Comparative study of percutaneous transvenous mitral commissurotomy using ACCURA balloon in juvenile vs adult rheumatic mitral stenosis
ORIGINAL RESEARCH ARTICLE
Comparative study of percutaneous transvenous mitral commissurotomy using ACCURA balloon in juvenile vs adult rheumatic mitral stenosis
Article Summary
- DOI: 10.24969/hvt.2023.398
- CARDIOVASCULAR DISEASES
- Published: 28/06/2023
- Received: 25/04/2023
- Revised: 11/06/2023
- Accepted: 12/06/2023
- Views: 5066
- Downloads: 4131
- Keywords: mitral stenosis, adult, juvenile, percutaneous transvenous mitral commissurotomy, mitral valve area, outcomes
Address for Correspondence*: Amulya Cherukumudi, Department of Cardiothoracic Surgery, Sri Jayadeva Institute of Cardiovascular Sciences, Bangalore, India E-mail : amicool91@gmail.com
ORCID: 0000-0001-5067-1126
Sunil Kumar Kondethimmanahally Rangaiah1a, Amulya Cherukumudi1b*, Parvat Kumar Dash2, Banajith Barooah3
1aDepartment of Cardiology and 1bDepartment of Cardiothoracic Surgery, Sri Jayadeva Institute of Cardiovascular Sciences, Bangalore, India
2Hi-Tech Medical College, Bhuvaneshwar, Odissa, India
3Department of Cardiology, Sri Sathya Sai Institute of Higher Medical Sciences, Whitefield, Bangalore, India
Abstract
Objective: Mitral stenosis (MS) is rarely seen in children and adolescents but is not uncommon in developing countries where rheumatic fever is still endemic. Rheumatic MS in India commonly affects children and young adults less than 20 years old (juvenile mitral stenosis). Although percutaneous transvenous mitral commissurotomy (PTMC) using the ACCURA balloon catheter has been shown to be safe and effective technique in large series of adult patients, reports of this technique in children are scarce.
In our study, we aim to evaluate the immediate and early follow-up results of PTMC in 50 patients of rheumatic MS age ≤ 20 years and compare the same with those of the patients aged > 20 years.
Methods: Fifty consecutive patients aged ≤ 20 years with symptomatic rheumatic MS who met the inclusion criteria and whose valves are suitable for PTMC formed the cases, another 50 consecutive patients aged > 20 years with similar characteristics formed the control group. PTMC was done for both the groups as per the standard protocol and hemodynamic and echocardiography parameters were noted. Appropriate statistical tests were used to compare these data.
Results: The juvenile group had more often severe MS than adult patients at baseline [mitral valve area (MVA) 0.77(0.16) cm2 vs. 0.86(0.15) cm2, p<0.0069]. Atrial fibrillation was rare in juvenile patients (2%). Following PTMC, when absolute MVA was compared between the two groups, there was no significant difference, but when the post-PTMC MVA was indexed to body surface area, the juvenile group had statistically significant increase in indexed MVA as compared to adults [1.28 (0.30) cm2/m2 vs. 1.06 (0.26) cm2/m2, p<0.0001]. The same significant gain in indexed MVA was maintained at 6 months follow-up in juvenile patients as compared to adults (p<0.001). Juvenile patients also had significantly higher baseline invasive hemodynamic parameters like mean mitral valve gradient [23.44 (8.14) mm of Hg vs. 19.02(5.79) mm of Hg, p<0.002], mean PAP [50.92 (19.16) mm of Hg vs. 40.94 (11.82) mm of Hg, p<0.002] and mean pulmonary vascular resistance index [8.99 (7.29) U/m2 vs. 5.61 (4.30) U/m2, p<0.006] when compared to adult patients. Invasively measured mean left atrial pressure and mean pulmonary capillary wedge pressure were also high in juvenile patients than in adult patient but not statistically significant.
