Quiz - Congenital heart diseases
QUIZ
Quiz - Congenital heart diseases
Article Summary
- DOI: 10.24969/hvt.2023.380
- Cardiac Surgery
- Published: 13/03/2023
- Received: 09/02/2023
- Accepted: 10/02/2023
- Views: 13789
- Downloads: 4716
- Keywords: quiz
Address for Correspondence: Kuat Abzaliev, Department of Clinical Disciplines, Al-Farabi Kazakh National University, Almaty Kazakhstan
Email: kuat_abzaliev@mail.ru
Quiz - Congenital heart diseases
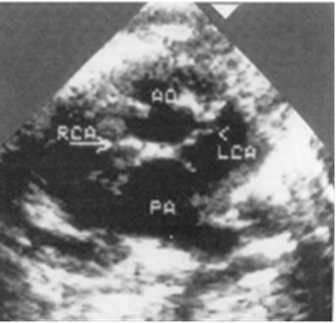
Case 1. Echocardiography (EchoCG) revealed a secondary atrial septal defect (ASD) of 0.79 cm in a newborn infant. Right-to-left shunt. Dilation of right atrium (RA) and right ventricle (RV). Paradoxical movement of interventricular septum (IVST). The left ventricle is compressed by the right ventricle. Common pulmonary venous chamber (CPVC) is visualized (Fig.1), pulmonary artery (PA) trunk dilatation. The shape of the flow in the PA indicates high pulmonary hypertension.
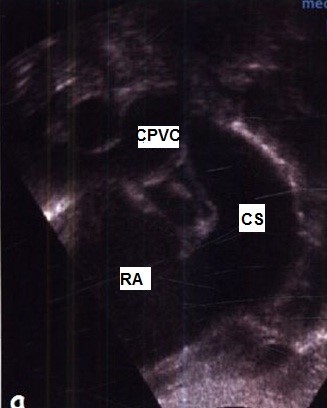
CPVC – common pulmonary venous chamber, CS – coronary sinus, RA- right atrium
Question: What diagnosis would you suggest for this child?
a) ASD
b) Total anomalous pulmonary veins drainage
c) Ebstein's anomaly
d) Transposition of the great vessels
e) Taussig-Bing's anomaly.
(Correct answer - b)
Case 2: A 3-month-old child has shortness of breath and perioral cyanosis when restless, decreased appetite, poor weight gain, sweating. The child's condition is relatively satisfactory. The skin is pale. Above the lungs, wheezing. The pulse rate is 140 per minute. The boundaries of the heart are dilated to the left. On auscultation, a systolic murmur is heard, with its epicenter in the IV intercostal space to the left of the sternum, the II tone over the PA is accentuated.

(Reproduced form https://cf2-online.org under CC BY license)
Question: What is the most likely diagnosis, and what should be the done?
a) Fallot tetralogy. It is necessary to make EchoCG, prescribe b-blocker and prepare for surgery.
b) ASD. Perform EchoCG to confirm the diagnosis. Prescribe enalapril, spironolactone, digoxin at pre-hospital stage and schedule surgical treatment.
c) Transposition of the great vessels. It is necessary to perform multislice computed tomography (MSCT) with contrast, catheterization of the right heart. Prepare for surgery.
d) Total anomalous pulmonary veins drainage. Perform EchoCG and right heart catheterization to confirm the diagnosis. Prepare for surgery.
(Correct answer )
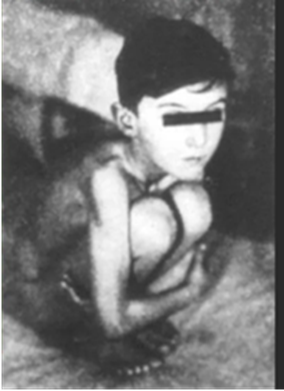
Case 3. The child is 1 year, 7 months old; on exertion he developed an attack of dyspnea, tachycardia, and cyanosis appeared. At first, the child was observed to be agitated, and then he adopted a lap and elbow position (Fig. 3). Examination of the child reveals signs of congenital heart defect - enlargement of heart borders, coarse systolic murmur conducted to all points, "dry" and airy lungs.

