Zero-fluroscopy ablation for cardiac arrhythmias: A single-center experience in Mexico
ORIGINAL RESEARCH ARTICLE
Zero-fluroscopy ablation for cardiac arrhythmias: A single-center experience in Mexico
Article Summary
- DOI: 10.24969/hvt.2023.400
- CARDIOVASCULAR DISEASES
- Published: 06/07/2023
- Received: 20/09/2022
- Revised: 17/06/2023
- Accepted: 17/06/2023
- Views: 5471
- Downloads: 4027
- Keywords: catheter ablation, fluoroscopy, tachyarrhythmias, electro anatomical mapping, intracardiac ultrasound
Address for Correspondence*: Ulises Rojel-Martinez, Arrhythmias and Pacing Unit, Cardiology Service, General Hospital “Dr. Eduardo Vazquez Navarro”, South Medical Center, Heath Secretary, Puebla, Mexico
E-mail : ulirm@hotmail.com
Ulises Rojel-Martinez1*, Arturo Enriquez1, Carlos De la Fuente1, Oscar Sanchez-Parada2, Ingrid Y. Lopez1, Alejandro Rodriguez-Garza1, Karla Bozada-Nolasco1
1Arrhythmias and Pacing Unit, Cardiology Service, General Hospital “Dr. Eduardo Vazquez Navarro”, South Medical Center, Heath Secretary, Puebla, Mexico
2Universidad Popular Autonoma Del Estado de Puebla (UPAEP) Facultad de Medicina, Puebla, Mexico
Abstract
Objective: Catheter ablation (CA) is a highly effective procedure for treating symptomatic tachyarrhythmias. However, the use of fluoroscopy, which is commonly employed in CA, exposes patients and medical personnel to ionizing radiation and its associated health risks. To address this concern, alternative techniques such as electro anatomical mapping and intracardiac ultrasound have emerged as viable options for performing CA without fluoroscopy. This study aims to describe the process and outcomes of mapping and ablation procedures performed without fluoroscopy in a Mexican electrophysiology laboratory.
Methods: Fifty-two patients with arrhythmias except atrial fibrillation were included in the study. The three-dimensional mapping system ENSITE Precision (Abbott) and intracardiac ultrasound, were used when the operator deemed it necessary. We assessed complications and immediate success of catheter ablation in our patients.
Results: A total of 52 patients were included in the study from January 2021 to July 2022of which 24 were men (42%) and 32 were women (57%). Only four patients received diagnostic three-dimensional mapping as a result of clinical tachycardia not being caused. An ablation of 52 arrhythmias substrates was performed with the following results: atrioventricular nodal reentry tachycardia in 20 cases (35.7%), typical atrial flutter in 16 cases (28.57%), atrioventricular re-entrant tachycardia mediated by concealed left accessory pathways in 4 cases (7%), manifest left accessory pathways in 3 cases (5.35%), manifest right accessory pathway in 2 cases (3.57%), right atrium tachycardia in 2 cases (3.8%), left atrium tachycardia in 3 cases (5.35%), right ventricular outflow tract ventricular extrasystoles in 2 cases (3.8%). The average duration of the procedure was 112.46 minutes. The immediate success rate was 100% in all ablated patients. An intracardiac ultrasound was used in 12.5% of cases.
Conclusion: Catheter ablation of arrhythmias without use of fluoroscopy in our study is found to be safe and immediate success rate of 100%. By eliminating the need for fluoroscopy, this research contributes to minimizing the health risks associated with ionizing radiation exposure during CA.
