Long-term tendency and risk factors for stroke in Bishkek
ORIGINAL RESEARCH ARTICLE
Long-term tendency and risk factors for stroke in Bishkek
Article Summary
- DOI: 10.24969/hvt.2023.384
- RELEVANT DISCIPLINES
- Published: 30/04/2023
- Received: 10/03/2023
- Revised: 24/04/2023
- Accepted: 26/04/2023
- Views: 6175
- Downloads: 4338
- Keywords:
Address for Correspondence*: Mirgul B. Yrysova, General and clinical epidemiology department I. K. Akhunbaev Kyrgyz State Medical Academy, 92 Akhunbaev Street, Bishkek, 720020, Kyrgyzstan
Email: yrysovamirgul@gmail.com, Mobile: +996550501039
Mirgul B. Yrysova1,2*, Keneshbek B. Yrysov2, Tatyna T. Samudinova3,4, Rakhat I. Toichibaeva1,2, Omor T. Kasymov1
1 National Institute of Public Health, Ministry of Health of the Kyrgyz Republic
2 I. K. Akhunbaev Kyrgyz State Medical Academy, Bishkek, Kyrgyz Republic
3 Kyrgyz Research Institute of Health Resort Science and Rehabilitative Medicine, Ministry of Health of the Kyrgyz Republic, Bishkek, Kyrgyz Republic
4 Stroke Registry at the Center for Emergency Medicine (CEM) in Bishkek, Ministry of Health of the Kyrgyz Republic, Bishkek, Kyrgyz Republic
Abstract
Objective: This retrospective study was designed to describe the morbidity, mortality rates and risk factors in adult urban population Bishkek, Kyrgyz Republic for the period 2004–2019 using data from the Stroke Registry.
Methods: The data were derived from Stroke Registry between 2004 and 2019 in Bishkek through examination of records of patients admitted to hospitals and those receiving treatment at home prescribed by doctors of Registry.
A retrospective epidemiological study of the long-term dynamics of the morbidity and mortality rates between 2004 and 2019 was performed. The growth (drawdown) rate was calculated using the least-squares method to align the time series. A comparative analysis of the rates was carried out by calculating the long-term average annual level of incidence by gender and age. Ethical approval was not necessary for the preparation of this article.
Results: The most common type of stroke registered for the population of Bishkek was ischemic stroke (IS) (68.5%), followed by hemorrhagic stroke (HS) (21.4%) and cryptogenic stroke (10.1%). During the analyzed period of time there has been a moderate decrease in the incidence of IS (4,0%) and a notable decrease of HS (9,0%) and cryptogenic (26,9%) strokes. As for stroke mortality in long-term dynamics, we could observe an essential decrease in this indicator in all strokes (IS-13.0%, HS 13.6%, cryptogenic ones-37.7%).
The most remarkable risk factor for stroke was arterial hypertension (86.5%). Cardiovascular pathology of another origin was detected in 32.7% of patients.
Conclusion: Our results further help to understand what changes have been in the long-term dynamics of the incidence and mortality of stroke in Kyrgyzstan, in relation to which risk factors for stroke should be taken more action. There is a need to continue to strengthen prevention at the population level, to assess and manage the risk of cardiovascular disease in primary healthcare. Such measures will help prevent complications and support efforts to prevent relapse and disability.
Key words: epidemiology, hemorrhagic stroke, ischemic stroke, cryptogenic stroke, risk factors, morbidity, mortality
Introduction
Bishkek is the capital and largest city in Kyrgyzstan with a population of 1,027,200 people (at the beginning of 2019) (1). Mortality from strokes in Kyrgyzstan is high (2, 3).According to the data of the Republican Medical Information Center of the Ministry of Health of the Kyrgyz Republic, there are more than 185 deaths per 100,000 people per year, with 34.6% of victims dying from a stroke within a month and one in two within a year. Of those who survive, only 20% manage an almost complete recovery (defined as not being assigned to a disability group), 18% presented with aphasia, and 48% developed kinetic problems (4).
In the Kyrgyz Republic, no studies have been conducted to identify the features of stroke in long-term tendency and concerning the risk determinants of stroke. In 1997, a stroke registry was established for the capital city of Bishkek and oblast of Osh. At present, this registry is functioning only in the capital and is managed by the same emergency agency that manages the ambulance system.
There are no reliable sources of information on the epidemiology of stroke for the rest of the country. In the regions of the republic, there is currently neither sufficient experience nor infrastructure to create a stroke registry (2).