(Adapted from https://гкб2.рф/wp-content/uploads/2022/01/c61eef0d7dbe606d13e2bf45e0843a24.jpg in frame of CC-BY license)
Question: Which defect is characterized by these symptoms?
a) Transposition of the great arteries
b) Total anomalous pulmonary veins drainage infracardiac form
c) Tetralogy of Fallot
d) Ebstein's anomaly
e) Taussig-Bing syndrome
(Correct answer - c)
Case 4. During a preventive examination of children, you found in a child of 7 years old a systolic murmur on the left edge of the sternum with the epicenter in the 2nd-3rd intercostal space. On collecting the anamnesis, there were no complaints, the parents said that there was a murmur at birth, but they did not apply anywhere and did not conduct examinations, because the child is active. You took an X-ray.

(Adopted from https://s0.slide-share.ru/s_slide/6aa6134c91df3cc1af1e4d4ded3f95f8/6ecb46b7-1d32-4006-a24a-5ec01df552f8.jpeg in frame of CC-BY license)
Question: What kind of congenital heart defect can a child have?
a) Patent foramen ovale
b) Atrial septal defect
c) Pulmonary artery stenosis
d) Ventricular septal defect
(Correct answer – c)
Case 5. Patient E., 8 months old was admitted to the cardiac intensive care unit in severe condition. Severe dyspnea, tachycardia, cardiomegaly, hepatomegaly, edema, cyanosis are noted. After stabilization and further examination the diagnosis of corrected transposition of the great vessels combined with ASD was made.
(Adapted from https://miro.medium.com/max/2000/1*crOwH6YXckx0DTAQY-rDcg.jpeg under CC-BY license)
Question: What needs to be found out to decide on the surgical tactics for treating the patient?
a) Size of the atrial septal defect
b)Pulmonary artery pressure
c)Diameter of the aorta and pulmonary artery
d) Anatomical location of the left ventricle).
Case 6. Your fellow radiologist comes running to you with a picture of a 5-year-old child. He cannot
understand why the image turned out that way and cannot describe it.

(Adapted from https://thepresentation.ru/img/tmb/1/88659/0739829692088d23570f7f4a8e6b5c62-800x.jpg under CC-BY license)
Question: What are the causes of the formation of the upper shadow, which resembles a snow moth, and the method of diagnosing this pathology?
a) Enlarged thymus, computed tomography
b). Anterior mediastinal tumor, mediastinal ultrasound
c)Pulmonary veins drained into the EPO, EchoCG and angiography
d) Superior vena cava syndrome, MSCT with contrast.
(Correct answer - c)
Case 7. A newborn diagnosed with CHD. Transposition of great vessels, patent foramen ovale, and open arterial duct. Saturation 55-65%.
Adapted from https://images.slideplayer.com/36/10584201/slides/slide_7.jpg under CCY-BY license)
Question: What actions should be taken to stabilize the patient by looking at the chart?
a)Do not relax the patient, ventilate with FiO2 50%, give intravenous infusion of prostaglandin E1 for 12 h at a dose of 0.1-0.6 ng/kg body weight per min, perform the Rushkind procedure
b) Perform relaxation, sedation, ventilation with FiO2 21%, prostaglandin E1 titration to maintain an open arterial duct, perform the Rushkind procedure to increase blood mixing.
c)Perform occluder placement in the open arterial duct and foramen ovale, perform intravenous infusion of prostaglandin E1 for 12 h at a dose of 0.1-0.6 mg/kg body weight per min, and perform relaxation, sedation, ventilation with FiO2 21%.
d)Perform relaxation, sedation, ventilation with FiO2 21%, prostaglandin E1 titration and Rushkind procedure, and open arterial duct stenting
(Correct answer -)
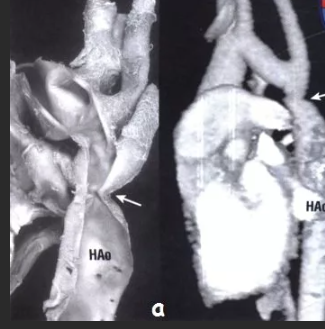
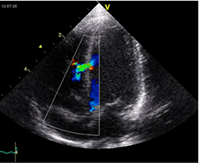
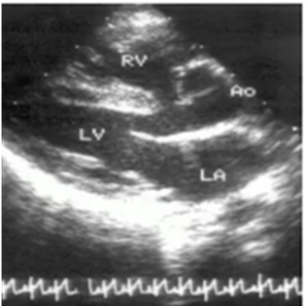
Case 8. From the ultrasound room, the nurse brought an ultrasound picture of a 3-month-old baby's malformation for your consultation.