Key words: catheter ablation, fluoroscopy, tachyarrhythmias, electro anatomical mapping, intracardiac ultrasound
Introduction
Catheter ablation (CA) is one of the most effective procedures in the treatment of symptomatic tachyarrhythmias (1). The effectiveness rate for these procedures exceeds 90% in the treatment of different supraventricular tachyarrhythmias and more than 70% in some ventricular substrates (2). CA normally uses tools, such as the use of fluoroscopy that allows the operator to anatomically locate and manipulate the catheters inside of cardiac structures. One of the main disadvantages of exposure to ionizing radiation is that it leads to adverse health effects for patients and the medical crew. The risk of injury depends on deterministic factors (variable dosage) such as cutaneous injuries and congenital malformations. Likewise, it represents a risk in gestating patients, especially during the first trimester (3).
Currently, we have tools that allow the performance of CA without the use of fluoroscopy like electro anatomical mapping and intracardiac ultrasound. There is sufficient evidence of the safety and efficacy of such methods (4).
The goal of this study is to describe the process and the results obtained of mapping and ablation of diverse cardiac arrhythmias without fluoroscopy in our electrophysiology laboratory in Puebla, Mexico.
Methods
Study design and study population
This is a retrospective analysis of prospectively collected data.
All patients sent to our service between January 2021 and June 2022 with different tachyarrhythmias were included.
Patients 12 years of age and older, of both genders and arrhythmias like atrial tachycardia (AT), atrial flutter (AFL), atrioventricular nodal reentry tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT) mediated by manifest of concealed accessory pathway, premature joint complexes (PJC) and premature ventricular complexes (PVC) were included. Patients with atrial fibrillation or whose arrhythmia would not have been documented by a non-invasive method were excluded.
Consent was obtained from patients before procedures, and the Ethics committee approval of that study complies with Ethical Standards of the Declaration of Helsinki of 1975 and the 1989 amendments to the agreement issued by the Ministry of Health, published on January 26 1982 and the Scientific Committee was obtained. The patients were informed about the risks, possible complications, and benefits of the procedure in all cases.
Catheter ablation
We used local anesthesia and for some patients, sedation under the operator’s criteria. The three-dimensional mapping system ENSITE Precision (Abbott) and intracardiac ultrasound, were used when the operator deemed it necessary.
The anatomical reconstruction was performed with a high-density mapping catheter HD-Grid (Abbott), starting from the inferior vena cava until its joining the right atrium, right atrium and continuing to the superior vena cava. This was identified by the atrial electrogram's appearance. A full reconstruction of the right atrium was conducted focusing on the His-bundle area and the coronary sinus ostium (Fig. 1). Right ventricle reconstruction was performed only for the premature ventricular complex ablation. In cases where the arrhythmia originated in the left atrium or left atrioventricular annulus, transseptal puncture or aortic retrograde access were performed (Fig. 2). Mapping of uninvolved cavities was not performed. A decapolar catheter was placed into the coronary sinus in every case.
Once catheters were in place in these regions, a stimulation protocol was driven according to our center's practices to induce clinical tachycardia. Only in a few cases the use of dobutamine or atropine to induce arrhythmia were necessary.
The ablation catheters used were: TactiCath contact force catheter with DF curve (Abbot, USA) in 80% cases and Thermocool Smart Touch (Johnson&Johnson, USA), 4-millimeter Therapy Catheter with S or M curve (Abbot and Boston Sci, USA).
In cases where intracardiac ultrasound was required, an ACUSON P500 device was used.
In cases where access to the left atrium was necessary, a transseptal puncture was performed, via access through the right femoral vein, advancing using a 0.032'' SuperStiff 180 cm interchange guide until atrial extrasystoles were observed in the polygraph as indirect data of its location in the right atrium; the same way its location was corroborated with help from the intracardiac ultrasound. Afterward, there was a change to the transseptal puncture system (Mullins casing with Brockenbrough needle Abbot, USA); this was supported in the interatrial septum using the same imaging support.
Data collect
The following data was gathered from every patient: age, gender, comorbidities, and arrhythmia type. The following data was obtained: full-time procedure, therapy time (duration of ablation) use of intracardiac ultrasound, and immediate success/complications.
