Surgical repair of ruptured infrarenal abdominal aortic mycotic aneurysm using superficial femoral vein graft: A case report
CASE REPORT
Surgical repair of ruptured infrarenal abdominal aortic mycotic aneurysm using superficial femoral vein graft: A case report
Article Summary
- DOI: 10.24969/hvt.2023.404
- Page(s): 377-381
- CARDIOVASCULAR DISEASES
- Published: 03/08/2023
- Received: 05/05/2023
- Revised: 26/07/2023
- Accepted: 27/07/2023
- Views: 4350
- Downloads: 3670
- Keywords: Aortic aneurysm, mycotic, femoral vein graft, rupture, case report
Address for Correspondence*: Tarun Shetty, Department of Cardiothoracic and Vascular Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry- 605006, India.
Mobile: +91 98200 96114 E-mail: tscvtsjipmer@gmail.com
Tarun Shetty*, Hemachandren Munuswamy, Aravind Kalyanasundaram
Department of Cardiothoracic and Vascular Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India.
Abstract
Objective: Intrathoracic or intra-abdominal mycotic aortic aneurysms (MA) are life-threatening infections with high morbidity and mortality. The objective of the present study is to report the treatment plan, roadblocks involved in management, pre-operative, and post-operative patient outcomes.
Case presentation: In this case report we have outlined in detail about the unusual presentation of a 58-year-old male patient with a ruptured mycotic abdominal aorta aneurysm. The pre-operative workup that led to the diagnosis of this uncommon condition and the use of a femoral vein as a bypass conduit to repair the infected diseased aorta was elucidated.
Conclusion: From our findings, we can state that early diagnosis using combination of clinical, laboratory, and radiological findings was proven to be effective. In such scenarios, early surgical intervention in the form of in-situ reconstruction with an autologous femoral vein as a conduit to repair was proven effective.
Key words: Aortic aneurysm, mycotic, femoral vein graft, rupture, case report
Introduction
In 1885, Sir William Osler first described the term ‘mycotic aneurysms’ in a 30-year-old man with infected aneurysms due to bacterial endocarditis. Till date, the term ‘mycotic aneurysms’ is a source of discussion among vascular surgeons for various reasons (1, 2).
In pre-antibiotic era, aneurysms were common. However, they are extremely rare to find nowadays. But, there is an increase in the incidence of aortic infections, which were reportedly high due to increase in drug abuse, intra-arterial invasive procedures, arteriography, and immunosuppression drugs (3). Such primary arterial infections are classified into 5 types based on the etiology and clinical findings as mycotic aneurysm, microbial arteritis, infection of a pre-existing aneurysm, post traumatic false aneurysm, and aortic infection from a contiguous organ with sepsis (4).
Among them, mycotic aneurysm or mycotic aortic aneurysm (MA) is generally caused due to an infection. In majority of the cases, it occurs either due to septic emboli (embolomycotic) or contiguous infection or bacteremic seeding or direct bacterial inoculation or mixed (5). MA also does not refer to fungal etiology, as majority of MAs are caused by bacterial pathogens (6).
In view of this, MA is also called as infected aneurysm. Infected aortic aneurysms are rare and accounts 0.5% - 1.3% of all aneurysms (7). The most common anatomical sites of MAs are abdominal aorta (~70%), thoracic aorta (~30%), and viscera (rare, <1%). Most common risk factors include pre-existing aneurysm, atherosclerosis, impaired immunity, antecedent infection, and arterial injury. MA have a male predilection (3:1, male to female) (8). MA is predominantly seen in patients over age 65 years, with a strong association with cigarette smoking, and diabetes mellitus. Clinically, atherosclerotic aortic aneurysms are largely identified in the infrarenal segment (85%), whereas aortic MAs in suprarenal portion of the aorta (8).