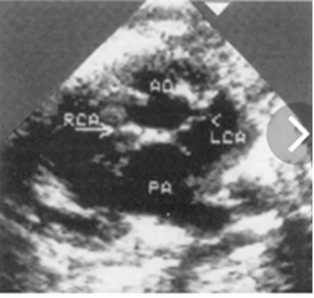
Adapted from https://thepresentation.ru/img/tmb/4/349645/528d1313f180ee842d5db16d7e6935b7-800x.jpg under CC-BY license)

(Adopted from https://present5.com/presentation/105348610_455380574/image-21.jpg under CC-BY license)
Question: What diagnosis would you suspect?
a) Total abnormal pulmonary vein drainage
b) Double branching of vessels from the right ventricle
c) Corrected transposition of the great vessels
d) Fallot's pentalogy
e) Uncorrected transposition of the great vessels
(Correct answer - e)
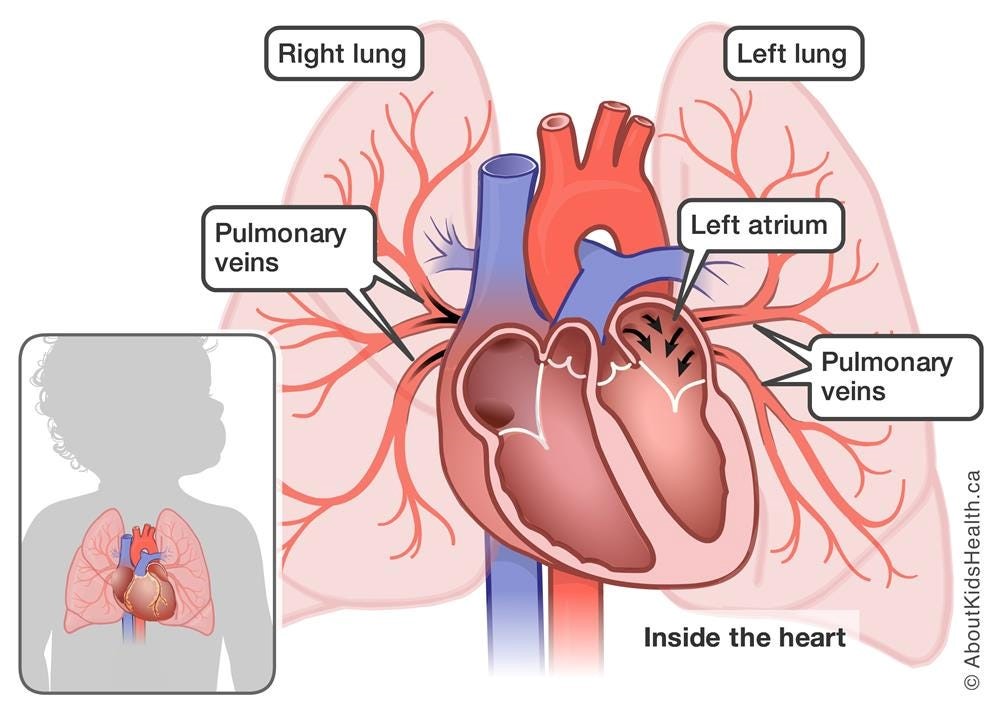
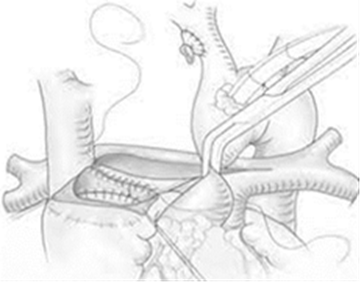
Case 9. EchoCG revealed a secondary atrial septal defect (ASD) of 0.79 cm in a newborn infant. Right-to-left shunt. Dilation of right atrium (RA) and right ventricle (RV). Paradoxical movement of interventricular septum (IVST). The left ventricle is compressed by the right ventricle. Common pulmonary venous chamber (CPVC) is visualized, pulmonary artery (PA) trunk dilatation. The shape of the flow in the PA indicates high pulmonary hypertension.
