Left atrial myxoma as a rare cause of acute hemiplegia in an 8-year-old child
CASE REPORT
Left atrial myxoma as a rare cause of acute hemiplegia in an 8-year-old child
Article Summary
- DOI: 10.24969/hvt.2023.383
- CARDIOVASCULAR DISEASES
- Published: 26/04/2023
- Received: 18/02/2023
- Revised: 18/04/2023
- Accepted: 24/04/2023
- Views: 4606
- Downloads: 4004
- Keywords: myxoma, hemiplegia, gelatinous mass, benign
Address for Correspondence*: HC Ramesh, Department of Cardiothoracic Vascular Surgery, Sri Jayadeva Institute of Cardiovascular Science and Research , Bangalore, Karnataka, India E-mail: ddr.hc.ramesh@gmail.com
Amulya Cherukumudi, Chandrashekhar Hebbale Ramesh, Raju Varadaraju, Neville Tata
Department of Cardiothoracic Vascular Surgery, Sri Jayadeva Institute of Cardiovascular Science and Research, Bangalore, Karnataka, India
Abstract
Objective: Myxomas are uncommon in the pediatric age group. However, acute cerebral infarcts in children are most often secondary to a myxoma. Early diagnosis is essential in such cases to prevent further such episodes, thereby decreasing the risk of permanent neurological deficits. In the pediatric age group, a high index of suspicion is required to diagnose such rare causes. Most myxomas are benign in nature, and hence surgery can offer complete curative resection and also help avoiding further incidents of cerebrovascular accidents (CVA). Here, we present an interesting case of an 8-year-old female child who presented with acute right-sided hemiplegia and was incidentally detected with a left atrial myxoma.
Case presentation: An 8-year-old female presented to the emergency department with the complaint of loss of consciousness for 1 hour. There was no preceding history of trauma and no associated seizures.Computed tomography and magnetic resonance imaging of brain revealed an acute thalamic infarct and 2D echocardiography showed a mass lesion in the left atrium. Mass was excised, and histopathology confirmed it as a benign myxoma.
Conclusion: Myxomas are a rare cause of CVA in children, making the diagnosis challenging. A high index of suspicion with a multidisciplinary approach is necessary for early diagnosis and appropriate management of such cases.
Key words: myxoma, hemiplegia, gelatinous mass, benign
Introduction
Atrial myxomas are a common benign tumor in adults but are rare in the pediatric population (1, 2). The most common cardiac tumor of in children is rhabdomyosarcoma. Myxoma rarely cause cerebrovascular accidents in children and is often this event which helps diagnose the tumor. The highest incidence according to observational studies occurs in the first year of life, particularly among neonates, and the nadir occurs in mid-childhood (1, 2). Mallick et al. (2) reported that one-third of all cases are secondary to arteriopathy, likely related to infection, and around 20% of ischemic strokes are cardioembolic. Among cardiac disorders, the majority of cerebrovascular accidents (CVAs) are related to congenital heart disease while others are secondary to acquired cardiac disease.
In this respect, cardiac myxomas are a rare cause of brain emboli in the pediatric population. In such cases, surgery is the treatment of choice, and early treatment can help prevent permanent neurological deficits in these children. The chance of recurrence is very minimal in the case of atrial myxomas, and this offers good outcomes for these patients after surgery.
Here, we present an interesting case of acute thalamic hemiparesis, which was found to be secondary to a left atrial myxoma.
Case report
An 8-year-old female presented to the emergency department with a complaint of loss of consciousness for 1 hour. There was no preceding history of trauma and no associated seizures. There were no such episodes in the past either. The child was born via a normal vaginal delivery at term, and there were no complications during or following the delivery.
On the initial examination, the child was unconscious, and responding only to painful stimuli. Glasgow coma score was E3V4M3. Hemodynamic parameters were stable on the initial examination. Patient was transferred to a Pediatric intensive care unit, and started on medications. Once she regained consciousness, it was observed that she had flaccid paresis of the right upper and lower limb, with a power of 2/5. There was no facial deviation or slurring of speech.
Computed tomography scan was performed, which revealed an acute non-hemorrhagic infarct involving the left lenticulostriate arteries of the left middle cerebral artery territory including left basal ganglia.