The purpose of this study was to assess the dynamics of long-term trends in the prevalence and incidence of strokes and to study risk factors among the urban population using data from the stroke registry in Bishkek.
Methods
Study design – retrospective cohort study (based on prospective registry data). Data from the Stroke Registry of Bishkek was used for the epidemiological analysis of stroke incidence and mortality of the adult population.
Study population - residents of Bishkek. The study included stroke cases that met the diagnostic criteria; stroke in a person permanently residing in the study area; the case must be discovered and clinically diagnosed by physicians as a "stroke" within 28 days of its onset; the case must meet the criteria for "stroke" or "death by stroke".
Excluded from the study were cases of stroke that did not meet diagnostic criteria; non-residents of the studied city; "misdiagnosed case of stroke" (false positive) when the case was initially regarded by doctors as a stroke, but later it turned out that it had a different cause (for example, oncological pathology); cases of transient cerebral ischemia or stroke in blood diseases (leukemia, polycythemia), tumors or metastatic brain lesions; secondary stroke caused by trauma. Ethical approval was not necessary for the preparation of this article.
Variables
Demographic data, cardiac comorbidities and risk factors were retrieved from patient’s records: sex, age, risk factors as hypertension, diabetes, overweight, smoking, coronary heart disease, history of myocardial infarction, atrial fibrillation, previous stroke, mortality.
Definitions
Hypertension was defined as systolic blood pressure ≥140mm of Hg and diastolic blood pressure ≥90mm of Hg (5). Overweight was defined as body mass index ≥25 kg/m2, which also included obesity (BMI ≥30 kg/m2) (6). Diabetes type 2, was included as a risk factor if the patient was taking hypoglycemic drugs at the time of the stroke or if it was first detected in the hospital (7).
The American Stroke Association definitions of stroke definition were used in our study (8):
-Ischemic stroke (IS) occurs when the vessel supplying blood to brain is obstructed. It accounts for 87% of all strokes.
-Hemorrhagic stroke (HS) (bleeds) occurs when a weakened blood vessel ruptures – usually aneurysms and arterio-venous malformations. The most common cause of hemorrhagic stroke is uncontrolled high blood pressure.
Cryptogenic stroke is caused when by a blood clot that blocks the flow to the brain and in most instances, the cause of a stroke cannot be determined.
Statistical analysis
A retrospective epidemiological study of the long-term trends of the prevalence and incidence of stroke between 2004–2019 was performed. The growth (drawdown) rate was calculated using the least-squares method to align the time series. A comparative analysis of the indicators was carried out by calculating the long-term average annual level of incidence by gender and age. According to the value of the growth (drawdown) rate, the tendency was estimated as follows:
With a rate value in the range:
0 to ± 1%—the tendency is considered stable;
±1.1% to ±5.0%—the tendency is assessed as moderate;
more than ±5%—the tendency is significant (9). Within the framework of the register, those risk factors that have objective confirmation were taken into account (medical documentation, results of previous medical examinations, laboratory analysis data). Shapiro-Wilk test were used to determine the normality of distributions. Statistical processing of the results was carried out using the specialized software packages Statistica 10.0 (StatSoft Inc.) and SPSS 16 FULL for Windows (SPSS Inc., USA).
Results
During the analyzed period 23299 cases of stroke (males – 10869 (46.65%), female – 12430 (53.34%)) were registered, including 15965 cases of ischemic IS (68.5%), 4975 cases of HS (21.4%), and 2359 cases of cryptogenic strokes (10.1%). For 2004-2019 there is a moderate decrease in the incidence of IS (4.0%) and a notable decrease in this indicator of HS (9.0%) and cryptogenic strokes (26.9%) compared with before 2004 (Fig. 1).
As for stroke mortality in long-term dynamics, we can observe an essential decrease in this indicator in all strokes (IS-13.0%, HS 13.6%), especially in cryptogenic ones (37.7%) (Fig. 1).
The registry data for the analyzed period revealed a remarkable increase in morbidity and mortality from strokes with age. The incidence of IS across various age groups in Bishkek increased from 2.5% (< 40 years old) to 51.0% (> 70 years old) (Fig. 2a).