Therapy time was measured in seconds. The study's duration was quantified from the first femoral puncture to the removal of catheters from the same point. The procedure was considered successful once tachycardia was not reinduced, extrasystole ceased or the arrhythmic substrate (accessory means, slow means, bidirectional blockage of the cavo-tricuspid isthmus) disappeared under our center's stimulation protocols, with and without pharmacological effect.
Statistical analysis
We used descriptive statistics. The data are presented as mean (SD) and number percentage.
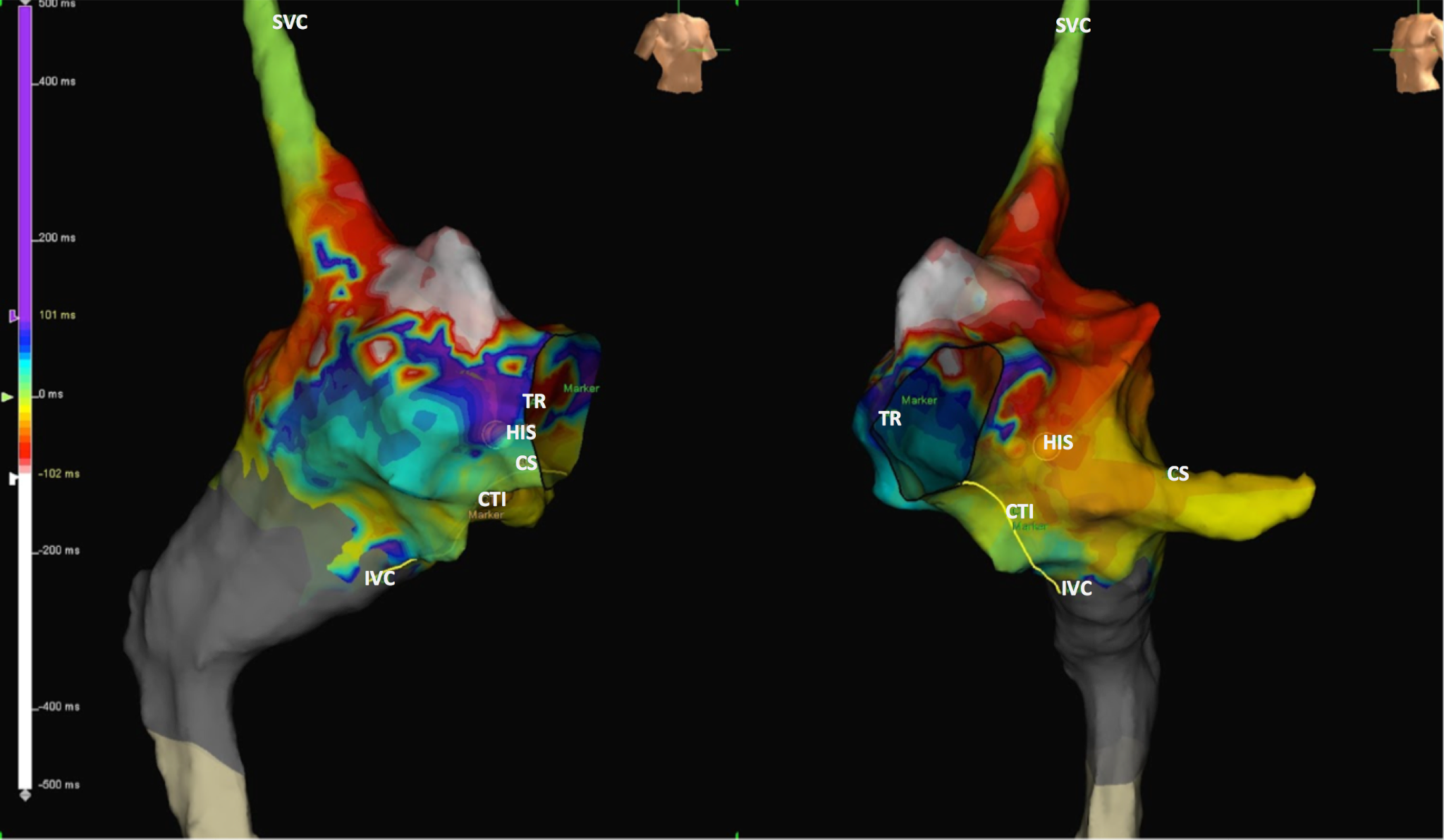
Figure 1. Three-dimensional mapping reconstruction of right atrium projecting right anterior oblique (left) and left anterior oblique (right) views both showing activation map of an atrial flutter dependent on the cavo-tricuspid isthmus (CTI). The zones corresponding to the inferior vena cava (IVC), His, coronary sinus (CS), tricuspid ring (TR) cavo-tricuspid isthmus (CTI), and superior vena cava are defined (SVC). Also, the line where the ablation is planned is drawn for two-directional blocking of the CTI
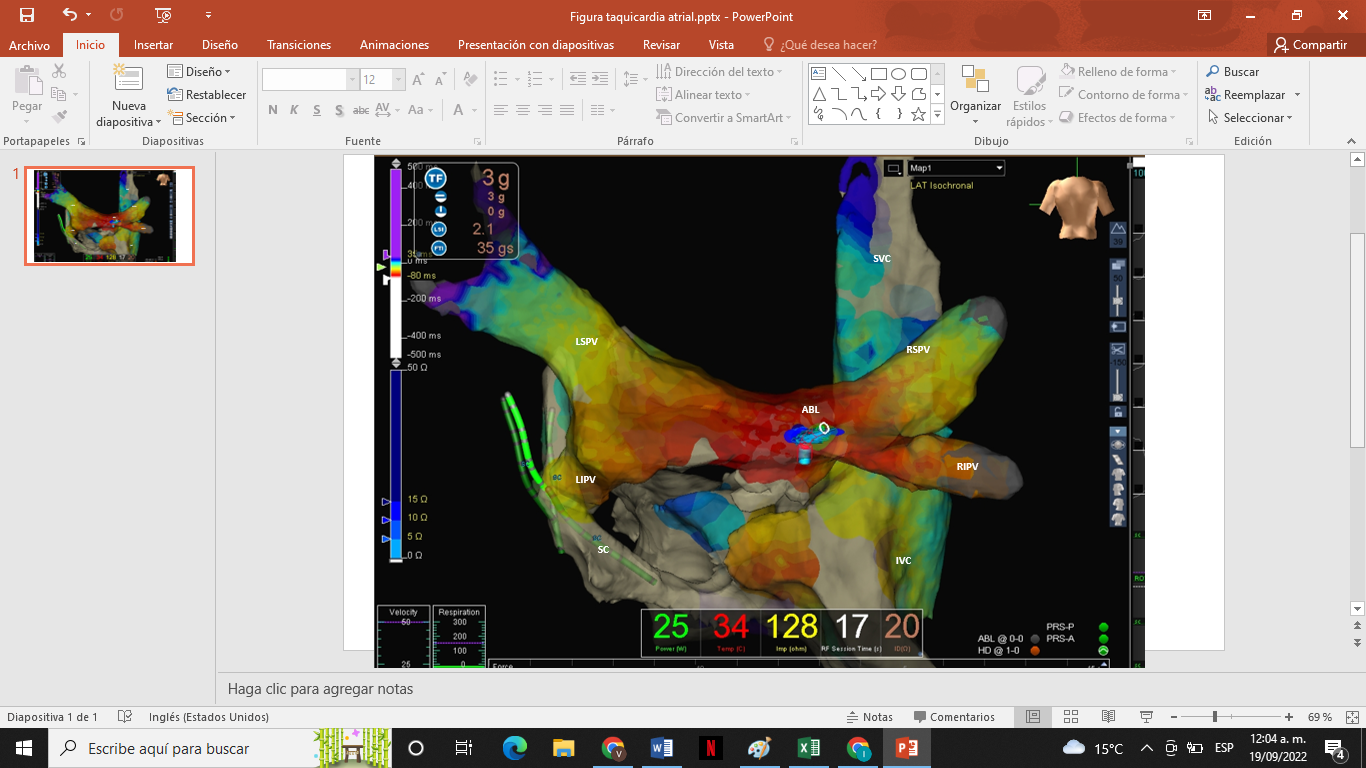
