Anesthetic management of pregnant patients with cardiovascular disease: a commentary on the 2023 American Heart Association (AHA) scientific statement
EDITORIALS
Anesthetic management of pregnant patients with cardiovascular disease: a commentary on the 2023 American Heart Association (AHA) scientific statement
Article Summary
- DOI: 10.24969/hvt.2023.389
- CARDIOVASCULAR DISEASES
- Published: 17/05/2023
- Received: 10/05/2023
- Accepted: 11/05/2023
- Views: 7452
- Downloads: 4567
- Keywords: pregnancy, cardiovascular diseases, anesthesia
Address for Correspondence*: Luigi Spadafora, Department of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, Rome, Italy. Email: luigispadafora167@gmail.com.
Francesca Romana Zimatore1, Annachiara Pingitore2, Stefano Cacciatore3, Francesco Perone4, Matteo Betti5,6, Martina Leonetti7, Luigi Spadafora8
1Sapienza University of Rome, Italy;
2Department of General and Specialistic Surgery ‘Paride Stefanini’ Sapienza University of Rome, Italy
3 Department of Geriatrics and Orthopedics, Università Cattolica del Sacro Cuore, Rome, Italy
4Cardiac Rehabilitation Unit, Rehabilitation Clinic "Villa delle Magnolie", Castel Morrone, Caserta, Italy 5Centro Cardiologico Monzino, IRCCS, Milan, Italy
6Università degli Studi di Milano, Milan, Italy
7Università Cattolica del Sacro Cuore, Rome, Italy
8Department of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, Italy
Abstract
The American Heart Association (AHA) has recently released a statement on cardiovascular management of pregnant women from an anesthesiological point of view. Although managing such situation is extremely frequent in clinical practice, poor attention is paid to the topic and many cardiologists and anesthesiologists in small centers have to cope with cardiovascular complications during pregnancy, being at the forefront as consultants. Consequently, we deem appropriate to dwell on this statement. The aim of the present commentary is to summarize the main practical indications provided by the AHA from a strictly cardiological point of view.
Key words: pregnancy, cardiovascular diseases, anesthesia
“In the end, the truths that count, the great principles, always remain two or three. The ones your mother taught you as a child.”
- Enzo Biagi
Given the great clinical relevance of anesthesiological management of pregnant patients with cardiovascular (CV) issues, American Heart Association (AHA) has released a scientific statement to provide operative tips on the management of some conditions of interest in obstetric cardio-anesthesiology conditions, ranging from the administration of inotropic drugs to the application of transthoracic echocardiography or the indications to invasive mechanical support and many others (1). This statement lays its basis on two fundamental issues: 1) CV drawbacks are the first cause of maternal mortality in the United States, despite relevant advances in anesthesiology peripartum care and CV management of pregnant women; 2) Regardless or not their interest in cardio-obstetrics, cardiologist or anesthesiologist consultants are often required to manage pregnant women with CV issues, especially in small centres (1, 2). Furthermore, anesthesiologists are the physicians who are mostly involved in managing CV acuteness in pregnant women, due to their greater versatility and ability to provide intensive care, which is of crucial importance in this setting (3).
Moreover, peculiar features make the management of CV disease in pregnancy challenging. Firstly, it is difficult to discriminate the onset of CV signs and symptoms from the normal physiological adaptations that occur during pregnancy (4).
Moreover, the administration of several CV drugs is not allowed in pregnancy, since they cross the placental barrier carrying the risk of teratogenicity (5).
Mostly important, it should be borne in mind that managing pregnancy concerns caring about the well-being of both the mother and the fetus, and every medical act must be committed to safeguarding the two people.
For instance, in the case of maternal cardiac arrest, it will be necessary to start the delivery procedures for the baby simultaneously with cardiopulmonary resuscitation in the mother (1, 4).
Nevertheless, there is evidence that safe pregnancy can be achieved with proper care, and that CV risk stratification in pregnant patients is of utmost importance in order to reduce mortality and morbidity (6). For all these reasons it is worth to gauge in detail CV management of pregnant women from an anesthesiological point of view and beyond.
The statement is divided into different sections, each one focusing on a particular aspect of CV care in pregnancy. We analyze them all below (Fig.1).