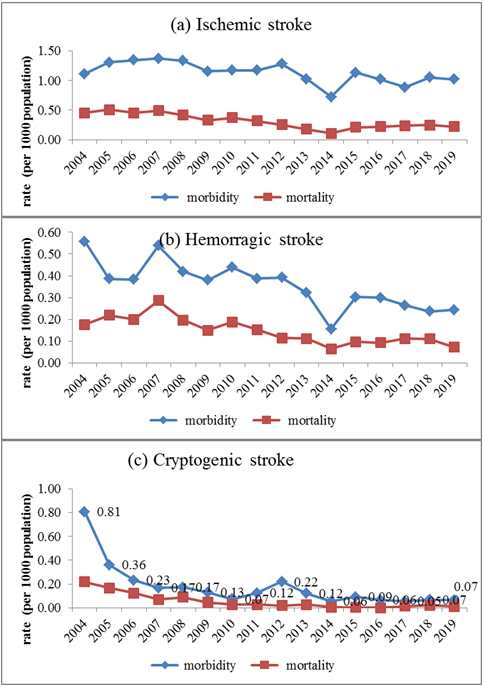
Figure 1. Morbidity and mortality rates of strokes in Bishkek between 2014 and 2019
The same pattern was observed for mortality from IS, where the mortality rate increased 2.3–4-fold for each ten-year age period. The incidence of IS in the over 70 years age group was significantly higher among women (32.7%) than among men (18.3%) (p<0.05). The number of deaths from cerebral infarction in women (47.3%) was two-fold higher than in men (23.5%) (p<0.05).
Similar trends were observed with HS (Fig. 2b). There was an increase in morbidity and mortality rates with age: 1.5–2.2-fold and 1.03–2.8-fold, respectively, with each ten-year step. The highest rates of morbidity and mortality in the over 70 year’s age group were 35.3% and 44.6%, respectively.
Notably, HS was more common than IS in people under 40 years of age (6.0% of cases and 3.4% of deaths from HS, compared with 2.5% of cases and 0.9% of deaths from IS).
The mortality of women is significantly higher (p<0.05) in the age group over 70 years. In other age groups, there was no statistically significant difference between mortality rates by sex.
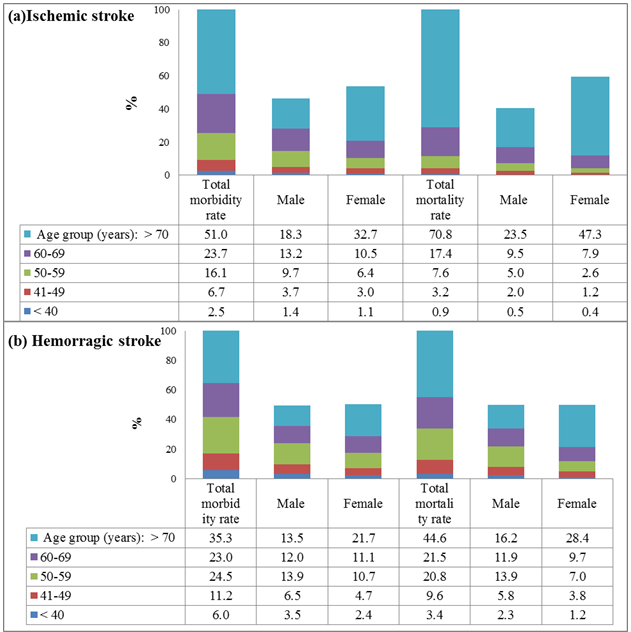
Figure 2. Morbidity and mortality by age and gender in ischemic (a) and hemorrhagic (b) stroke patients.
Of the identified risk factors, the most significant (86.5%) was arterial hypertension (Table 1). Structural heart diseases (coronary heart disease, history of myocardial infarction, atrial fibrillation) were identified in 32.7% of patients. Previous strokes were identified in 17.3% of patients according to the anamneses, conclusions of neuroimaging methods, and outpatient records. Overweight was recorded in 16.8% of patients. Type 2 diabetes (9.7% of patients) was included as a risk factor if the patient was taking hypoglycemic drugs at the time of the stroke or if it was first detected in the hospital. Smoking were noted by 9.4% of patients. In a comparative analysis of risk factors by gender, statistically significant differences were found for the following indicators: hypertension and overweight, which were more common in women, and cardiovascular pathology and smoking in men.