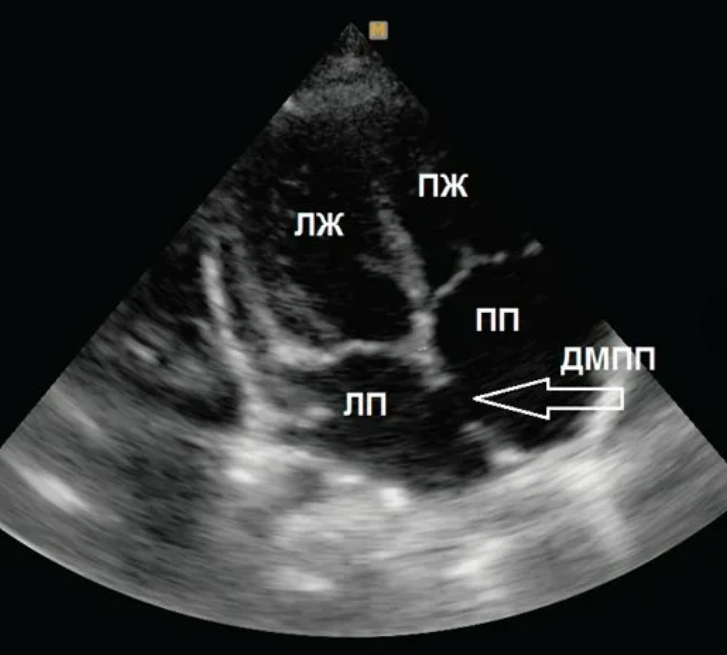
(Adapted from https://www.medison.ru/si/n29/s429/p1b.jpg under CC-BY license)
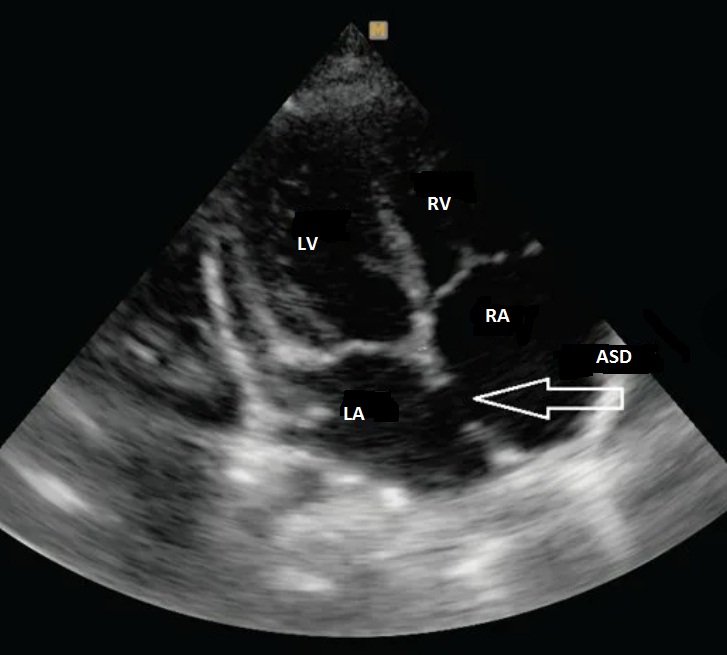
(Adapted from https://cf2.ppt-online.org/files2/slide/a/aWwROjy64E2LI7QBNGiz9d3A58cKFZvhS0Memqnks/slide-19.jpg under CC-BY license)
Question: Which of the additional methods of examination will not help you to verify the diagnosis?
a) To confirm the diagnosis and clarify the anatomical form of the defect, a transesophageal EchoCG should be performed
b) To confirm the diagnosis and clarify the anatomic form of the malformation, contrast MSCT-angiocardiography should be performed
c).+ To confirm the diagnosis and clarify the anatomical form of the defect, you should perform a right heart catheterization with angiography
d) To confirm the diagnosis and clarify the anatomic form of the malformation, catheterization of the left heart with angiography should be performed
(Correct answer -c)
Case 10. A 9-year-old child. He complains of frequent headaches, tinnitus, nasal bleeding, poor memory, pain in the lower extremities when walking fast. Examination draws attention to body disproportion - athletic torso, well-developed shoulder girdle musculature. There is a difference in BP in the arms and legs. At the same time, the blood pressure in the arms was 155/90 mm Hg.
(Adapted from https://dommedika.com/cardiology/Pic/koarktacia_aorti.jpg under CC-BY license)
Question: Which research method would be uninformative for making a diagnosis in this situation? a) Cardiac ultrasound
b)Chest X-ray review
c)Electrocardiography
d) MSCT angiography
(Correct answer -c)
Case 11. The child is 8.5 years old, complains on frequent headaches, tinnitus, nosebleeds, poor memory, pain in the lower extremities when walking fast. Examination reveals physique disproportion - athletic torso, well-developed shoulder girdle musculature). At the same time, the blood pressure in the hands is 150/90 mmHg.