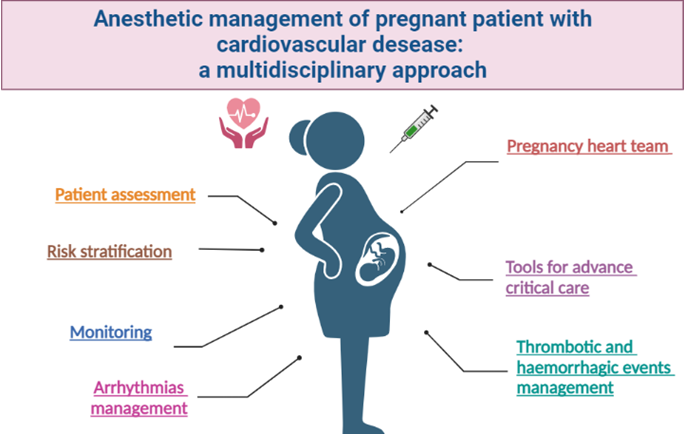
Figure 1. An overview on the anesthetic management of pregnant patients
Patient assessment, risk stratification, pregnancy heart team
The multidisciplinary assessment is the core element for a successful management of pregnant patients with CV disease (CVD), indeed it is demonstrated that a coordinated cardio-obstetrics team can help in preventing severe cardiac complications during pregnancy (1, 6, 7). This team should include gynecologists, cardiologist, critical care nurses and sub-specialized figures in the management of any concomitant diseases, but obviously a key figure is the cardio-obstetrics anesthesiologist (1, 7). The specialized cardio-obstetrics team should consider the complexity of the baseline CV condition and perform a pre-conceptional counseling, in which the women will be informed about pregnancy risks, educated about the need for regular surveillance during pregnancy and postpartum (1, 6), and the medical therapy optimized (discontinuation of any teratogenic medications). Regarding prognostic stratification scores, none of them is perfectly accurate, as they are often based on retrospective studies, although the use of the modified World Health Organization (mWHO) pregnancy risk classification is recommended (1, 8).
Vaginal delivery vs Cesarean delivery
In this section, we find a focus on the most appropriate mode of delivery that should be chosen by the pregnancy heart team, balancing maternal CV risk with fetal and obstetric risk (1, 7). Vaginal natural birth should be the preferred mode of delivery, as it allows more gradual hemodynamic changes with poor obstetric complications.
The main concern related to vaginal delivery regards the Valsalva maneuver which strongly reduces preload and increases aortic shear stress, two relevant issues in valves and aortic diseases (1, 7). Conversely, cesarean delivery should be reserved to patients at a very high CV risk, for instance those with high-risk aortopathy or maternal decompensation (1, 7). For vaginal deliveries, regional anesthesia techniques such as epidural or combined spinal-epidural are preferred due to their effectiveness in providing pain relief, while allowing the patient to remain alert and participate in the birthing process (1, 9). These techniques are generally safe for patients with concomitant CV disease, although close monitoring of blood pressure and heart rate remains mandatory (1, 9). If complications such as hypotension or bradycardia occur, prompt intervention through administration of intravenous fluids or vasopressors is necessary (1, 9). In cesarean deliveries, regional anesthesia is the preferred technique as well (9). In patients with severe CV disease or other medical comorbidities, general anesthesia may be necessary. General anesthesia is associated with a higher risk of adverse maternal and fetal outcomes, including hypertension, hypotension, and respiratory depression, and should be limited to cases of contraindicated or unsuccessful regional anesthesia (1, 7). Overall, the anesthesia technique choice in both vaginal and cesarean deliveries should be based on a thorough evaluation of the patient's medical history, clinical conditions, and preferences, albeit always considering the healthcare provider indications. Goals of a correct management include an adequate uteroplacental perfusion, to be achieved by preventing and treating hypotension and avoiding aortocaval compression and an accurate selection of anesthetic drugs and techniques; it should be taken into account that no anesthetic agent or adjuvant drug has yet been proven to be teratogenic in humans.
When and Where
Timing of delivery is not clearly established and still debated. The statement recommends to achieve 39 weeks of pregnancy, even if this cut-off should be tailored on the concomitant comorbidities and maternal CV risk (1). Regarding place of delivery, it is acknowledged that patients with high CVD risk should deliver at a maternal level IV care center able to provide an eventual emergent cardiac surgery with specialized critical care units (1).