Conclusion: Juvenile patients had severe mitral valve disease with severe pulmonary arterial hypertension at presentation, both echocardiographically and hemodynamically than adult patients. Juvenile patients had significantly better immediate echocardiographic and hemodynamic benefits following PTMC than adult patients, and this was observed even at 6 months following the procedure. PTMC is safe and effective in juvenile rheumatic MS. It provides better immediate results in juvenile patients than in adults.
Key words: mitral stenosis, adult, juvenile, percutaneous transvenous mitral commissurotomy, mitral valve area, outcomes
Introduction
Rheumatic heart disease is a chronic manifestation of rheumatic carditis, which occurs in 60 to 90% of cases of rheumatic fever (1). Although all of the cardiac valves may be involved by this rheumatic process, the mitral valve is involved most prominently resulting in valvular regurgitation, stenosis or both (2).
Acute rheumatic fever is a rare disease in the very young; only 5% of first episodes arise in children younger than age of 5 years and the disease is almost undiagnosed of in those younger than 2 years (3). Mitral stenosis (MS) is rarely seen in children and adolescents except in developing countries where rheumatic fever is still endemic (4).Rheumatic mitral stenosis in India commonly affects children and young adults less than 20 years old (juvenile MS) (5). MS is rarely seen in children and adolescents but is not uncommon in developing countries where rheumatic fever is still endemic (6). Rheumatic MS in India commonly affects children and young adults less than 20 years old (juvenile MS) (7). As described by Roy et al. (7), juvenile MS is an acquired form of rheumatic MS distinctly different from congenital MS. Juvenile rheumatic MA develops rapidly after the attack of acute rheumatic fever with considerable commissural fusion, little or no calcification and severe pulmonary venous and arterial hypertension (7, 8). Valves are pliable, hence quite amenable to balloon valvotomy. Moreover, there exists an issue of the availability of a suitable valve size for a smaller body surface area (BSA) in juvenile patients, when the surgical option is considered.
Although percutaneous transvenous mitral commissurotomy (PTMC) using the ACCURA balloon catheter has been shown to be safe and effective technique in large series of adult patients (9), reports of this technique in children are scarce. ACCURA balloons are less expensive than other systems (Fig. 1).
In this study, we aim to evaluate the immediate and early follow-up results of PTMC in 50 patients of rheumatic MS aged ≤ 20 years and compare the same with those of the patients aged > 20 years.
Methods
Study design and population
It was a single-center prospective observational study performed in Sri Sathya Sai Institute of Higher Medical Sciences, Bangalore, India. Patients admitted for management of symptomatic severe MS in the center over a duration of 3 years were divided into groups of juvenile and adult MS. Fifty consecutive patients aged ≤ 20 years with symptomatic rheumatic MS who met the inclusion criteria and whose valves are suitable for PTMC formed the cases (juvenile MS), another 50 consecutive patients aged > 20 years with similar characteristics formed the control group (adult MS). Those patients with presence of any factor which by itself is a contraindication for PTMC, patients with redo PTMC or those who underwent OMC/CMV in past, those c-existing significant aortic valve disease, presence of organic tricuspid valve disease, those with severe left ventricular dysfunction, associated congenital heart disease, those with NYHA class IV symptoms and pregnant women were excluded from the study.
Written informed consent was obtained from all the subjects before the enrollment in the study. The study protocol was approved by the Institutional Ethical committee.
Clinical examinations and echocardiography
Clinical history was recorded and clinical evaluation was done for all the selected patients as per protocol, including age, sex, NYHA class, body surface area (BSA), electrocardiographic parameters: rhythm, atrial fibrillation, left atrial and biatrial enlargement. Routine pre-procedure transesophageal echo was done for all patients ≥30 years of age and those in atrial fibrillation, with past history systemic thromboembolism, in heart failure or evidence of severe right ventricular dysfunction on transthoracic echocardiogram, to rule out left atrial (LA) appendage clot. The following variables were assessed by echocardiography: chambers size, mitral regurgitation (MR), left ventricular end-diastolic volume, left ventricular end-systolic volume, ejection fraction (EF), mitral valve area (MVA), pulmonary artery systolic pressure (PASP), and mitral valve gradient (MVG). We assessed echocardiographic parameters pre- and post-procedure, and at 6-month follow-up echocardiography.
