitation (29) (Fig. 2).
The assessment of the mitral valve anatomy, function and mechanism of abnormalities are performed by echocardiography. Sex and sizes specific parameters should be considered to evaluate left ventricle dilation in the setting of mitral regurgitation. Transesophageal echocardiography is used in pre-procedure assessment and guidance of percutaneous procedures including both repair and replacement (Fig.2).
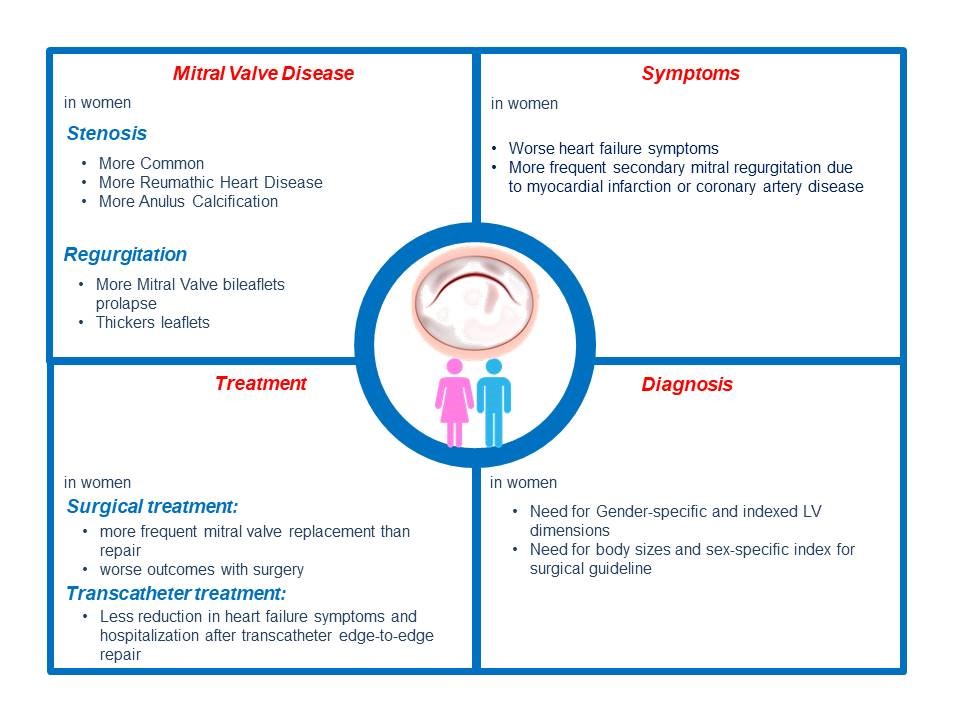
Figure 2. Gender differences in mitral valve disease. Gender-related differences in mitral valve disease regarding incidence, clinical presentation, treatment, and outcomes
Although mitral valve (MV) disease is more common in women compared to men, women are referred for mitral valve intervention at fewer rates and later in the disease course (30). The delayed referral, probably due to cut-off values based primarily on a predominantly male population without sex-based differences, partially explains the worse clinical outcomes after mitral surgery in women (31).
Furthermore in women undergoing surgery for primary or degenerative mitral regurgitation, mitral repair was less performed. Indeed in women MV replacement is performed more frequently compared to men (32). Since MV repair is preferred to replacement for early and late better clinical survival (33), the mortality after MV surgery is higher in women compared to men (32). These differences in intervention and outcomes may be related to frailty, differences in the prevalence and severity of secondary mitral regurgitation, rheumatic valve disease, and mitral annular calcification. Indeed in a propensity score-matched analysis of 846 patients the surgical approaches for men and women were similar and mortality was comparable (34). These results underlines that the clinical outcomes are dependent upon the later referral, the severity of the mitral disease and associated co-morbidities at the time of surgery (Figure 2).
Rheumatic mitral stenosis is more frequent in women, and data on outcomes after percutaneous balloon mitral valvuloplasty are mixed and it is unclear if there are sex-based differences in outcomes after balloon valvuloplasty (35).
The incident mitral annulus calcification is more frequent in women, therefore in Mitral Annulus Calcification Global Registry 68% of patients were women (36).
Data on percutaneous valve replacement in mitral annulus calcification have demonstrated a worse clinical outcome compared to valve-in-valve and valve-in-ring procedures (37). After transcatheter edge-to-edge repair (TEER) reverse left ventricle remodeling is revealed more frequent in female gender (38).
Nonetheless, the clinical improvements in women treated with TEER seem to be no better compared to men. Indeed studies investigated sex difference in clinical outcomes after TEER have reported contrasting results. The Transcatheter Mitral Valve Interventions (TRAMI) registry (39) and the Getting Reduction of Mitral Insufficiency by Percutaneous Clip Implantation in Italy (GRASP) registry (40) have reported less improvement in New York Heart Association Class in women compared to men, while the European Registry of Transcatheter Repair for Secondary Mitral Regurgitation (EuroSMR) study have shown equivalent quality of life and symptomatic improvements in both women and men (41).