|
Table 1. Cardiovascular risk factors in stroke patients |
|||||||||
|
Risk factors |
Total n=23299 |
Male |
Female |
||||||
|
% |
SD |
95% CI |
% |
SD |
95% CI |
% |
SD |
95%CI |
|
|
AH * |
86.5 |
0.22 |
86.1-86.9 |
38.7
|
0,32 |
38.1-39.3 |
47.8
|
0,33 |
47.2-48.4 |
|
p<0.01 |
|||||||||
|
Structural heart diseases (coronary heart disease, history of myocardial infarction, atrial fibrillation) |
32.7 |
0.31 |
32.1-33.3 |
17.1 |
0.25 |
16.6-17.6 |
15.6 |
0.24 |
15.1-16.1 |
|
p<0.01 |
|||||||||
|
Recurrent stroke |
17.3 |
0.25 |
16.8-17.8 |
8.8
|
0.19 |
8.4-9.2 |
8.5
|
0.18 |
8.1-8.9 |
|
Overweight ** |
16.8 |
0.24 |
16.3 -17.2 |
4.0
|
0.13
|
3.7-4.3
|
12.9
|
0,22 |
12.5-13.3 |
|
p<0.01 |
|||||||||
|
Diabetes (type 2) |
9.7 |
0.19 |
9.0-9.8 |
5.1
|
0.14
|
4.8-5.4
|
4.6 |
0.14 |
4.3-4.9
|
|
Smoking
|
9.4
|
0.19 |
37.8-39.6 |
6.4
|
0.16 |
6.1-6.7 |
6.4
|
0.16 |
2.8-3.2 |
|
p<0.01 |
|||||||||
|
*Hypertension was defined as systolic blood pressure ≥140mm of Hg and diastolic blood pressure ≥90mm of Hg **Overweight was defined as body mass index ≥25kg/m2 which also included obesity (BMI ≥30) |
|||||||||
Discussion
In Bishkek, the morbidity rates of all types of strokes decreased over the analyzed period. There is also a decrease in the mortality rate in long-term dynamics from strokes, especially from cryptogenic ones. The decline in both morbidity and mortality appears to be associated with improved healthcare delivery.
There are two stroke departments in Bishkek. In recent years, patients prefer to receive care in a hospital rather than stay at home. For example: in 2016, more than 90% of all stroke patients were hospitalized compared to 2011 (70.6%). In a hospital setting, access to specialists such as a cardiologist and angiologist, early neurorehabilitation services, including physiotherapy and speech therapy, is possible. The population also uses private providers of neuroimaging and diagnostic services, whose inpatient care is comparable to that provided by the stroke departments of public clinics (2, 3).
An assessment of the epidemiology of clinical variants of IS in different countries of the world showed that the highest incidence rates were registered in developing and post-Soviet countries (10). The global age-standardized stroke rate has declined significantly in high-income countries and increased in low- and middle-income countries. At the same time, in developed countries such as Sweden or Spain, there is a long-term decrease in the frequency of strokes (over the study period 1980–2017) (11, 12).
Mortality has declined significantly both in high-income countries (37%) and in low- and middle-income countries (20%) (13, 14). Stroke deaths have declined over the past decade, and stroke is now the fifth leading cause of death in the United States (15). In the EU, especially in the countries of Southern and Western Europe, Latin America, and the Caribbean, a similar trend has been observed (16, 17).
Of all strokes registered for the population of Bishkek, IS was the most common, which corresponds to data from other authors (18, 19). For example, in the U.S. and globally, the proportion of IS from all types of strokes is 87% (20, 21). The proportion of cryptogenic strokes in Bishkek remains high compared to other countries (10.1%). In China, the proportion of IS was 77.8%, HS 23.8%, and cryptogenic strokes 2.1% (22).
The registry data for the analyzed period revealed a significant increase in morbidity and mortality from strokes with age. The higher percentage of strokes in older patients confirms the results of previous studies, in which age is considered one of the most important non-modifiable risk factors for all types of strokes (especially IS) (23). The data of authors from other countries show a difference in the rates of morbidity and mortality from strokes by sex, mostly high rates among men (21, 22, 24-28). Morbidity and mortality from IS in the age group over 70 years is significantly higher in women than in men in Bishkek, possibly due to the demographic difference of the population by sex, which increases with age. There are more women in this age group. Life expectancy for men in Bishkek was 69.6 years, for women 79 years in 2019 (1).
The same picture is observed in HS, where morbidity and mortality increases with age, especially in people over 70 years of age (29, 30). Minimum numbers of IS cases and deaths occur in people under 40 years of age, although the authors point to an increase in strokes in young people (31). HS is more common than IS in people younger than 40 years of age. These data coincide with results obtained by other authors (32, 33).