(Adapted from http://www.mif-ua.com/media/uploads/arhiv/zr/2015/1(60)/131/131.jpg under CC-BY license)
Question: What treatment plan would you suggest? a) X-ray endovascular implantation of a stent graft is indicated
b) Surgical correction of the defect is indicated
c) Prepare for embolization of the adrenal vessels
d) Exempt from physical education and sports
(Correct answer - b)
Case 12. According to the mother, at your consultation, the child (2 years old, 13 kg) is active, does not have any complaints. General condition is satisfactory. Hemodynamics is stable, blood pressure - 100/70 mmHg, pulse 102 per minute. EchoCG revealed a 3 mm trabecular septal defect. Interventricular gradient LV/RV -88 mmHg, PA systolic pressure 20 mmHg.
(Adapted from https://upload.wikimedia.org/wikipedia/commons/thumb/7/79/Ventricular_Septal_Defect.jpg/1280px-Ventricular_Septal_Defect.jpg under CC-BY license)
Question: What is the further tactic of management of this patient?
a).Planned ASD occluder implantation
b) Refer the patient to a cardiac surgeon for urgent surgical treatment to perform valvular fibrillation repair.
?) Continue dynamic observation. Surgical treatment is not indicated. There is a possibility of spontaneous closure of the defect.
d) Prescribe drugs to stimulate independent closure of the defect, prescribe prostaglandin E, spironolactone.
(Correct answer - a)
Case 13. A 6-year-old child has: delayed physical development, fainting attacks, choking, pale skin, dilated heart borders, II tone accent over the pulmonary artery, systolic-diastolic ("machine") murmur over the whole heart area, chest X-ray: increased pulmonary pattern, cardiomegaly, protrusion of the pulmonary artery arch.

(Adapted from http://images.myshared.ru/9/686666/slide_27.jpg under CC-by license)
Question: What is the diagnosis and what kind of examination is necessary to clarify the diagnosis and determine further management tactics?
a) ASD. It is necessary to perform EchoCG, catheterization of the right heart to measure the pressure in the heart chambers and decide whether to place an occluder
b) Patent ductus arteriosus. EchoCG, heart catheterization for invasive monitoring of pressure in the heart cavities and main vessels and determination of indications for surgery should be performed.
c) Ventricular septal defect. Perform EchoCG, cardiac MSCT with contrast and ECG
d) Pulmonary artery stenosis. Perform chest X-ray, pulmonary angiography, and cardiac chambers` pressure measurement
(Correct answer - b)
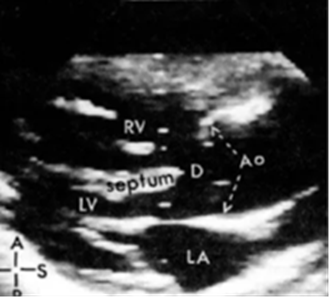
Case 14. From the ultrasound room we brought a description (report) and a photo of the child's defect for your consultation.
(Adapted from https://thepresentation.ru/img/tmb/4/349645/528d1313f180ee842d5db16d7e6935b7-800x.jpg under CC-BY license)
Question: What EchoCG signs do you see on the image?
a)The aorta is displaced to the right. The pulmonary artery is poorly visualized. The main vessels and ventricular outflow tracts are crossed (output simultaneously without rotation of the transducer); the right semilunar valves are at a low level;
b)The aorta takes off from the RV, the pulmonary artery from the LV; the trunk vessels and ventricular outflow tracts are parallel (they exit simultaneously without probe rotation); the semilunar valves are at the same level; mitral-pulmonary fibrous extension
c)The aorta is displaced to the right and is over the ASD ("Rider"). The pulmonary artery is poststenotically dilated to 3 cm. The main vessels are located normally. The semilunar valves on both are located at the normal level;
d) The pulmonary artery is displaced to the left, the aorta to the right. There is a VSD under the septal leaflet of the tricuspid valve
(Correct answer - b)
Case 15. Name the main stages and terms of hemodynamic correction of univentricular heart defects
a) Stage 1 -modified Blalock-Taussig shunt or PA banding during neonatal period
b) Stage 2 of the Glenn bidirectional cardiopulmonary anastomosis 6-12 months of age
c) Stage 3 Fontaine surgery between 1.5 and 5 years of age
d) Stage 4 Conducting the Rushkind procedure with a possible Maze III procedure.
