Endovascular treatment with coil embolization of saccular celiac artery aneurysm: a case report
CASE REPORT
Endovascular treatment with coil embolization of saccular celiac artery aneurysm: a case report
Article Summary
- DOI: 10.24969/hvt.2023.399
- CARDIOVASCULAR DISEASES
- Published: 03/07/2023
- Received: 05/05/2023
- Revised: 24/06/2023
- Accepted: 24/06/2023
- Views: 5318
- Downloads: 3983
- Keywords: saccular aneurysm, celiac artery, endovascular coiling procedure, cardiac surgery, complications
Address for Correspondence*: Semen Chevgun, Kursk City Clinical Emergency Hospital, Pirogova Str., 14,
Kursk, 305035, Russian Federation Kursk City Clinical Emergency Hospital, Kursk, Russian Federation.
Email: schevgun@mail.ru Phon: +7 923 34 78 144;
Nikolai V. Bolomatov, Semen D. Chevgun, Maksim Yu. Gordov, Filip N. Klishevich, Andrey V. Alekseev, Bislan M. Dzhamalutinov, Kemran V. Abasov, Margarita V. Gerasimenkova
Kursk City Clinical Emergency Hospital, Kursk, Russian Federation
Abstract
Objective: Aneurysms of the celiac artery and its visceral branches are more often an incidental finding and can lead to serious complications. Many difficulties arise in matters of their treatment due to the rarity of occurrence.
Case presentation: This report describes the rare case of saccular celiac artery aneurysm in patient with severe cardiac comorbidities including history of cardiac surgeries. Celiac artery aneurysm was treated using the endovascular coiling procedure. We had coil dislocation during procedure, and 2nd attempt of coil embolization of aneurysm was successful. The dislocation into femoral artery was treated successfully. Immediate and 1st month follow-up data showed no evidence of recanalization and aneurysm enlargement and computed tomography angiography chowed correct position of coil.
Conclusion: Coil embolization is a safe and effective method for the treatment of celiac artery aneurysm in patients with severe comorbid conditions. One should be also prepared for possible technical difficulties that were overcome successfully and thus making minimal invasive approach in such patients effective.
Key words: saccular aneurysm, celiac artery, endovascular coiling procedure, cardiac surgery, complications
Introduction
Celiac artery aneurysms (CAAs) and its visceral branches are more often incidental findings and can lead to serious complications. Many difficulties arise in matters of their treatment due to the rarity of occurrence. CAAs account for only 3.6% to 4% of splanchnic artery aneurysms. Since the anomaly was first described in 1745 (1), fewer than 180 cases have been reported in the international medical literature. Early recognition and intervention are crucial, as the operative mortality rate associated with ruptured celiac artery aneurysms is 40%, compared to only 5% for non-ruptured aneurysms (2). Anatomically, CAAs are classified into two types. Type I CAAs located in the main trunk of the celiac artery. Type II CAAs located on the branches of the celiac artery (3).
CAAs have a strong tendency to rupture and can have fatal complications. The reported mortality after ruptured CAA approaches 100%. The overall reported risk for rupture appears to range from 10% to 20% (4-5). The majority of patients with CAA are symptomatic at presentation, although occult asymptomatic aneurysms are more likely to be diagnosed radiologically. Rupture occurs in approximately 5% of celiac trunk aneurysms ranging from 15 to 22 mm in diameter and in 50% to 70% of those that exceed 32 mm in diameter (6-7).
Treatment is strongly recommended for nonruptured celiac artery true aneurysms >2 cm, with a demonstrable increase in size or associated symptoms in patients of acceptable risk due to the risk of rupture. For aneurysms less than 2 cm, observation should prevail in stable asymptomatic CAAs or those in patients with significant medical comorbidities or limited life expectancy. For the elective treatment of CAA endovascular intervention is suggested if it is anatomically feasible, as well as open surgical. (8). Endovascular treatments include coil or glue embolization, percutaneous or open thrombin injection, and endovascular stent grafting. After endovascular intervention for CAAs, periodic surveillance with appropriate imaging studies is necessary. The potential for early or late failure, such as growth in sac size or leak, coil migration that would require reintervention, requires early and serial imaging follow-up (9-13).