Women represented only 36% of patients in Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) trial (42) and only 25% of patients in the Percutaneous Repair With the MitraClip Device for Severe Functional/Secondary Mitral Regurgitation (MITRA-FR trial) trial (43); this underrepresentation raises questions about the applicability of results to women. In a sex- specific outcomes subanalysis of the COAPT TEER resulted in improved clinical outcomes compared with guideline-directed medical therapy alone, irrespective of sex. However, the reduction in heart failure hospitalizations was less pronounced in women compared to men beyond the first year after treatment (44). Instead data from the Society of Thoracic Surgery/ACC Transcatheter Valve Therapy registry (5.295 patients, 47.6% women enrolled from 2011 to 2017), have demonstrated sex differences in outcomes after TEER, with female sex associated with lower adjusted 1-year risk of all- cause mortality (45). Similarly a meta-analysis of eleven studies with a total of 24.905 patients (45.6% women) have reported that female sex is associated to lower adjusted mortality on long-term follow-up (46).
Further studies are need to confirm sex differences in outcomes after transcatheter edge-to-edge repair (Fig. 2).
Tricuspid valve
According to etiology and mechanism, tricuspid regurgitation (TR) is classified in primary and secondary (47). Primary TR is less common and it is due to congenital and genetic anomalies (Ebstein’s anomaly, tricuspid dysplasia, and myxomatous degeneration leading to tricuspid valve prolapse) or due to acquired valve disease (endocarditis, carcinoid, rheumatic involvement). In primary TR the dominant mechanism is tricuspid leaflet abnormalities with variable leaflets mobility and dilatation of tricuspid annulus, right ventricle and right atrium.
Secondary TR represents 90% of all TR and it is characterized by normal valve leaflets with incomplete leaflet coaptation. There are two types of secondary TR: atrial and ventricular. Atrial TR is due to atrial fibrillation/flutter or heart failure with preserved ejection fraction. In atrial TR the dominant mechanism is marked tricuspid valve annulus dilatation; right atrium is also dilated, while leaflets mobility and right ventricle volume are typically normal. Ventricular TR is related to left-sided ventricular or valve disease, pulmonary hypertension, right ventricular cardiomyopathy or infarction. In ventricular regurgitation the dominant mechanism is marked leaflet tethering, with leaflet mobility reduction in systole and dilatation of right annulus, right ventricle and right atrium.
The Framingham Heart Study (48) and other community-based cross sectional studies (49) have demonstrated a female preponderance for mild or severe TR dominance with a male-to-female ratio of 1 to 1.6. Post mortem studies have revealed sex-differences in annular anatomy, with more elastic, more cellular and smaller when correcting for heart weight right atrioventricular annuli in men compared to women (50) (Fig. 3). Consequently, triggers such as atrial fibrillation may cause more frequently annular dilation and secondary TR in women. The progression from moderate to severe TR is also more rapid in women compared to men (51). Furthermore women with secondary TR are older and more symptomatic than men (52) (Fig. 3).
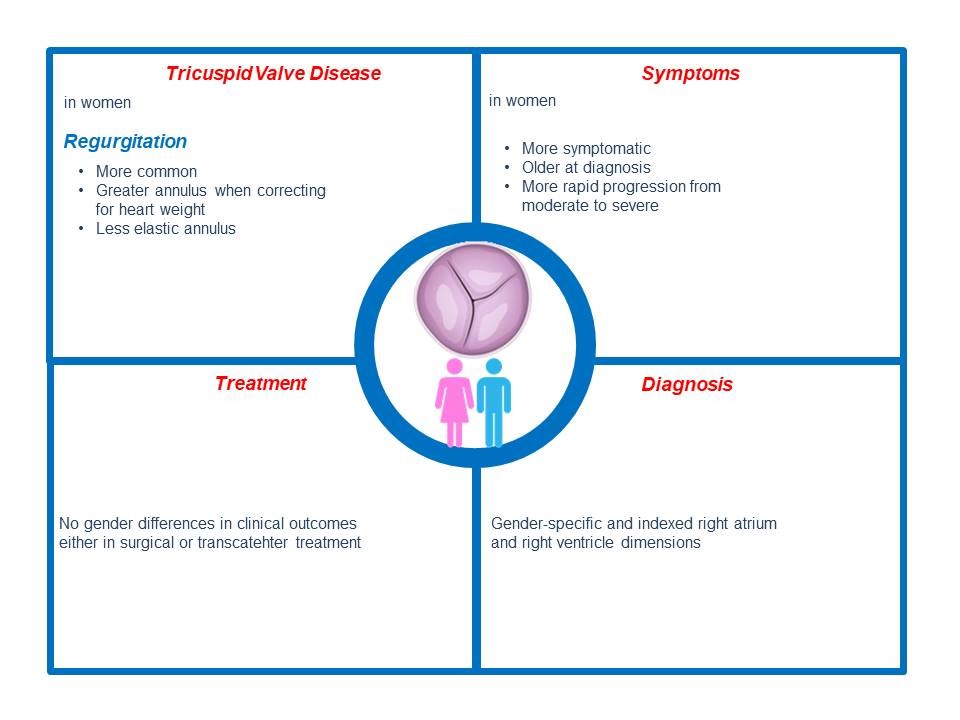
Figure 3. Gender differences in tricuspid valve disease. Gender-related differences in tricuspid valve disease regarding incidence, clinical presentation, treatment, and outcomes
Surgical intervention for isolated TR is a rare intervention with higher in-hospital mortality (8.8%), repair is associated to better clinical outcome compared to replacement (53). In the analysis of data from the National Inpatient Sample women represent the majority of patients undergoing tricuspid surgery and no gender difference is identified in clinical outcomes (54).