Percutaneous transvenous mitral commissurotomy
The procedure was performed via a femoral approach with a 9F sheath in the vein and a 5F sheath in the artery. 3000 U heparin is administered. Then right heart catheterization was performed. Transseptal catheterization was performed via a standard Brockenbrough procedure using right anterior oblique and left anterior oblique views. Next, a coiled-tip guidewire was placed into the LA through the Brockenbrough sheath. The ACCURA balloon catheter (Fig.2) was advanced over the coiled-tip wire. Once the balloon catheter had crossed the interatrial septum, the catheter formed a loop with the tip facing toward the mitral valve orifice (Fig 3).
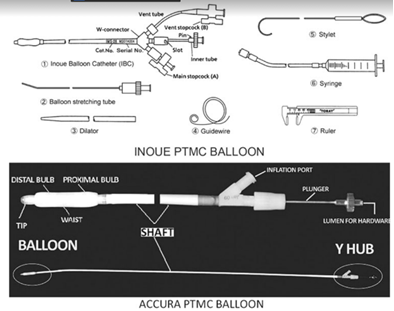
Figure 1. Diagrammatic representation of ACCURA balloons(vendor details- courtesy—Toray
Industries,Tokyo, Japan http://www.torayusa.com/ medical/ibpd.htm
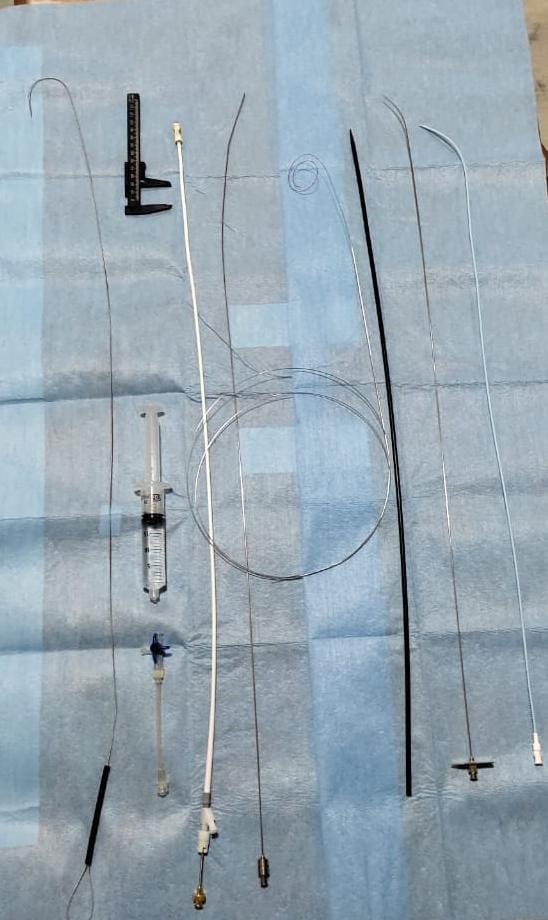
Figure 2. ACCURA balloon with the various components used in our study
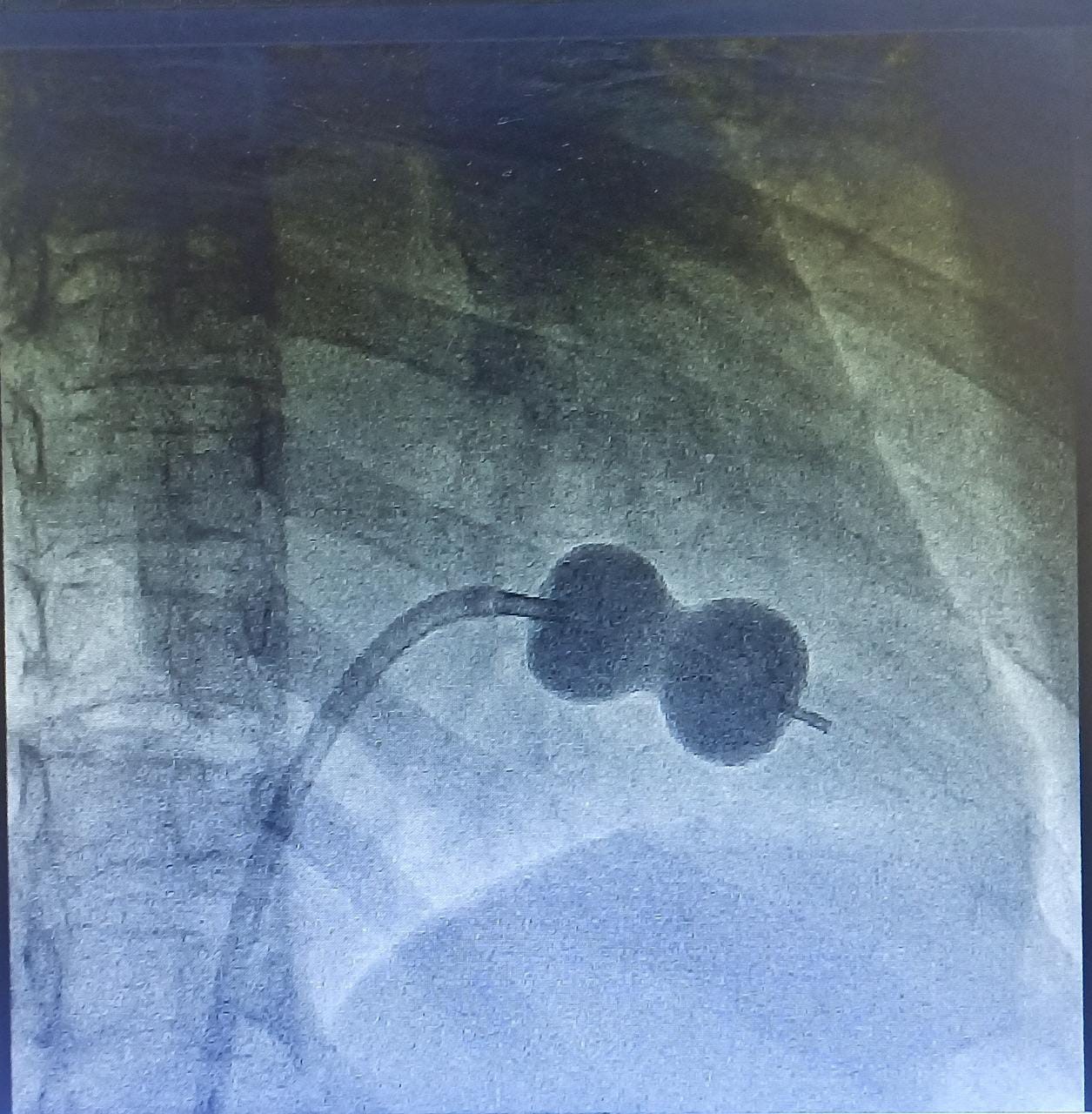
Figure 3. Fluoroscopic images of the ACCURA balloon across mitral valve
Alternately, stylet was used to advance the balloon in left ventricle. Once the balloon catheter had been inserted into the left ventricle, the distal portion of the balloon was inflated with contrast media and the catheter was then pulled until resistance was felt, following which full dilatation of ACCURA balloon was done.