This report describes the rare case of saccular celiac artery aneurysm treated with endovascular coiling procedure in a patient with severe cardiac comorbidity.
Case Report
A patient, a 66-year-old man, presented with pain in the right hypochondrium that was aggravated after eating.

Figure 1. Contrast-enhanced CT angiography: Saccular celiac artery aneurysm with thrombus along the wall (axial).
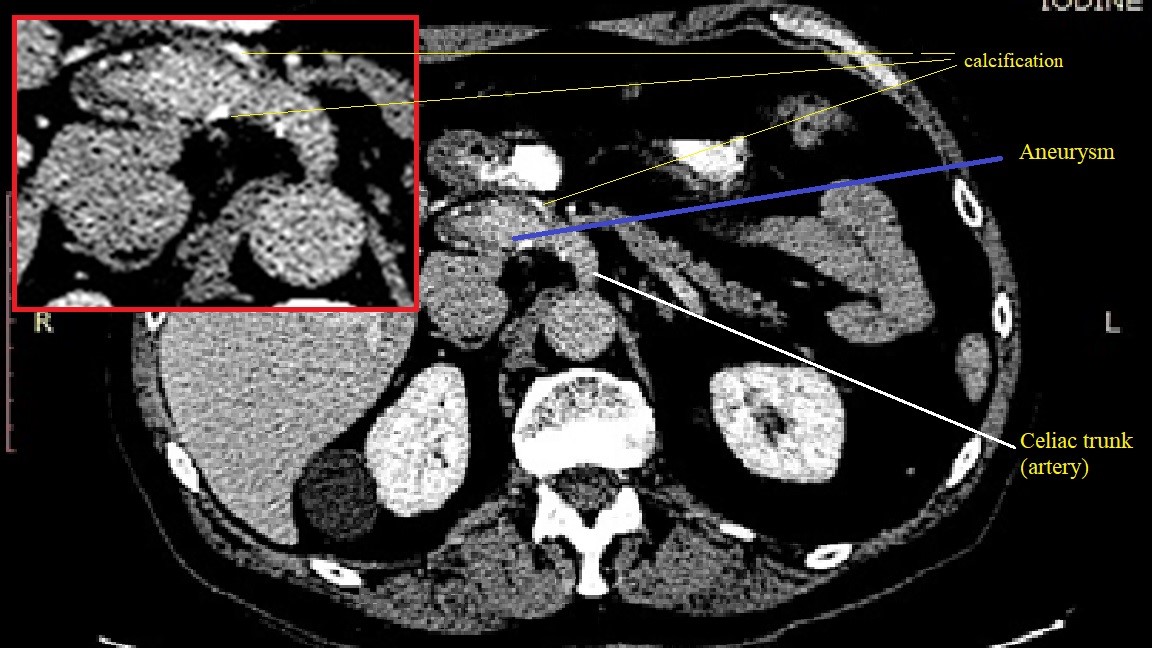
Figure 2. Non contrast-enhanced CT angiogarphy: Saccular celiac artery aneurysm with wall calcification (axial).
The symptoms had been presenting for about two months, and an abdominal ultrasound revealed a pancreatic cyst.
However, a computed tomography angiography (CTA) subsequently diagnosed an aneurysm of the celiac artery. The patient had several comorbidities including atrial fibrillation, hypertension, and dilated cardiomyopathy, for which he received treatment with beta-blocker - bisoprolol, statin - atorvastatin, mineralocorticoid receptor antagonist - spironolactone, angiotensin-converting enzyme inhibitor- perindopril, and new oral anticoagulant – dabigatran. He had history of mitral and tricuspid valve annuloplasty - performed in 2020. The patient is a smoker but does not have a history of alcohol abuse.
Computed tomography angiography
The patient underwent CTA. A saccular aneurysm of the celiac trunk measuring 29 x 18 x 21 mm was observed. The aneurysm walls exhibited signs of calcification and thrombosis (Fig. 1, 2).