The microbiological spectrum of aortic MA is evolving depending upon the geographic conditions. Where, the common pathogen in Asian countries is Salmonella, while in Western countries consistently reported Pseudomonas aeruginosa (10%), Salmonella spp (15%), and Staphylococcus aureus (28%) as the most common pathogens (9). In recent years, S. Aureus and coagulase-negative staphylococci have emerged as the most common cause of aortic MA, accounting for ~50%-60% of cases. Earlier, gram-negative bacilli, especially non-typhoid Salmonella was the most common microorganism than staphylococci, but now they account for ~30% - 40% of cases (8, 10).
The present case report describes the unusual presentation of a 58-year-old male patient with a ruptured mycotic abdominal aorta aneurysm. Where, pre-operative workup, treatment plan, roadblocks involved, pre-operative, and post-operative patient outcomes are discussed in detail.
Case report
A 58-year-old male, known diabetic for 10 years on irregular medication was presented to our center with non-specific constitutional symptoms and bilateral lower limb claudication pain that had started 4 months ago, which aggravated over the last month. He also developed continuous high-grade fever 3 days prior to admission. Physical examination showed signs of local pain and tenderness. On laboratory examination, patients white cell count was 15 × 109/L, creatinine level was 62 μmol/L, platelet count was 165 × 109/L, hemoglobin level was 105 g/L, and his urea level was 4.1 mmol/L. Blood culture report was positive.
Further, contrast enhanced computed tomography (CECT) of the abdomen and bilateral lower limb was done in view of acute on chronic bilateral lower limb ischemia. It demonstrated a calcific diseased abdominal aorta with a saccular outpouching posteriorly in the infrarenal abdominal aorta of size 2.5cmx2.5cm, with periaortic inflammation and air foci (Fig. 1A and 1B). Diagnosis of infrarenal MA was made.
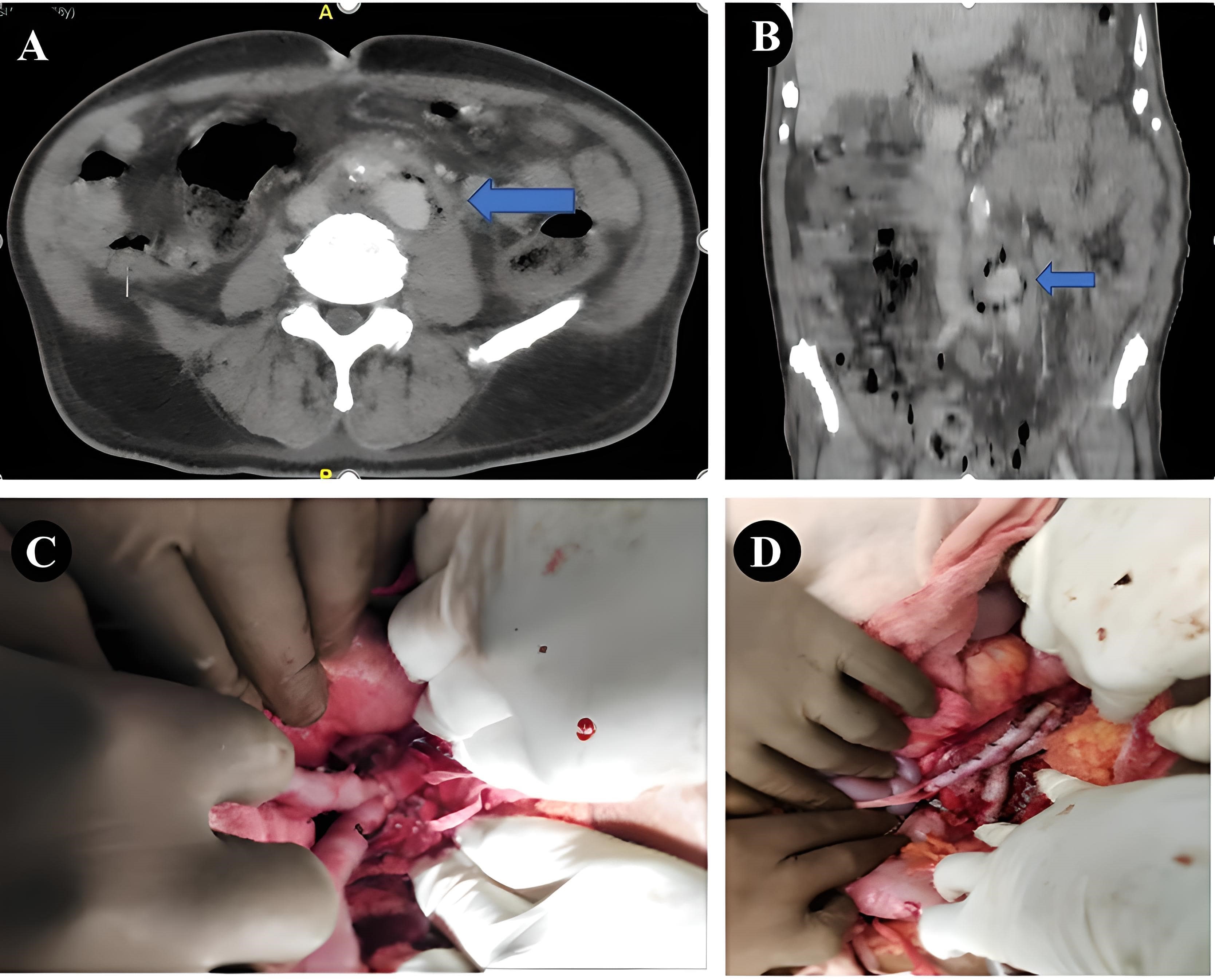
Figure 1. A and B –Contrast-enhanced computed tomography images of infra-renal abdominal aortic aneurysm with peri-aortic inflammation and air foci. C and D –Intraopreative view of proximal and distal anastomosis of the femoral vein graft.