Possible variations: a) 1-2 b) 2-4 c) 2-3 d) 1-3
(Correct answer -)
Case 16. A 11-year-old girl L. was admitted to the hospital with complaints of dyspnea and cyanosis, which increased with physical exertion. The anamnesis shows that the first heart murmur was heard in the maternity hospital. After 6 months of life, cyanotic coloring of skin and mucous membranes appeared. On examination: skin and mucous membranes with cyanotic hue. The symptom of "drumsticks" and "watch glasses". Borders of relative cardiac dullness: left - on the left midclavicular line, right - on the right parasternal line, upper - II intercostal f) Heart sounds of satisfactory volume, HR - 84 beats per minute. BP is 20 beats per minute. Intense, prolonged systolic murmur of a harsh timbre, centered in the II-III intercostal space to the left of the sternum. II tone was attenuated in the second intercostal space on the left side of the sternum. Cardiac ultrasound revealed:
(Adapted from https://thepresentation.ru/img/tmb/1/88659/1c3c727206a02a3ebcfb09cc26bdb138-800x.jpg under CC-BY license)
Question: In which disease do these syndromes and symptoms occur?
a) Transposition of the great vessels
b) Total anomalous pulmonary veins drainage - intracardiac form
c) Fallot tetralogy
d) Primary pulmonary hypertension
(Correct answer - c)
Case 17. The child is 1 year, 5 months old. On exertion (walking 60 meters) he developed an attack of dyspnea, tachycardia, and cyanosis appeared. At first, the child was observed to be agitated. Examination of the child revealed the signs of congenital heart defect - cardiac dilatation, coarse systolic murmur conducted to all points, "dry" lungs
(Adapted from https://studfile.net/html/2706/261/html_1VelhcNMEN.5lX3/htmlconvd-Ofjz_I35x1.jpg under CC-BY license)
Question: Which of the following manipulations should not be done?
a)The child is helped into a lap and elbow position (to increase systemic vascular blood flow)
b)+ Bloodletting up to 200 ml
c) Giving oxygen with a mask
d) Administer morphine im or sc 0.1-0.2 mg/kg
e) IV 4% sodium bicarbonate solution: first 200 mg/kg (5 ml/kg) slowly over 5 minutes, then repeat the same dose by dividing it into two parts. The first part is administered in the first 30 minutes. The other part is administered within one hour.
f) if cyanosis persists, administer propranolol 0, 1-0.2 mg/kg in 10 ml of 20% glucose solution(1ml/min; for convulsions, administer sodium 50 oxybutirate 100 - 150 mg/kg slowly 20 mg/kg/h
(Correct answer –b)
Case 18. A 55-year-old man was taken to the emergency room. According to his attendants, he collapsed in a grocery store and was unconscious for 1 to 2 minutes. The man was able to say that it started with a sudden heartbeat. Presented with complaints of pain behind the sternum and dizziness. Past medical history: arterial hypertension, type 2 diabetes mellitus. Currently receiving outpatient treatment for pneumonia and taking the following medications; lisinopril, metformin and azithromycin. On examination, there were no signs of any trauma.
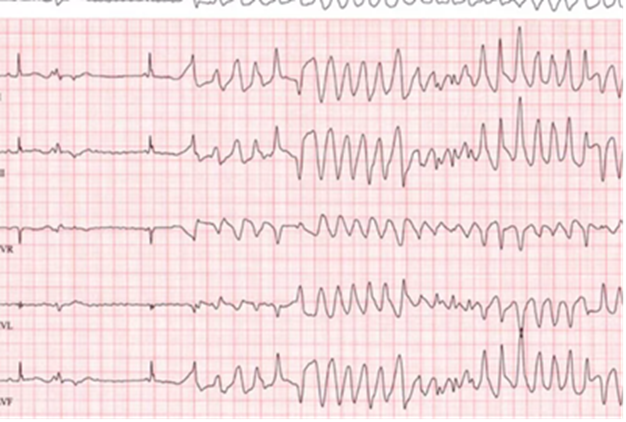
During electrocardiography, recurrent loss of consciousness for 1 minute is noted. ECG- revealed polymorphic ventricular tachycardia with rapid irregular QRS complexes, which look (see photo) like "flipping" around the electrocardiogram isoelectric line.
Questions:
1.What is the patient's diagnosis?
2. What is most likely to have caused this condition?
3. How should this condition be treated?
(Correct answer - )
Kuat Abzaliev
Department of Clinical Disciplines, Al-Farabi Kazakh National University, Almaty Kazakhstan
Peer-review: Internal
Conflicts of interest: None to declare
Authorship: K.A.
Acknowledgement and funding: None to declare
Note: Media adapted from other free online sources are reproduced under CC-BY license and fair use for educational purposes.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