Angiography data and coiling procedure
After general consultation with vascular surgeons, obtaining informed consent and preparing the patient, an endovascular coiling procedure was performed following angiography. Local anesthesia was administered, and the right brachial and right common femoral arteries were punctured with 6 Fr. introducers. Intra-arterial administration of 5000 IU of heparin was performed to prevent thrombus formation. The abdominal aorta and celiac artery were selectively catheterized. On the series of angiograms, a saccular aneurysm with dimensions of 12mm x 15mm x 22mm was observed at the ostium of the celiac artery. The diameters of the aneurysm neck and celiac artery were comparable (approximately 7mm). No visible pathology was found in the splenic artery, common hepatic artery, or left gastric artery (Fig. 3).
. 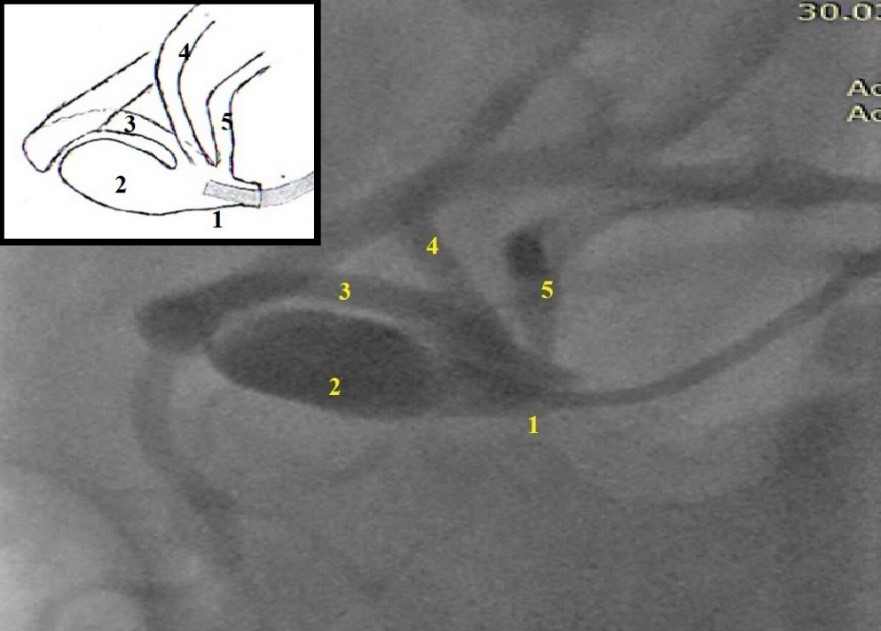
Figure 3. Selective angiography of celiac artery: 1 - celiac artery, 2- saccular aneurysm, 3- splenic artery, 4- left gastric artery, 5- common hepatic artery.
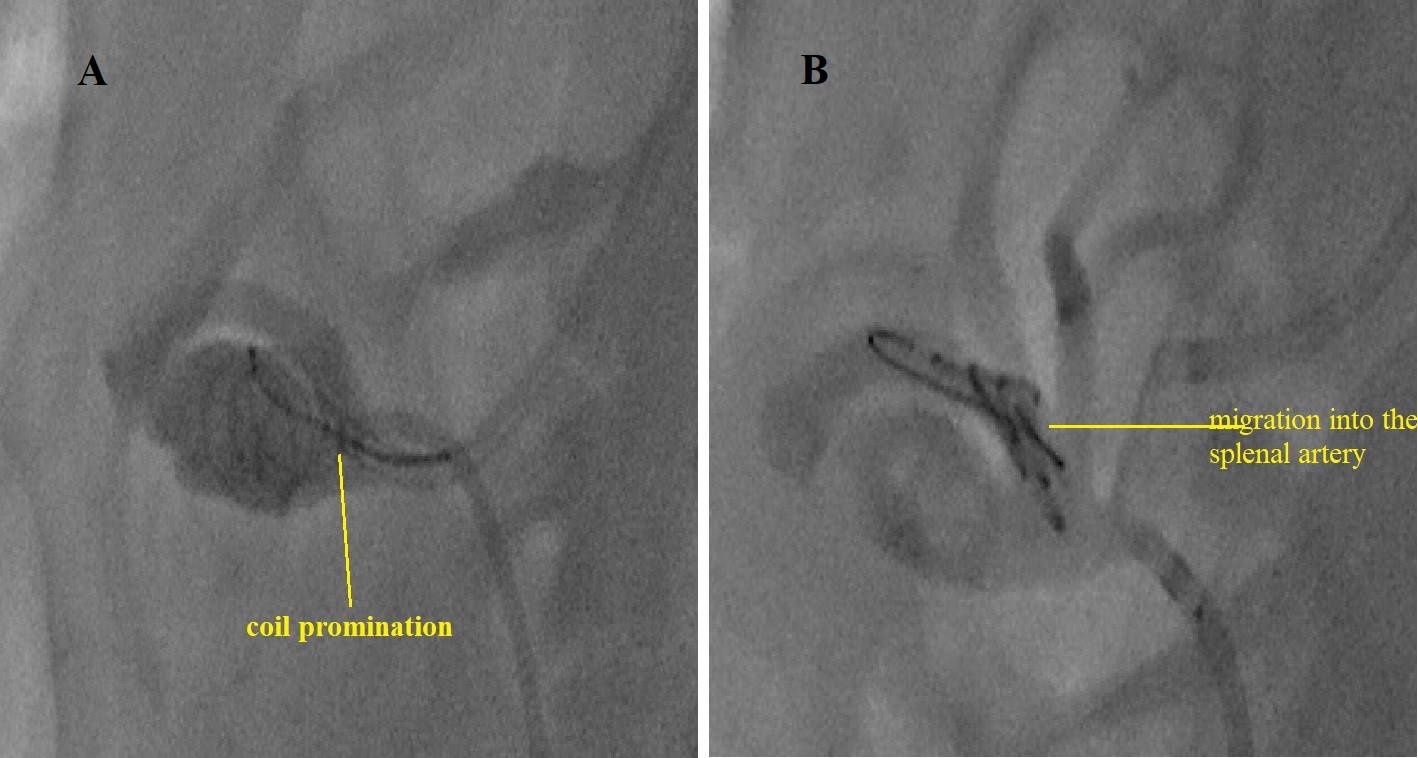
Figure 4. Coil dislocation into the celiac artery with followed migration into the splenic artery.
The dual access was selected for the treatment procedure using Judkins Right 5 and 6 French guiding catheters. Initially, Nester Embolization Coil with a size of 8 mm (Cook Medical, USA) was selected for embolization, which was inserted through the catheter. The placement of the coil