The patient was taken up for emergency surgery and the infrarenal aorta was exposed via infra-umbilical midline laparotomy. Left retroperitoneal clot noted, indicating rupture. Saccular aneurysm 3cmx3cm was noted arising from the aorta-left common iliac junction. Diseased infrarenal aorta with the aneurysmal sac and the involved proximal part of the bilateral common iliac arteries and the surrounding necrotic tissue was excised. The left femoral vein was harvested from the left thigh along its entire length. The vein was cut into two unequal lengths depending upon the length required from the proximal aortic stump to the right and left common iliac, respectively.
The medial wall of the proximal end of the cut veins was sutured to make it a single lumen and a Y-graft was created. The proximal part of the graft was anastomosed to the proximal aortic stump in an end-to-end fashion and the distal limbs were anastomosed to the right and left common iliac respectively in an end-to-end fashion (Fig. 1C and 1D).
In the postoperative period, the patient developed abdominal distension on post-operative day 2. Ultrasound ruled out the fluid collection in the abdomen. The patient improved with conservative management. The patient developed left thigh swelling with lymphatic discharge from the suture line. The wound was managed with daily dressings and the lymphatic discharge resolved gradually. The biopsy report of the excised specimen was suggestive of an infectious/mycotic aneurysm. Blood culture on post-operative day 3 grew Acinetobacter Baumannii, sensitive to minocycline. The patient was started on intravenous minocycline and repeat blood cultures on post-operative day 8 were sterile. The patient was discharged on post-operative day 16. The patient was symptom-free with no signs of bilateral lower limb arterial or venous insufficiency, two months after surgery.
Discussion
Management of intrathoracic or intra-abdominal MAs remains challenging due to multiple dependent factors such as age, medical history, comorbidities, aneurysm type, location, pathogen type and its presentation; followed by antibiotic treatment and the type of surgical approach. All these parameters play a vital role in controlling MAs life-threatening infections, which are well known for their notoriety in causing high morbidity and mortality.