Recently different percutaneous treatments for tricuspid regurgitation are proposed. Multiple technologies for transcatheter tricuspid valve repair are available, including coaptation or annuloplasty devices. Data of safety and feasibility trials on these devices reported promising results (55, 56).
Other current transcatheter treatment options include heterotopic caval valve implantation and not yet commercially available transcatheter tricuspid valve replacement with orthotopic valve implantation. The Transcatheter Tricuspid Valve Therapies (TriValve) registry have enrolled patients with severe tricuspid regurgitation undergoing transcatheter tricuspid valve intervention (percutaneous edge-to-edge, annuloplasty, tricuspid replacement) from 2016 to 2021 in 24 centers (57). Data from this registry have demonstrated no difference between men and women in survival, heart failure hospitalization, functional status, and tricuspid regurgitation reduction up to 1 year, but transcatheter tricuspid valve intervention is associated by survival benefit compared to medical therapy alone in both women and men (Fig. 3).
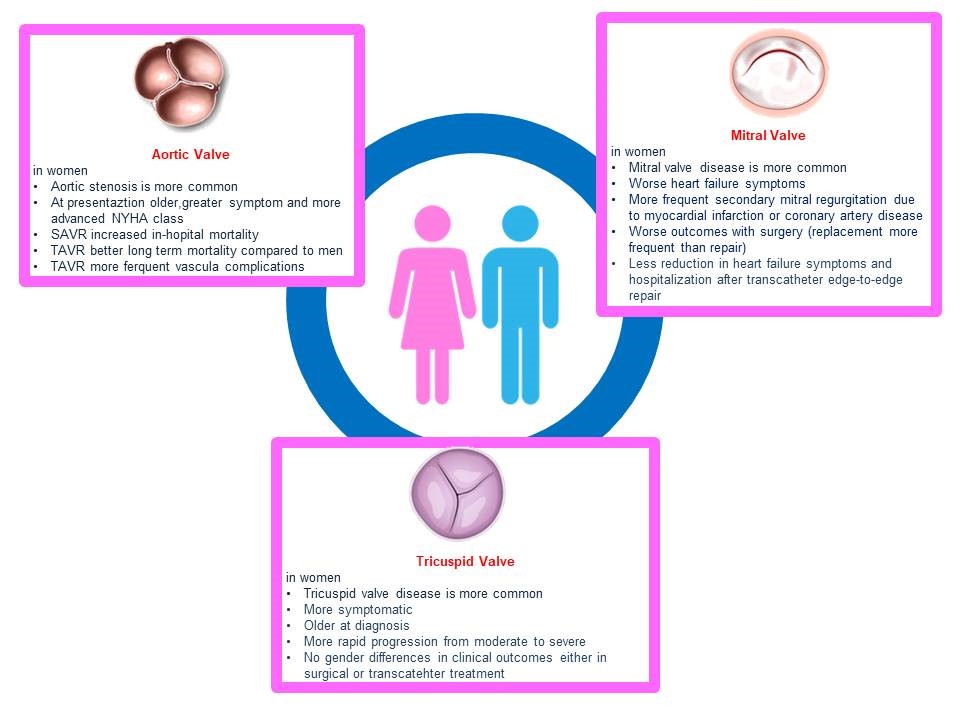
Figure 4. Gender-related differences in heart valve disease
Conclusions
VHD increases significantly among aging populations and important sex-related differences in clinical presentation, treatment, and outcomes are revealed by several studies. A specific risk profile is identified in females with consequently unique challenges for the invasive treatment of the diseased valve (Fig. 4). Implementation of sex-specific treatment criteria should be encouraged in order to guarantee timely referral to treatment.
Future research studies on sex-related differences are need for a tailored management with respect to the timing of intervention and treatment modality to benefit both sexes.
Peer-review: External and internal
Conflicts of interest: None to declare
Authors’ disclosures: Cristina Aurigemma has been involved in advisory board activities by Abbott, Abiomed, Medtronic and Daiichi Sankyo. Francesco Burzotta discloses to have been involved in advisory board meetings or having received speaker’s fees from Abbott, Abiomed, Medtronic and Biotronic. Carlo Trani discloses to have been involved in advisory board meetings or having received speaker’s fees from Abbott, Abiomed, Medtronic and Biotronic.
No fee was received for this work.
Authorship: C.A., F.B., and C.T. equally contributed to the study and manuscript preparation.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