Monitoring and tools for advanced critical care
Monitoring is a crucial issue in advanced maternal care during delivery. As suggested by Langesæter et al., early-onset preeclampsia could be early detected through prompt identification of vasoconstriction and low cardiac output, therefore strict monitoring combined with echocardiography are pivotal to prevent this condition (10). According to the statement, heart rate and blood pressure should be monitored during delivery in all patients, while pulse oximetry and electrocardiographic monitoring should be considered in patients with CVD (1). AHA recommends an immediate evaluation for any pregnant woman with heart rate > 120 beats per minute, peripheral saturation < 95%, respiratory rate > 25 breaths per minute, systolic blood pressure > 160 mmHg (1). Central venous and pulmonary pressure monitoring should be considered in patients with high cardiopulmonary risk, such as those with right ventricular failure (1, 3). Bedside transthoracic echocardiography is the gold standard to assess cardiac function and output assessment with 4 essential implications: 1) stroke volume assessment, 2) global and regional function 3) valvular and ascending aorta assessment, 4) pericardial effusions (1, 11). As a last line of support, ExtraCorporeal Membrane Oxygenation (ECMO) can be vital in patients with respiratory failure, ventricular failure or CV decompensation: many cases of successful resuscitation with ECMO after peripartum cardiac arrest have been reported in literature (1, 12).
Thrombotic and hemorrhagic events
Another important issue regards peripartum hemorrhage or thrombotic events, both frequent in pregnant patients with CVD. The management of thrombotic and hemorrhagic events in postpartum women requires a tailored approach based on the patient's risk factors and clinical presentation. For thrombotic events, the use of prophylactic anticoagulation is often recommended for women with additional risk factors, such as previous history of thrombosis, cesarean delivery, or obesity (13).
In addition, anticoagulation can influence delivery timing and safety of anesthesia, so the role of anesthesiologists is to coordinate the timing of anticoagulation therapy discontinuation (1).
Recommended anticoagulation strategies involve the use of subcutaneous unfractioned heparin or subcutaneous low-molecular-weight heparin (1).
For hemorrhagic events, early recognition and prompt intervention are pivotal, as sudden hemodynamic deterioration may occur in cases of postpartum hemorrhage (1, 14). According to Surbek et al. patients’ blood management in obstetrics should be carefully evaluated not only in the post-partum phase, but also in diagnostic and/or therapeutic interventions during pregnancy and during delivery (14). Uterine massage and administration of uterotonics such as oxytocin can be effective in reducing bleeding (1 ,14). If bleeding persists, surgical intervention such as uterine artery embolization or hysterectomy may be necessary and obstetric maneuvers should also be considered in addition to medications due to the systemic side effects of uterotonics (1). In cases of coagulopathy-related bleeding, transfusion of blood products such as packed red blood cells, fresh frozen plasma, and platelets may be necessary, along with administration of clotting factors such as prothrombin complex concentrate or recombinant factor VIIa (1).
Arrhythmias management
Most common arrhythmias involve premature atrial beats, premature ventricular beats, and sinus tachycardia (1, 7). Among the allowed drugs during pregnancy, we find metoprolol, propranolol, sotalol, verapamil, procainamide, flecainide and digoxin (1, 15). Electrical cardioversion and adenosine are allowed as well (1).
Conclusions
As discussed throughout the paper, AHA is fighting to improving maternal care before, during and after child delivery, endorsing a meticulous preoperative assessment, careful selection of anesthetic agents and close monitoring during the perioperative period. It becomes clear that effective anesthetic management of pregnant patients with CV disease requires a multidisciplinary approach involving obstetricians, cardiologists, and anesthesiologists. By adhering to the guidelines set forth in the AHA scientific statement, we can minimize the risks associated with anesthesia and surgery, improving maternal and fetal outcomes. However, it is important to note that each patient is unique, and individualized care strategies must be developed based on the patient's medical history and condition: at this aim, clinical sense should guide decision-making.
It is imperative to pay attention to the points raised by AHA experts in the management of pregnant women with CVD. Furthermore, we advocate the training of an increasing number of obstetric anesthesiologists with a particular sensitivity towards the management of CV acute issues.
Peer-review: Internal
Conflicts of interest: None to declare
Authorship: All authors have participated in manuscript design and drafting. All authors read and approved the final version.
Funding: None to declare. The authors have not declared a specific grant for this work from any funding agency in the public, commercial or not-for-profit sectors.
Acknowledgement: The authors thank Dr. Luis Esse for providing valuable insights on clinical and scientific subjects.
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