caused difficulties and subsequently dislocation into the celiac artery with followed migration into the splenic artery occurred. There were multiple attempts to extract the displaced coil using the Amplatz Goose Neck Snare Kit 10 mm (EV3, Inc., USA) with the assistance of coronary balloon, but tightening the coil into the catheter led to its dislocation into the right deep femoral artery (Fig. 4).
For the second attempt at embolization, we chose a 6 mm Hydro Fill Helical coils (MicroVention, Inc., Terumo, USA), which we installed using a Headway 21 Microcatheter (MicroVention, Inc., Terumo, USA). After repeated angiography, we confirmed the occlusion of the aneurysm cavity, optimal position of the coils, and the absence of other branches damage (Fig. 5). At the final stage of the procedure, we removed the migrated coil from the deep femoral artery using contralateral access and the above-described Snare Kit 10 mm.

Figure 5. Selective angiography of celiac artery. Optimal position of the coils.
Follow-up data
Three days later, CT angiography revealed that the coils were adequately positioned within the aneurysm, the aneurysm cavity was thrombosed, and there were no leaks (Fig. 6). Patient was discharged on medical therapy he was prescribed before procedure.
After the 1-month follow-up, color Doppler ultrasound showed that the aneurysm remained stable with no enlargement or recanalization (Fig. 7). Unfortunately, the patient refused the proposed control CTA.
