A case report: A severe juxta-ductal coarctation of aorta with post coarctation aortic aneurysm
CASE REPORT
A case report: A severe juxta-ductal coarctation of aorta with post coarctation aortic aneurysm
Article Summary
- DOI: 10.24969/hvt.2023.381
- CARDIOVASCULAR DISEASES
- Published: 29/03/2023
- Received: 31/01/2023
- Revised: 25/03/2023
- Accepted: 26/03/2023
- Views: 6138
- Downloads: 4022
- Keywords: Aortic coarctation, aortic surgery, post coarctation aneurysm, ventral repair
Address for Correspondence: Jignesh Kothari, U. N. Mehta Institute of Cardiology and Research Centre, (Affiliated to B. J. Medical College), New Civil Hospital Campus, Asarwa, Ahmedabad-380016, India
Email: jvks20@yahoo.com Phone: +93 9825845972, Fax: +93 07922682092
Kush Bhatt, Utkarsh Sanghavi, Devvrat Desai, Jignesh Kothari
Department of Cardiovascular and Thoracic Surgery, U. N. Mehta Institute of Cardiology and Research Centre, (Affiliated to B. J. Medical College), New Civil Hospital Campus, Asarwa, Ahmedabad-380016, India
Abstract
Objective: Coarctation of aorta with post coarctation aneurysm is a congenital malformation of the aorta which usually occurs in undiagnosed and long standing coarctation and present in third to fifth decade of life. In this case, we present technique of differential hypothermia used to repair coarctation and post coarctation aneurysm: meticulous repair of coarctation segment and aneurysm without compromising blood flow to the vital organs distal to the coarctation segment.
Case report: A 44-year old male patient with severe juxtaductal coarctation of aorta with post coarctation aortic aneurysm who was relatively asymptomatic until he presented with hypertension since 6 months in his fifth decade of life was admitted to our hospital. The patient was managed with surgery of coarctation of aorta and aneurysm repair using dual arterial cannulation and maintaining selective antegrade cerebral perfusion.
Conclusion: Differential hypothermia allows meticulous repair of coarctation segment and post coarctation aneurysm without compromising blood flow to vital organs and and better neurological recovery.
Key words: Aortic coarctation, aortic surgery, post coarctation aneurysm, ventral repair
Introduction
Coarctation of aorta with large post coarctation aneurysm is rare and can be calcified and thrombosed in long standing cases when the patient present in the later part of their life. These aneurysms can be densely adhered to surrounding vital structures like left main bronchus and left lung or may be compressing proximal part of descending thoracic aorta. Surgery in such cases can be challenging because of the complex anatomy and should be done meticulously without compromising blood flow to vital organs distal to coarctation and without neurological complications.
In our case the aneurysm was large with calcification and was densely adhered to surrounding vital structures. We present technique of differential hypothermia used to repair coarctation and post coarctation aneurysm: meticulous repair of coarctation segment and aneurysm without compromising blood flow to the vital organs distal to the coarctation segment.
Case Presentation
A 44-year-old man was admitted to our hospital with complaints of progressive fatigue and exertional dyspnea for 6 months. He had a medical history of refractory uncontrolled hypertension and complaints of occasional headache. Physical examination showed blood pressure 158/86 in both upper limbs, a heart rate of 82 beats/minute. Femoral pulses were palpable bilaterally but were feeble and delayed compared to the brachial pulses. Ankle pressure was 124/70 mmHg in both the lower limbs.
2-Dimensional echocardiography
Echocardiogram showed aortic annulus of 27 mm in size, aortic root: 35 mm sino-tubular junction: 26 mm, descending thoracic aorta (DTA) at diaphragm level: 32 mm. Post ductal coarctation of aorta with peak gradient: 70 mmHg, narrowest part measuring: 6.5 mm. Pre-stenotic segment: 22 mm. Normal left ventricle (LV) size and fair LV systolic function. Chest radiograph demonstrated enlarged aortic knuckle with calcification suggestive of aneurysmal dilatation of arch of aorta. (Fig. 1A).