After each dilatation, left atrial (LA) pressures were obtained. If the pressure did not drop, the balloon size was increased in 1-mm increments until the pressure decreases or substantial worsening of mitral regurgitation (MR) occurred. In addition, 2-dimensional echocardiographic observations were performed after each dilatation. To assess mitral valve orifice area (MVOA) If 1 of the 3 following events is encountered:
1. Increase in the MVOA > 1.5 cm2, without increase In MR more than Grade I and LA mean pressure of < 18 mm Hg
2. Occurrence of significant MR, or
3. Substantial splitting of the commissure; further dilatation were not performed
The results of PTMC were assessed using Wilkins score (10). We recorded LA pressure, MVOA left ventricular end-diastolic pressure (LVEDP), pulmonary vascular resistance index (PVRI), balloon size, number of dilatations, and contrast volume used to inflate balloon.
Statistical analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 15 (IBM Corp., Armonk, N.Y., USA).The discrete qualitative variables such as frequencies of different types of diseases among males and females proportions were analyzed using the chi-square test. Continuous variables were compared using independent-samples t-test. Independent means were compared with ANOVA test. P-value of<0.05 was considered significant.
Results
There were a total of 100 study participants, of which 50 were in the juvenile group and 50 were in the adult group. The age of subjects in juvenile group ranged from 8 years to 19 years. The mean was 14.7 (2.6) years (Table 1). The age of subjects in the adult group ranged from 21 years to 55 years. The mean age was 32.0 (8.5) years. In juvenile group 54 % (27) were males and 46% (23) were females while adult patients, 28% (14) were males and 72% (36) were female subjects.
|
Table 1. Baseline clinical characteristics of cases and controls |
|||
|
Baseline clinical characteristics |
Juvenile group (n=50) |
Adult group (n=50) |
p |
|
Age, years, mean (SD) |
14.7 (2.6) |
32.0 (8.5) |
<0.001 |
|
Males, n(%) |
27 (54) |
14 (28) |
|
|
Females, n(%) |
23 (46) |
36 (72) |
|
|
BSA, m2 |
1.25 (0.25) |
1.62 (0.37) |
<0.001 |
|
NYHA functional class, n(%) Class II Class III |
48 (96) 2 (4) |
50 (100) _ |
NS
|
|
Electrocardiographic variables |
|||
|
Sinus rhythm, n(%) |
49 (98) |
46 (92) |
? |
|
Atrial fibrillation, n(%) |
1 (2) |
4 (8) |
|
|
Left atrial enlargement, n(%) |
17 (34.7) |
36 (78.3) |
|
|
Biatrial enlargement, n(%) |
32 (65.3) |
10 (21.7) |
|
|
Data are presented as mean (SD) and n(%) Chi-square and t test for independent samples |
|||
|
Table 2. Propensity score matching of baseline characteristics |
|||
|
Variables |
Juvenile (n=50) |
Adult (n=50) |
p |
|
Men |
27 |
14 |
0.0041* |
|
NYHA >II |
2 |
0 |
0.921 |
|
EF <40% |
5 |
12 |
0.001* |
|
MVOA < 1.5 cm2 |
14 |
9 |
0.067 |
|
AF |
4 |
16 |
0.083 |
|
AF – atrial fibrillation, EF – ejection fraction, MVOA – mitral valve orifice area |
|||
The BSA in the juvenile group ranged from 0.8m2 to 2.1m2. The mean body surface area was 1.25 (0.25)m2. In adult patients, the body surface area ranged from 1.1m2 to 2.5 m2. The mean BSA was 1.62(0.37).
Overall 96% (48 patients) of subjects in juvenile group were in NYHA functional class II on presentation and 4% (2) were in functional class III. All the patients in the adult group were in NYHA functional class II on presentation.
In juvenile group, 98% of subjects were in sinus rhythm, while 2% were in atrial fibrillation. Similarly, 8% of adults were in atrial fibrillation. The adult group had more LA enlargement as compared to juvenile group.
The Table 2 shows that after matching baseline characteristics, adult patients with MS more often had left ventricular dysfunction and atrial fibrillation as compared to young patients (p<0.05 both).
Echocardiographic variables (Table 3)
A statistically significant initial gain in indexed MVA was maintained in juvenile group as compared to adult group at follow up echo after 6 months (p < 0.001). At follow up echo performed the 6 months, the mean indexed MVA in the juvenile group was 1.28 (0.30) cm2/m2 and in adults, it was 1.03 (0.27)cm²/m2.