Figure 2.This is activation map. Three-dimensional mapping reconstruction of the right and left atrium addressed through transseptal puncture, for focal atrial tachycardia, located in the left atrium's posterior wall. Shown are the superior vena cava (SVC), inferior vena cava (IVC), right superior pulmonary vein (RSPV), right inferior pulmonary vein (RIPV), left superior pulmonary vein (LSPV), left inferior pulmonary vein (LIPV), coronary sinus CS), and the site of successful ablation (ABL)
Results
A total of 52 patients were included from January 2021 to July 2022 of whom 24 were men (42%) and 32 were women (57%) (Table 1). The mean age was 34 (18) years. Only four patients received diagnostic three-dimensional mapping as a result of clinical tachycardia not being caused. An ablation of 52 arrhythmias substrates was performed with the following results: AVNRT in 20 cases (35.7%), typical AFL in 16 cases (28.57%), AVRT mediated by concealed left accessory pathways in 4 cases (7%), manifest left accessory pathways in 3 cases (5.35%), manifest right accessory pathway in 2 cases (3.57%) right atrium tachycardia in 2 cases (3.8%), left atrium tachycardia in 3 cases (5.35%), right ventricle outflow tract ventricular extrasystoles in 2 cases (3.8%) (Fig. 3).
The average duration of the procedure was 112.46 minutes. The immediate success rate was 100% in all ablated patients. An intracardiac ultrasound was used in 12.5% of cases (Table 1). At the time of writing this document, no elapses were observed in any patient during the follow-up visits. No complications were observed.