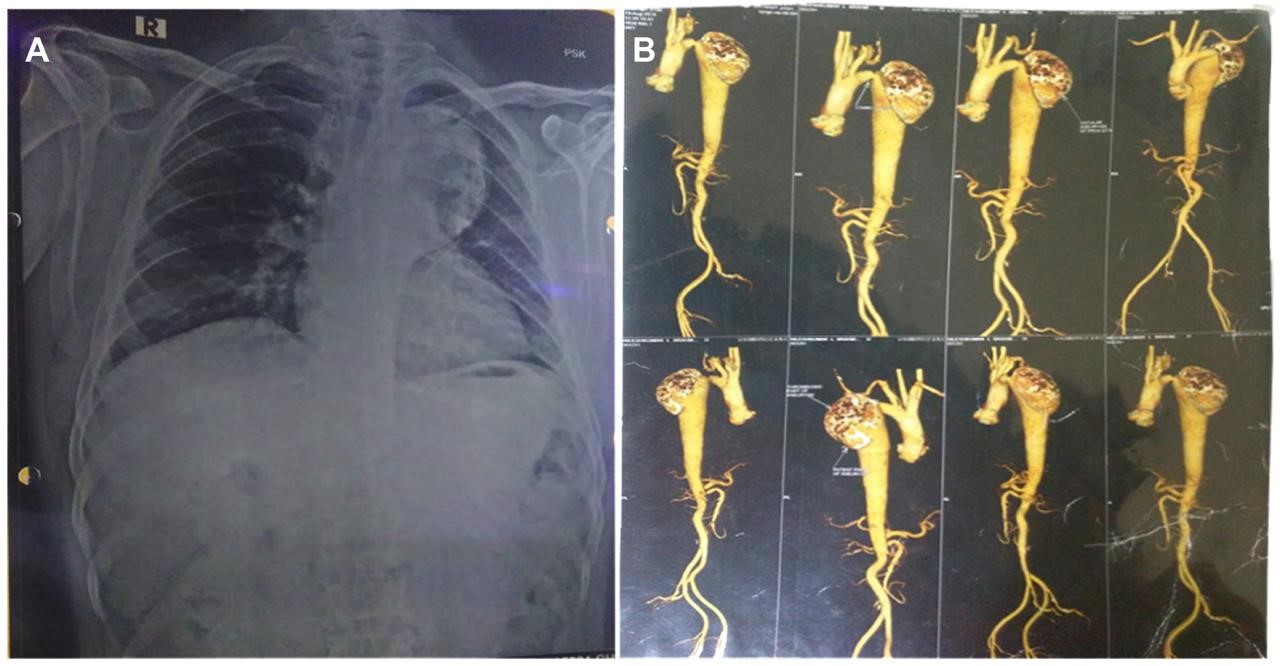
Figure 1. Preoperative chest X-ray (A) and computed tomography aortogram (B) – see text for description
Computed tomography (CT) aortogram
Juxta ductal coarctation. Coarctation segment is measured as 7.3x6.8 mm in caliber 2 cm from left subclavian artery. Large predominantly thrombosed saccular aneurysm arising from proximal DTA. Calcification involving wall of aneurysm as well as in thrombosed aneurysm. Saccular aneurysm was causing compression over patent proximal DTA. Total aneurysm was 70.3x58 mm in axial plane with craniocaudal extent of 98 mm; patent portion was 41x20.5 mm in axial plane. Largest part of neck of communication was 41.3 mm in transverse plane with craniocaudal extent of 33.6 mm (Fig. 1b).

Figure 2. Cannulation strategy
Thus, the patient had indication for repair of post-ductal coarctation of aorta and aneurysm. Initially, the case was discussed with endovascular team who had refused endovascular stenting. It was decided to proceed with surgery.
Cannulation strategy (Fig. 2)
Aims: 1) to maintain cerebral circulation 2) to maintain perfusion to spinal cord and vital organs distal to coarctation segment during cardiopulmonary bypass (CPB).