Magnetic resonance imaging with magnetic resonance angiography was performed, which showed an acute infarct with hemorrhagic transformation in left basal ganglia, lateral thalamus and medial temporal lobe.
2D echocardiography was done to evaluate for the etiology, and they found a 4.2 x 2.3 cm mass in the left atrium, which was free from the mitral valve leaflets.
A working diagnosis of thrombus and left atrial myxoma was made.
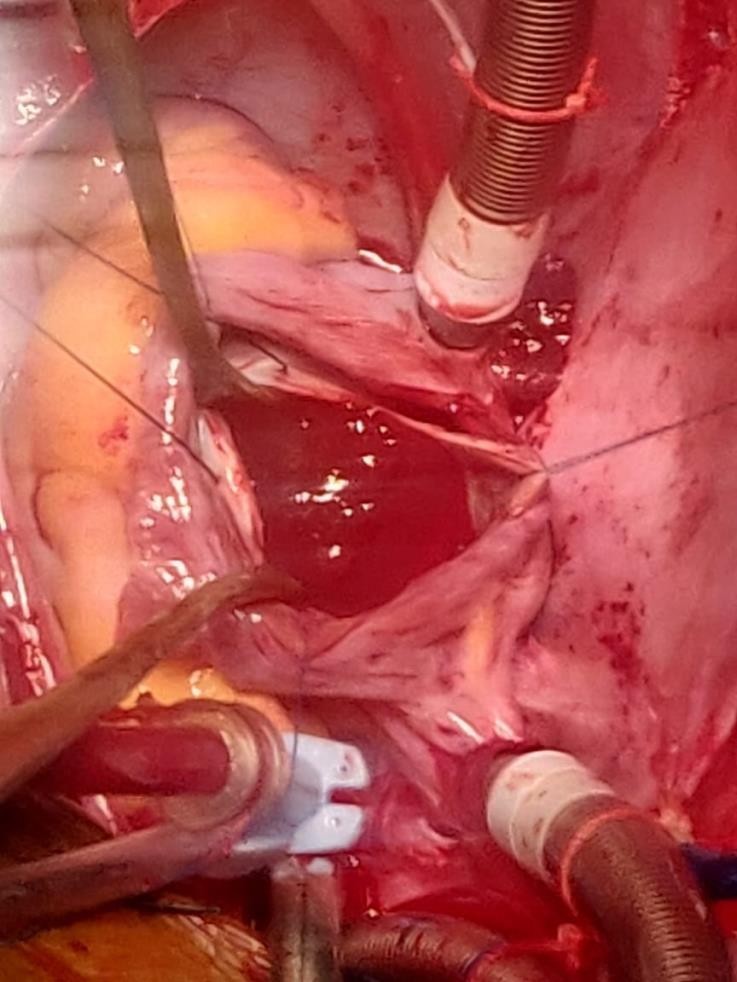
Figure 1. Intraoperative findings of friable gelatinous mass in the left atrium
The child was evaluated, and was regularly being followed up by a pediatric neurologist and pediatric cardiologist. For the neurological deficit, child was initiated on anti-platelet drugs and provided physiotherapy to improve the deficit. Following admission, a detailed discussion was conducted with the pediatric neurologist and cardiologist, and it was decided to operate at the earliest, fearing the risk of another embolic event. Once fitness was sought, routine blood work up was performed, and patient was taken up for surgery. Intraoperatively, a gelatinous, friable mass was found to be attached to the interatrial septum, measuring about 5 x 3 cm. The mass was extracted piecemeal (Fig. 1). There was no involvement of the mitral valve.
The defect in the interatrial septum was closed with an untreated autologous pericardial patch. The postoperative period was uneventful, and the patient was discharged. On subsequent follow-up, there was no evidence of any remnant mass or clot. The child did not demonstrate any neurological deterioration following surgery. To allow for epithelialization of the autopericardial patch used for closure of the defect, as well as the CVA, the child was maintained and discharged on anti-platelet medications.