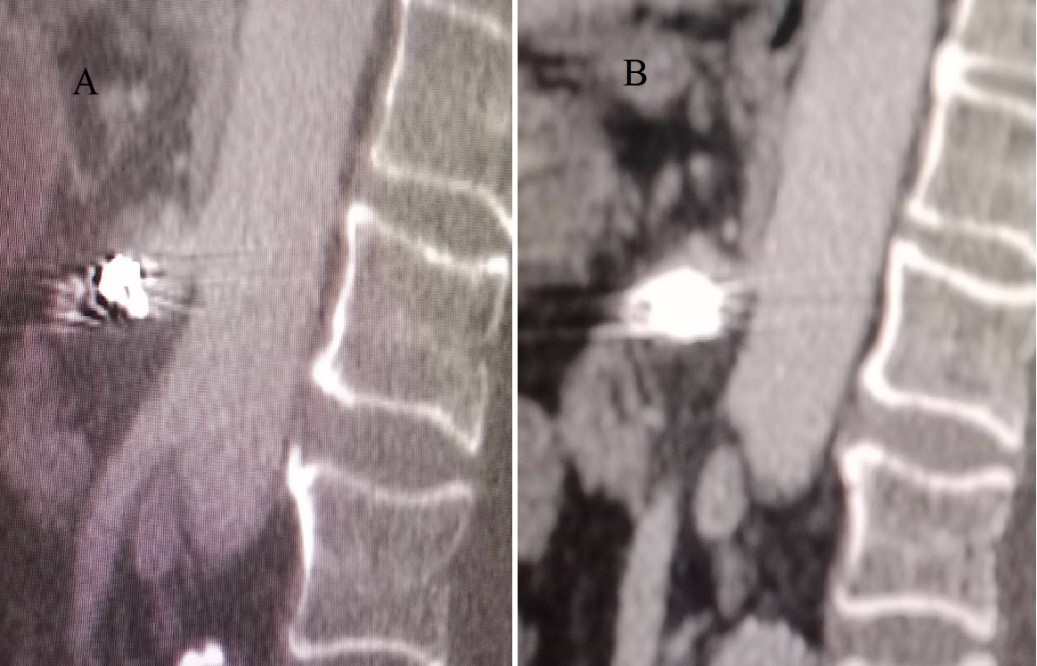
Figure 6. CT angiography showed an adequate position of the coils inside the aneurysm
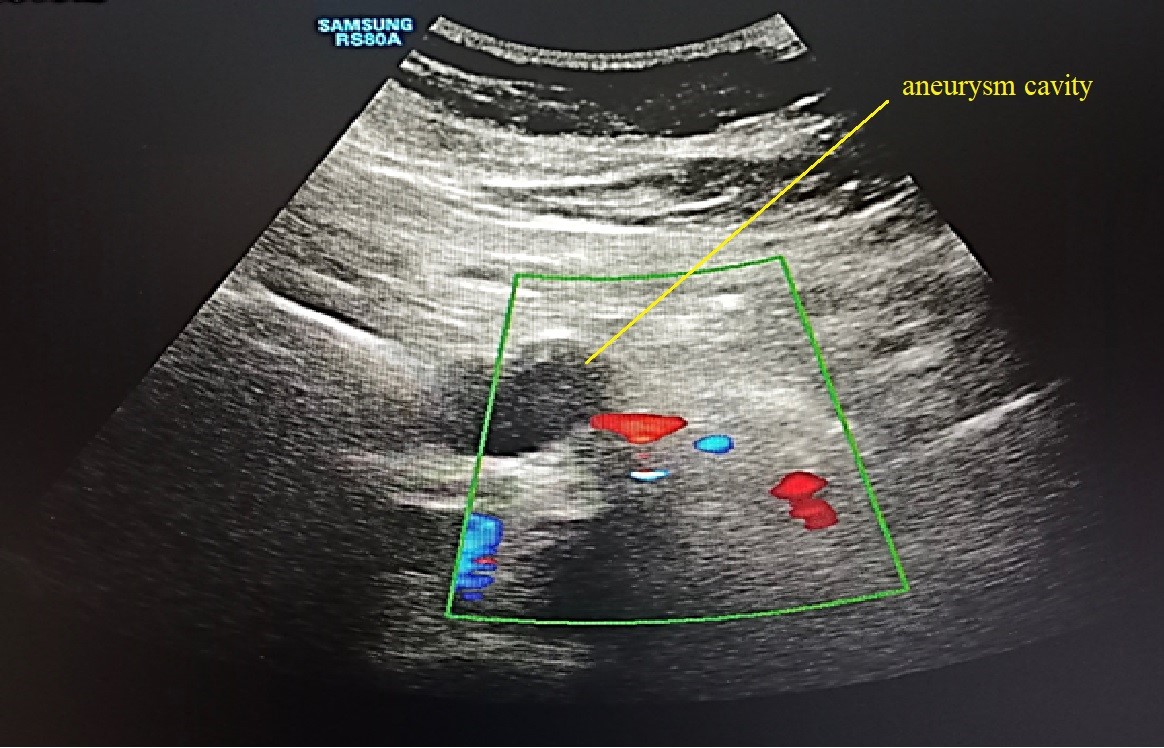
Figure 7. After 1-month of follow-up, color Doppler ultrasound showed stability of the celiac artery aneurysm cavity
Discussion
Endovascular treatment approaches have low procedural morbidity and mortality and are the most preferred for anatomically suitable visceral aneurysms (14). The recanalization rates after endovascular intervention were 18% and 30%, respectively, in two reported series (15-16). To assess the origin, shape, position, and anatomical features of CAAs, several methods of invasive and non-invasive diagnostics are recommended for visualization. Authors also noted that regular follow-up with duplex ultrasound or CT is necessary for patients with visceral aneurysms treated by embolization (17). Among other things, invasive diagnostics make it possible to clarify the quality of blood flow in terms of possible collateral branches, especially if a procedure is planned. In treating CAA, to determine the need for revascularization or sparing of the celiac artery and its branches, there is a necessity of evaluating the status of the superior mesenteric artery, gastroduodenal artery, and other relevant collateral circulation, which must be carefully documented on preoperative CT angiography or angiography. However, the usage of contrast medium diagnostics in the case of patients with renal insufficiency is variable.
In our case, in addition to the ultrasound study, which showed erroneous information (pancreatic cyst), we used contrast methods of study such as CT angiography and preoperative selective angiography. This made it possible to clarify the diagnosis and plan the endovascular intervention procedure. Also, the patient had severe cardiac pathologies and underwent cardiac surgeries in the past, as well as he has the need for anticoagulant therapy. It