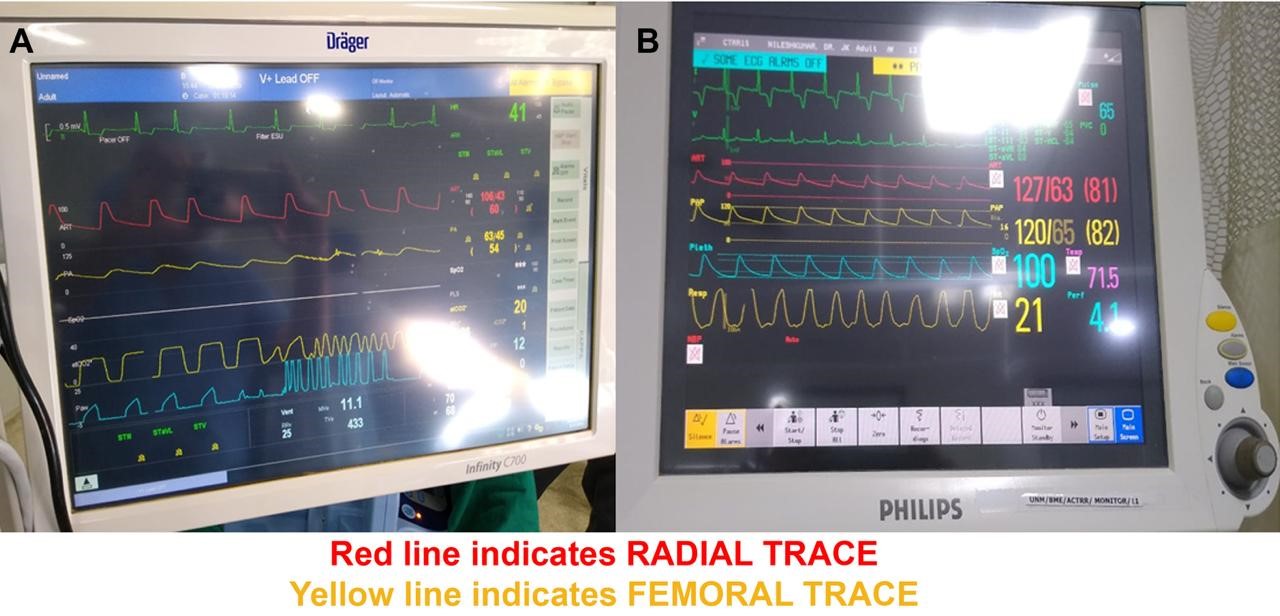
Figure 3. Detailed monitoring of hemodynamics through two invasive arterial lines
Operative strategy
After obtaining of informed consent, we started detailed monitoring of hemodynamics through two invasive arterial lines i.e right radial and left femoral artery (Fig. 3). As the aneurysm was very large in dimensions and could be adhered to the surrounding vital structures like left main bronchus and left upper lobe and was thrombosed and calcified which could affect the mobility and dissection, it was decided to proceed with midline sternotomy and not thoracotomy.
Midline sternotomy and pericardiotomy were performed. Under systemic heparinisation right axillary artery, superior vena cava (SVC), inferior vena cava (IVC) and left femoral artery were cannulated (Fig. 2).
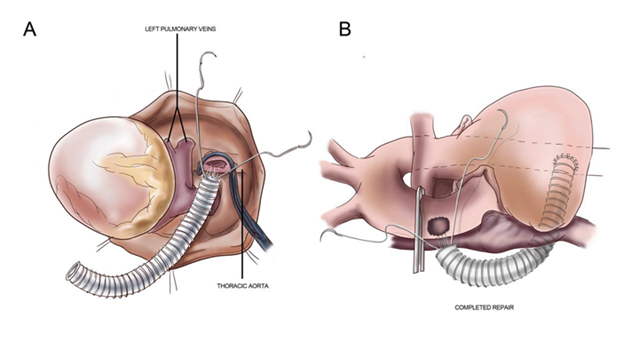
Figure 4. Procedure of aneurysmal cavity decalcification and the false lumen closure using multiple pledgetted polypropylene sutures
Right innominate and left common carotid artery (CCA) were isolated and looped. After establishing complete CPB, DTA was mobilized in posterior mediastinum distal to coarctation segment. Aorta was cross-clamped and antegrade root cold blood cardioplegia was given to achieve instantaneous electromechanical diastolic arrest. The 16 mm polytetrafluoroethylene (PTFE) graft was anastomosed distally on ventral aorta using side biting clamp (Fig. 4A). Proximal end of PTFE graft was traversed through oblique sinus between right inferior pulmonary vein and posterior portion of IVC and was kept near the ascending aorta.
Under profound hypothermic arrest with drifting of temperature to 20 degree Celsius selective antegrade cerebral perfusion (SACP) was maintained through axillary cannulation, (from right innominate to internal carotid artery (ICA) and circle of WILLIS). Lower body perfusion distal to coarctation was maintained through left femoral artery cannula. Total circulatory arrest of lower body was achieved after clamping left femoral artery and IVC cannula.