In both groups mean MVA, MVG and PASP decreased after PTMCA and at 6-th month of follow up (p<0.05 for all).
|
Table 3. Comparison of pre-PTMC, post-PTMC and follow- up echocardiographic parameters in studied groups |
||||
|
PTMC ECHO parameters |
Juvenile group (n=50) |
Adult group (n=50) |
P* |
|
|
MVA, cm2 |
Pre |
0.77 (0.16) |
0.86 (0.15) |
0.0069 |
|
Post |
1.60 (0.30) |
1.68 (0.21) |
0.1244 |
|
|
Follow up |
1.57 (0.30) |
1.62 (0.26) |
0.3549 |
|
|
Indexed MVA, cm2/m2 |
Pre |
0.60 (0.13) |
0.53 (0.15) |
0.0139 |
|
Post |
1.28 (0.30) |
1.06 (0.26) |
0.0001 |
|
|
Follow up |
1.28 (0.30) |
1.03 (0.27) |
<0.001 |
|
|
Mean MVG, mm of Hg |
Pre |
24.02 (8.49) |
21.6 (9.6) |
0.1849 |
|
Post |
7.0 (3.69) |
5.22 (2.01) |
0.0035 |
|
|
Follow up |
7.72 (3.79) |
7.32 (2.57) |
0.5385 |
|
|
PASP, mm of Hg |
Pre |
69.46 (25.03) |
58.48 (18.09) |
0.0136 |
|
Post |
38.52 (14.44) |
31.6 (9.76) |
0.0060 |
|
|
Follow up |
36.56 (10.88) |
36.58 (10.0_ |
0.9924 |
|
|
Wilkins Score |
|
9.40 (0.90) |
9.66 (0.92) |
0.157 |
|
Data are presented as mean (SD), *t –test for independent samples MVA- mitral valve area, MVG – mitral valve gradient, PASP – pulmonary artery systolic pressure |
||||
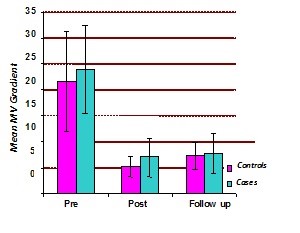
Figure 3. Mean mitral valve gradient (MVG) assessed by echocardiography in cases (juvenile) and controls (adult) before, after percutaneous transvenous mitral commissurotomy and at 6th month of follow-up
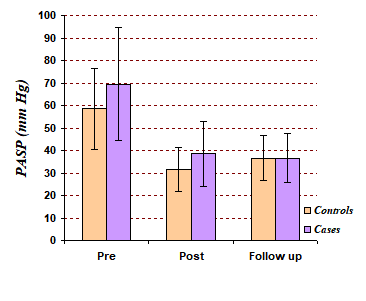
Figure 4. Mean pulmonary artery systolic pressure (PASP) assessed by echocardiography in cases (juvenile) and controls (adult) before, after percutaneous transvenous mitral commissurotomy and at 6th month of follow –up
MV gradient (Fig.3)
The MV gradient in juvenile group ranged from 10 to 40 mm of Hg, the mean MV gradient being 24.02 (8.49) mm of Hg. The MV gradient in the adult group ranged from 7 mm of Hg to 56 mm of Hg, with the mean gradient of 21.69.6 mm of Hg. Even though the mean pre PTMC MV gradient was higher in juvenile group than in adults, it was not statistically significant (p=0.1849). However, immediately after PTMC, there was a significant decrease in mean MV gradient in juvenile group as compared to adults (p= 0.0035). After PTMC, the mean MV gradient in juvenile group decreased from 24.02 (8.49) mm of Hg to 7.0 (3.69) mm of Hg (MV gradient reduction of 17.02 mm of Hg) and in adults, it decreased from 21.6 (9.6) mm of Hg to 5.22 (2.01) mm of Hg (MV gradient reduction by 16.4 mm of Hg).