Of the identified risk factors, hypertension was the most significant and is comparable with the results obtained by other authors (22, 29, 34, 35). Statistical analysis has revealed the key reasons for the lack of control of hypertension in Kyrgyzstan. A very low level of hypertension diagnoses was highlighted, despite the prevalence of hypertension being 30–40%, according to various studies. For 20 years, the healthcare system has been trying to increase the level of diagnosis. According to the final report on the control of hypertension in all regions of Kyrgyzstan under the leadership of the WHO regional office, together with employees of the Central Economic Health Center of the Ministry of Health of the Kyrgyz Republic and the National Center for Cardiology and Therapy, the level of diagnosis of hypertension in each Family Medical Center was about 4–5% (4).
Identification of the cardiogenic mechanism of IS is of great therapeutic importance. IS due to myocardial infarction may develop as a result of cardiac embolism or systemic fall in blood pressure, and hemorrhagic - due to the use of thrombolytics and anticoagulants (36). In 32.7% of patients, heart diseases such as coronary artery disease, a history of myocardial infarction and atrial fibrillation were identified.
Previous strokes were identified in 17.3% of our patients. According to other authors, the frequency of relapses decreased until the mid-2000s but has not changed over the past decade. Repeated strokes still account for 25–30% of all strokes and represent unsuccessful secondary prevention (37). Most recurrences of cardioembolic or HS are of the same type, indicating that effective preventive strategies in these cases are still suboptimal (38). Dyslipidemia and overweight is more common in young people and is the second most common condition after hypertension (22). Multifactorial treatment of risk factors for stroke, in particular lifestyle factors, hypertension, and dyslipidemia, will prevent a significant number of these disabling strokes (39, 40).
Diabetes mellitus and IS often occur at the same time. People with diabetes are more than twice as likely to have an IS than people without diabetes after correcting for other risk factors. According to some authors, patients with diabetes mellitus may account for 50% or more of the total number of patients with IS, and they have more adverse clinical outcomes compared with individuals without diabetes (39, 41).
Smoking was noted by 9.4% of patients, according to the results of the survey. Smoking was a quite common risk factor (48%), especially in young people (32, 36). According to the INTERSTROKE study, hypertension was more associated with intracerebral hemorrhage than with IS, whereas smoking, diabetes, apolipoproteins, and cardiac pathology were more associated with IS (42).
According to our study, arterial hypertension and dyslipidemia were more common in women, cardiovascular pathology and smoking were more common in men. However, women, given their reproductive status, have a different frequency and significance of risk factors than men.
Risk factors for stroke those are more common in women than men include HS, atrial fibrillation, diabetes mellitus, abdominal obesity, migraine with aura, emotional stress, and depression. Exclusively for women, factors such as the age of menarche, pregnancy, gestational diabetes mellitus, preeclampsia, changes in hormonal status, use of the combined oral contraceptives, and hormone replacement therapy are characteristics (26, 43, 44).
Study limitations
We have limited data on other cardiovascular diseases in patients with stroke, as well as in patients with risk factors such as arterial hypertension, diabetes mellitus, it is impossible to determine the impact of treatment details, patient compliance, drug combinations, insulin status, etc. due to retrospective study design. The another limitation is that we did not investigate regular physical activity, social status, dietary habits, health education, sleep apnea and other novel risk factors.
Conclusions
Long-term dynamics show decreases in morbidity and mortality from strokes of all types in Bishkek, with IS the most common type of stroke observed. Morbidity and mortality rates from IS in people over 70 years of age are observed in more than half of cases. HS is more common than IS in people younger than 40 years of age. Analysis by gender revealed significantly higher rates of IS morbidity and mortality in women; mortality from HS predominates in women over 70 years of age compared with the male population. Dyslipidemia, cardiovascular pathology, smoking, diabetes mellitus, and previous strokes were identified as risk factors, with the most significant being hypertension. Significant differences by gender revealed that hypertension and dyslipidemia were more common in women, and cardiovascular pathology, diabetes and smoking were more common in men.
The results of this study will help to understand what changes have occurred in Kyrgyzstan in the long-term dynamics of morbidity and mortality from stroke, what factors are predetermining in the development of stroke, in respect of which additional measures should be taken. It is necessary to strengthen prevention at the population level, assess and manage the risk of cardiovascular diseases at the level of primary health care. Such measures will help reduce the burden of strokes.
Ethics: Patient`s informed consent was obtained before all procedures
Peer-review: Internal and external
Conflicts of interest: None to declare
Authorship: M.B.Y., K.B.Y., T.T.S., R.I.T., O.T.K. equally contributed to the study and preparation of manuscript.
Acknowledgement and funding: We would like to express our deep thanks to the D.D. Turgumbaev, Kyrgyz State Medical Institute for Retraining and Advanced Studies, Bishkek, Kyrgyz Republic for help in conducting this study.
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