should be noted, that the therapy used before the procedure was left after. Endovascular coil embolization was performed in our case successfully, though we had coil dislocation during procedure into celiac artery, splenic artery and further into femoral artery, complication that was overcome with success. The 2nd attempt of coil embolization was successful. Control CT angiography after procedure showed correct placement of coil. Immediate and 1st month follow-up data showed no evidence of recanalization and aneurysm enlargement.
The advantages of endovascular interventions over open surgeries include rapid postoperative rehabilitation, reduced hospital stay, accessibility for patients with severe concomitant diseases, avoiding local complications, and multi-stage treatment.
Conclusion
Coil embolization is a safe and effective method for the treatment of celiac artery aneurysm in patients with severe comorbid conditions. However, this rare case of endovascular treatment for a saccular celiac artery aneurysm requires further observation, especially given the patient's serious cardiac pathology, which increases the risks of potential recanalization and subsequent aneurysm enlargement.
Despite the possible technical challenges during procedure for which the team must be prepared, we believe that the minimally invasive approach taken in this case was appropriate.
Take home message: Use of proper diagnostic methods to locate CAA and planning the invasive procedure, readiness to overcome possible technical difficulties during coil embolization are necessary for successful endovascular management of rare condition as CAA.
Ethics: Informed consent was obtained from patient before all procedures.
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: N.V. B., S.D.C, M.Yu.G., F.N.K, A.V.A., B.M.D., K.V.A, M.V.G. equally contributed to patient`s management and manuscript preparation
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