On follow up echo at 6 months, there is no significant difference in mean MV gradient in juvenile group when compared to adults (p=0.5385). In juvenile group, it remained at 7.72 (3.79) mm of Hg, but in adults, there was an increase in mean MV gradient from 5.22 (2.01) mm of Hg after PTMC to 7.32 (2.57) mm of Hg at 6 months follow up.
PASP (Fig. 4)
The pre-PTMC PASP in juvenile group ranged from 35 mm of Hg 130 mm of Hg, with mean being 69.46 (25.03) mm of Hg. In the adult group, the pre PTMC PASP ranged from 35 to 105 mm of Hg with the mean being 58.48 (18.09) mm of Hg, showing that juvenile group had significantly higher PASP at presentation than the adult group (p=0.0136).
Immediately following PTMC, the PASP in the juvenile group decreased from 69.46 (25.03) mm of Hg to 38.52 (14.44) mm of Hg and in adult group, it decreased from 58.48 (18.09) mm of Hg to 31.6 (9.76) mm of Hg, which when compared between the groups, a statistically significant difference was observed (p=0.0060). However, on follow up echo at 6 months, there was no significant further drop in PASP in both the groups.
There was no significant difference in mean Wilkins scores of juvenile and adult patients. The mean Wilkins score of juvenile patients was 9.4 (0.90) and for adults, it was 9.66 to 0.92.
PTMC variables
The baseline mean LVEDP was higher in adults when compared to juvenile group (p<0.001) and no statistically significant difference was observed between juvenile and adult patients when post PTMC increase in LVEDP was analyzed.
The pre PTMC PVRI in juvenile patients was significantly higher than in adult patients (p 0.006). When compared, there was a trend towards significant drop in PVRI in juvenile patients when compared to adults (p= 0.067).
There was no statistically significant difference between the balloon size used for juvenile and adult group (p=0.231). The mean volume of diluted contrast used for balloon inflation for juvenile group was 23.48(1.43) mm and for adult group, the mean volume taken was 23.96 (1.65) mm. There was no statistically significant difference between the two groups when volume taken was considered (p=0.124).
The mean number of dilatations used in case of juvenile patients was 2.12(0.59) and in case of adults, it was 2.16 (0.76). Again there was no statistical difference between the groups (p=0.771). Overall, there was no difference between the juvenile and adult groups when balloon characteristics are taken into consideration. In other words, balloon characteristics did not influence the difference in outcome between the two groups.
Discussion
This study was aimed at analyzing the clinical, echocardiographic and hemodynamic parameters immediately before and after PTMC using ACCURA balloon in juvenile rheumatic MS patients and comparing these parameters with those in the adult patients aged > 20 years. We observed that there was a higher preponderance of males in the juvenile group, with a significant improvement in the mean index MVA, PASP and LVEDP when compared to the adult group.
Follow-up echocardiographic parameters at 6 months after PTMC were analyzed between the groups. The severity of various parameters at baseline and the extent of response immediately following PTMC was critically analyzed between the study groups, any differences with respect to complications of the procedure between the groups was studied.
The mean age of the juvenile group was 14.7 (2.6) years, whereas the mean age of adult group was a 32.0 (8.5) years (p<0.001). In the cohort studied by Bahl et al. (11), the mean age in juvenile group was 14.5 (5) years and in adult group, it was 32 (11) years, very much similar to present study. The average age in Fawzy et al. (12) study was also similar -juvenile group of 16.7 years and adult group of 33.7 years.
In the juvenile group, the male to female ratio was 1.1:1, a slight male preponderance in juvenile rheumatic MS was noted. Similar slight male preponderance was also noted by other authors as well. Cherian et al. (13) noted a male to female ratio of 1.3:1, while Kothari et al. (14) noted a ratio of 1.5:1.