|
Table 1. Baseline characteristics |
|
|
Patients, n |
56 |
|
Male, n (%) |
24 (42) |
|
Female, (%) |
32 (58) |
|
Age, years |
34 (18) |
|
Substrates, n |
52 |
|
AVNRT, n |
20 |
|
Typical flutter, n |
16 |
|
Left atrium tachycardia, n |
3 |
|
Right atrium tachycardia, n |
2 |
|
AVRT, n |
9 |
|
RVOT PVC |
2 |
|
Study time, min |
114.6 |
|
Intracardiac ultrasound, % |
12.5 |
|
Complications |
0 |
|
AVNRT – atrioventricular nodal reentry tachycardia, AVRT – atrioventricular reentrant tachycardia, RVOT PVC – right ventricular outflow tract premature ventricular complexes |
|
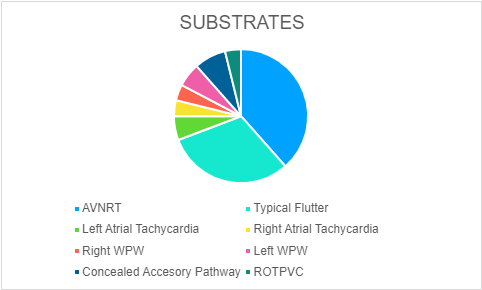
Figure 3. Percentage of arrhythmic substrates where it can be seen the most frequent diagnoses were intranodal reentry tachycardia and typical atrial flutter
AVNRT – atrioventricular nodal reentry tachycardia, WPW – Wolf-Parkinson-White syndrome, RVOT PVC – right ventricular outflow tract premature ventricular complexes
Discussion
The purpose of this study was to investigate the efficacy and safety of catheter ablation without the need for fluoroscopy use, in only one center in Mexico. This study included the highest number of patients to date with different arrhythmia substrates ablated without the use of fluoroscopy by one center in Mexico. The success rate of such procedures was the same for each operator.