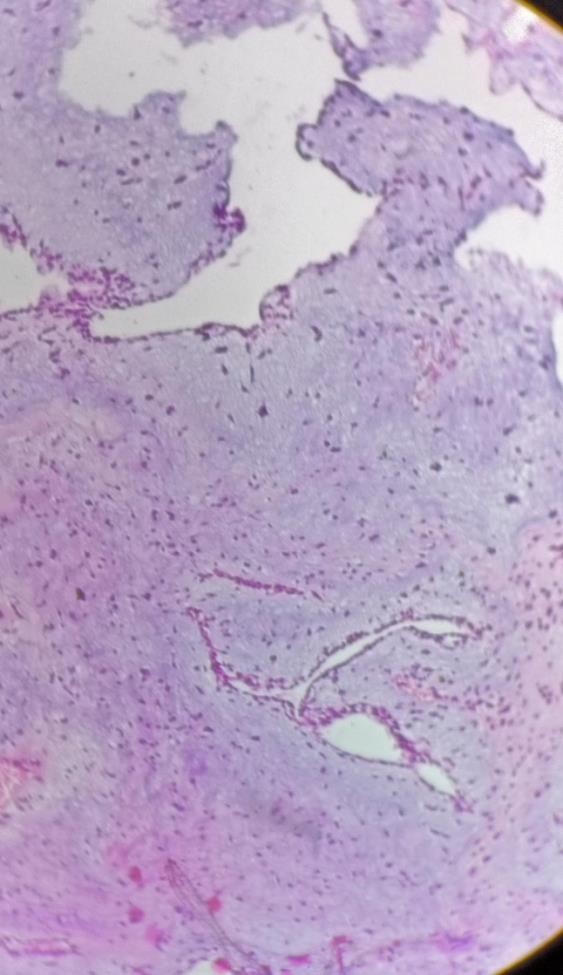
Figure 2. Histopathology of tumor specimen showing myxomatous cells
Histopathology was suggestive of a benign left atrial myxoma (Fig. 2).
Discussion
Primary cardiac tumors in childhood are extremely rare. A prevalence of up to 0.28% in autopsy studies and an incidence rate of 1.38 per 100.000/residents in a population-based cohort have been reported (?). Over 90% of these tumors are benign and the most common types are rhabdomyoma and fibroma. Although most tumors are incidental, they may as well be responsible for cardiac murmurs, shortness of breath, syncope, fever of unknown origin and embolic events (3). Myxomas can be isolated or part of a syndrome complex. For Carney’s complex, which comprises myxomas, pigmentation of the skin and mucosa and endocrine abnormalities, this is an autosomal dominant in origin. Several genetic mutations have also been identified, such as PRKAR1 on chr 17 (4).
Overall, 95% of all cardiac myxomas are atrial in origin and can be pedunculated or sessile. Most patients remain asymptomatic, whereas in 15% cases, they can develop sudden cardiac death. In the pediatric population, cardiac myxomas frequently result in acute infarcts, and it is incidentally detected (4).
There are very few case reports/series that have analyzed the CVAs secondary to myxoma in the pediatric age group, and there is limited data regarding the subsequent prognosis and remnant neurological deficit.
A review was conducted on 9 cases of LA myxoma in children, and it was found that right hemiparesis was the most common finding (8/9). Other common symptoms documented were red spots on the limbs (44%), aphasia (44%), lethargy (22%), seizures, headache, blindness, slurred speech, dizziness and diplopia (11%). Pridie et al. also described three children with cardiac myxoma; all had systemic emboli involving the central nervous system (5).
As it is a benign tumor, early diagnosis and surgical resection offers complete cure (6, 7).
In this case, the decision to remove the tumor was made once the neurological deficit had resolved satisfactorily. As with adults, complete excision of the myxoma is the curative aspect of management, and the same applies to the pediatric age group. However, prior to surgery, a thorough evaluation of other causes of CVA in the pediatric population as mentioned above must be ruled out.
Conclusion
Atrial myxomas are a rare finding in the pediatric population, and most often result in acute CVA. Early diagnosis and timely treatment is necessary to prevent permanent neurological impairment.
The take-away message from this case report is that to maintain a high index of suspicion when we encounter children with CVAs, and evaluate the cardiovascular system to rule out thrombus, valve lesions and vegetations, and in rare situations, a myxoma.
Ethics: Patient`s informed consent was obtained before all procedures
Peer-review: Internal and external
Conflicts of interest: None to declare
Authorship: A.Ch., H.C.R., R.V., N.T. equally contributed to management of patient and preparation of manuscript.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution 4.0 International License.
AUTHOR'S CORNER