Bahl et al. (11) who found a mean BSA of 1.3 (0.3) m2 in juvenile patients and 1.5 (0.3) m2 in adult patients. Fawzy et al. (12) reported a mean BSA of 1.42 m2 in juvenile group and 1.6 m2 in adult groups.
Most of the juvenile patients in our study were in the NYHA class II and III. In Cherian et al study (13), 25% of juvenile patients were in functional class II and 75% belong to functional class III and IV. In Fawzy et al. study (12), 90.4% of juvenile patients were in NYHA class III and IV and 87.8% of adult patients were in NYHA class III and IV.
Bahl et al. (11) have reported a pre-PTMC mean indexed mitral valve area of 0.53 (0.05) cm2/m2 and a post-PTMC mean indexed mitral valve area of 1.6 (0.15) cm2/m2 in juvenile group. In adults, they reported a pre-PTMC mean indexed mitral valve area of 0.47 (0.06) cm²/m2 and a post-PTMC mean indexed MVA of 1.3 (0.20) cm2/m2, like present study.
Mattos et al. (15) reported a pre PTMC mean mitral valve gradient of 15.3 (5.4) mm of Hg in juvenile group which decreased to 6.0 (2.5) mm of Hg after PTMC which was statistically significant. However, they have not compared with adults, unlike in the present study
Fawzy et al. (12) have also reported a higher hemodynamically measured baseline MVG in juvenile patients when compared to adults, which was similar to the findings of the present study.
Shrivastava et al. (16) also reported a significant decrease of mean MVG in the juvenile patients from 18.0 (6.0) mm of Hg to 6.0 (2.0) mm of Hg after PTMC (p <0.001). In Mattos et al. (15) study the mean MVG decreased from 21.7 (6.8) mm of Hg to 4.4 (3.0) mm of Hg after PTMC in juvenile patients (p < 0.001).
In Fawzy et al. (12) study, the mean PASP decreased from 48.0 (16.2) mm of Hg to 38.3 (14.5) mm of Hg after PTMC in juvenile patients whereas in adults it decreased from 48.5 (17) mm of Hg to 39.2 mm of Hg. Within the groups, the fall in pulmonary artery pressure after PTMC was statistically significant (p<0.0001) but when the two groups are compared and fall in pulmonary artery pressure following PTMC was considered, there was no significant difference unlike that observed in the present study.
Similarly, studies by Kothari et al. (14), Fawzy et al. (12) and Shrivastava et al. (16) showed a significant difference in the reduction in PVRI, LA pressure and pulmonary capillary wedge pressure in individual groups, but there was no difference between the groups, like the findings of our study.
Gamra et al. (17) defined procedural success as an index mitral valve area of ≥0.9 cm2/m2 with no severe MR after the procedure. Patil et al. (18) observed a procedural success of 100% in juvenile patients and 92% in adult patients, again emphasizing high procedural success in both the groups. In our study the mean MVA in juvenile group was 1.57 cm2 and in adults - 1.62 cm2 at 6-month of follow-up.
Study limitations
Our study has several limitations as:
1.Small sample size
2.Short follow-up period
3.Echocardiography is operator dependent, and a better modality of comparison is necessary to assess the outcomes.
Conclusions
Juvenile patients had severe mitral valve disease with severe PAH at presentation, both echocardiographically and hemodynamically than adult patients. Juvenile patients had significantly better immediate echocardiographic and hemodynamic benefits following PTMC than adult patients. The better immediate post-PTMC echocardiographic and hemodynamic benefits in juvenile patients was maintained at 6 months of follow-up. There was no significant difference between juvenile patients and adults, when procedural success rate and complications are compared.
Hence, PTMC is safe and effective in juvenile rheumatic MS. It provides better immediate results in juvenile patients than in adults.
Ethics: Informed consent was obtained from patients before all procedures. Study protocol was approved by institional Ethic Committee
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: S.K.K.R., A.Ch., P.K.D., B.B. equally contributed to study and manuscript preparation
Acknowledgement: None to declare
Funding: The study was performed using available resources at the institute, no external funds were sought/utilized
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