The treatment of choice for symptomatic tachyarrhythmias is catheter ablation; however, despite its effectiveness, it carries some health risks both for the patient and the medical team. These risks are related to radiation exposure as well as the protection of radiological equipment used, like cancer or spinal cord injury (9, 10). Casella et al. (5) found that the radiological exposure of electrophysiologists is considerable, with doses ranging from 1 mSv (during non-complicated supraventricular paroxysmal tachycardia ablations) to 28 mSv (during ventricular tachycardia ablation), and even higher doses received by radiologists (13). Another disadvantage of this procedure stems from the type of patient in the room; considering body composition, dermatological conditions, age, or pregnancy, the procedure is not recommended during the first trimester of pregnancy with a class IIb recommendation (evidence level C) (5, 7, 11). The catheter ablation, without fluoroscopy used, is considered elective for expecting patients during the first or second trimesters and drug-induced tachycardia side effects and showing signs of low cardiac output (13).
Among the multiple benefits of using three-dimensional mapping are the accessibility to difficult-to-access areas and the higher precision that allows to minimize the risk of injury to adjacent healthy tissue, due to a better view of both vascular structures and cardiac cavities (6, 8, 13).
Multiple studies and meta-analyses have demonstrated that ablation using three-dimensional mapping is not-inferior to conventional electrophysiological study using fluoroscopy and sometimes the first one is even superior (10, 11). This also depends on the operator and staff's experience.
In our series notably was the absence of patients with atrial fibrillation, because cryoballoon ablation is first preferred in our center and we do not have proper experience yet to do it only with intracardiac ultrasound.
There are very few reports in Latin America; but just one prior of ours in Mexico (13) with similar results about lack of complications and high success rate. In conjunction, the data observed in our country is similar to other reported in worldwide series.
Perhaps the disadvantages of these techniques in our country are related to the high cost of equipment and systems required for conducting electroanatomical mapping. The variety of techniques, available catheters, and constantly developing technologies also represent the need of investing in education, training, and proper equipment maintenance. There are more and more papers that prove the aforementioned and it is to be expected that, shortly, the indications and contraindications of these techniques are defined in global clinical practice guides (12).
Study limitations
The small number of patients included in this study makes it difficult to definitively conclude the safety of the technique in different contexts not foreseen in this population, requiring further experience, especially in patients with structural cardiac disease with systolic left ventricular dysfunction, congenital heart diseases, and a higher number of complex arrhythmias like post-incisional arrhythmias, ventricular tachycardia substrate ablation, atrial fibrillation, and non-typical flutter.
Conclusion
This study proves the feasibility and safety of using three-dimensional mapping in ablating cardiac arrhythmias in our laboratory. It could be considered an alternative to reduce side effects associated with radiation exposure, as long as the proper infrastructure and possibility of solving any potential complications are in place. Likewise, it could become the ideal method of dealing with incessant arrhythmias during pregnancy. Three-dimensional mapping should be adopted soon by everyone who seeks to thrive in electrophysiology and arrhythmia ablation and should be included as an effective means in the work toward reducing unnecessary radiation exposure for medical imaging specialists, proposed by the FDA.
Ethics: Consent was obtained from patients before procedures, and the Ethics committee approval of that study complies with Ethical Standards of the Declaration of Helsinki of 1975 and the 1989 amendments to the agreement issued by the Ministry of Health, published on January 26 1982 and the Scientific Committee was obtained. The patients were informed about the risks, possible complications, and benefits of the procedure in all cases.
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: U. R-M., A.E., C.D.F., O.S-P., I.Y. L., A.R-G., K.B.-N. equally contributed to study and manuscript preparation
Acknowledgement: None to declare
Funding: The study was performed using available resources at the institute, no external funds were sought/utilized
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