Aneurysmal cavity was decalcified and the false lumen was plicated using multiple pledgetted polypropylene sutures with buttressing native aortic walls (Fig. 4B). Rewarming was commenced. Proximally graft was anastomosed to ascending aorta using partial aortic clamp under partial CPB support. Total circulatory arrest (TCA) time for lower body part was 80 minutes. After complete rewarming, CPB was weaned off uneventfully. In view of impending risk of diffuse hemorrhage from surrounding raw area of dissection, chest cavity was packed for 24 hours and closed uneventfully the next day with stable hemodynamics.
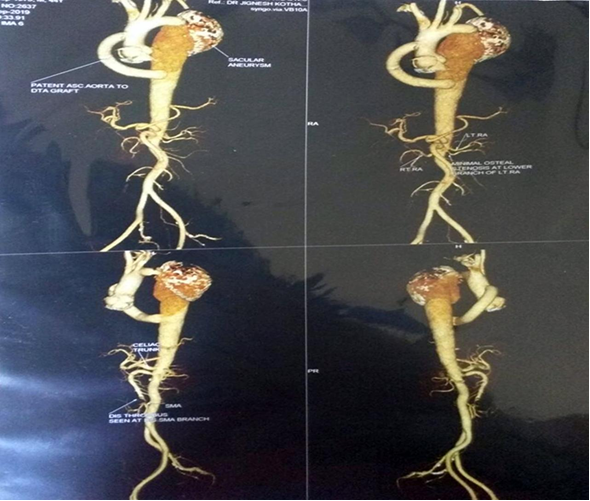
Figure 5. Postoperative computed tomography aortogram
Postoperative period
Post operatively upper and lower limb pressures were equal (Fig. 3B). Follow up CT aortogram showed patent graft from ascending aorta to descending thoracic aorta- bypassing the coarcted segment with no leak from aneurysm (Fig. 5). Postoperative echocardiogram showed good LV function, no effusion, no regional wall motion abnormality at rest.
Patient was discharged uneventfully.
Discussion
Coarctation of aorta is a congenital vascular lesion, which is usually diagnosed, in early life, and accounts for 5 to 10% of all congenital cardiovascular malformations (1) but it may be undetected well until adulthood (2). It usually manifests as childhood hypertension, lower extremity fatigue or weakness, diminished lower extremity pulses and/or congestive heart failure. Diagnosis is usually based on clinical suspicion and physical findings (3), which include blood pressure difference between the upper and lower extremities, delay in pulses between upper and lower limbs and a systolic murmur over the thoracic spine. Other manifestations include bicuspid aortic valve, systolic ejection murmur and neurological complaints. Prognosis and survival depend on the disease severity and patient’s age at the time of presentation. Causes of mortality in coarctation can be heart failure, coronary artery disease, aortic rupture/dissection, concomitant aortic valve disease, infective endocarditis, or cerebral hemorrhage (4, 5). Few patients in the past were first diagnosed at a very late age (2, 6, 7). Treatment of coarctation includes aggressive control of hypertension, prophylaxis of endocarditis and surgical or percutaneous correction of coarctation with a high gradient (8).
Our cannulation strategy to perfuse both ascending and descending aorta allows avoiding under-perfusion distal to the coarctation and gives adequate time for meticulous repair of aneurysm. On CPB with collaterals, distal body perfusion is likely to be hampered because of non-pulsatile flow and low-pressure collaterals are not adequate. This cannulation strategy maintains blood supply and adequate perfusion pressure in body distal to the coarctation segment so abdominal visceral and spinal cord ischemia and other neurological complications are avoided.
We maintained antegrade cerebral perfusion through axillary artery cannulation, (from right innominate to ICA and circle of WILLIS). These also circumvents cerebral embolism. Postoperatively, neurological recovery was uneventful as compared to other patients who undergo total circulatory arrest.
The weaknesses in this report are as following: we cannulated two arteries and used sternotomy approach instead of thoracotomy as the aneurysm was very large and densely adhered to the surrounding vital structures.
Conclusion
The differential hypothermia (lower body TCA with selective antegrade cerebral perfusion of upper body) with double cannulation strategy helps uneventful neurological recovery, spinal cord and abdominal visceral protection (kidney and intestine) with ample time for meticulous repair of aorta coarctation and aneurysm.
Ethics: Written patient consent form was obtained before all procedures
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: K.B., U.S., D.D., and J. K. equally contributed to the preparation of manuscript and management of patient
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