Due to non-availability of any algorithm or single investigation to diagnose MAs, the diagnosis is always made from combination of clinical, laboratory, and radiological findings. In view of this, a multi-disciplinary team approach will be highly beneficial for differential diagnosis and better outcomes. Differential diagnosis is highly recommended to differentiate the difference between infected aneurysms, inflammatory aneurysms, Lemierre syndrome, and Behçet disease, etc. (5).
As of date, surgery (open repair or endovascular therapy or hybrid) remains the mainstay of management, while medical management using antibiotics is supplementary. Due to limited supporting data and literature, exclusive medical management of the condition is not well accepted. In view of this, the choice of antimicrobial therapy is also specific, based on the identification and susceptibilities of the specific microorganism, depending upon the patients history of antimicrobial therapy. On the other hand, blood cultures are positive in only ~ 45% of patients with intraoperative tissue cultures were negative in one-third of patients; therefore, empiric therapy is often necessary. In almost all the patients, post-operative medical management is highly recommended from 6 weeks to 6 months, depending upon the patient’s condition. In exceptional cases, lifelong suppressive antimicrobial therapy is also considered. In aortic MA patients, use of antimicrobial therapy alone was associated with mortality rate of 65%-100%. Therefore, use of antimicrobial therapy alone for the treatment is considered only in patients who are unfit for surgery or who refuse surgery or endoscopic vacuum therapy (EVT), or palliative care (8).
In patients favorable to surgery, the choice and timing of an optimal procedure should be individualized and it is largely dependent on multiple factors such as rupture or impending rupture, presence of an entero-vascular fistula, response to initial antimicrobial therapy, single or multiple MAs, location of MA (intrathoracic or intra-abdominal), presence of gross purulence surrounding the MA or adjacent vertebral infection, and underlying comorbidities. In such patients, the options for management include open surgical resection with extra-anatomic revascularization or in situ reconstruction - EVT, or a combination of these procedures. Literature has reported affirmative results of resection of an infected aortic MA with in situ reconstruction, and this has become the procedure of choice in most of the patients with aortic MA (11–16).
The major advantages of in situ over extra-anatomic re-construction are as followed (17): (1) rifampin-soaked poly-ester or other conduits are readily available, especially in patients with rupture or impending rupture who require urgent surgical intervention; (2) for technical reasons, in-situ reconstruction is more versatile than extra-anatomic reconstruction for thoracic, suprarenal, or visceral artery MA; the latter requires renal and visceral artery revascularization; (3) there are fewer long-term complications, such as limb amputation, aortic stump rupture, and recurrent infection; (4) selected patients with aortoenteric fistulae have a lower risk of complications; (5) higher long-term survival rates have been achieved. The major theoretical disadvantage of in-situ reconstruction is the potential risk of reinfection because a foreign body material is used as an interposition graft in infected vascular tissue, often with surrounding purulence. The use of autogenous venous grafts or cryopreserved arterial allografts can reduce the risk of infection in these patients. In a nationwide study conducted by Quan et al. (18) both open and endovascular treated patients showed acceptable clinical outcomes. However, endovascular operative technique was considered to be favorable in terms of better outcomes. In a systematic review by Kan et al. (19) endovascular operative technique was reported to be the best possible alternative method in treating MA. An international multicentre study conducted by Ivika et al. (20) have also confirmed the biological grafts as a durable option with excellent infection resistance and good overall survival. Study by Daenens et al.(21) also proven the fact of in situ reconstruction of infected aortic grafts with the lower extremity deep veins as a safest alternative.
To conclude, infected aortic aneurysms do not present with characteristic findings, making them difficult to diagnose. In addition, the causative agent Staphylococcus Aureus or Salmonella and infection by Acinetobacter Baumannii are even rarer. In such scenarios, the autologous femoral vein as a conduit for bypass has many advantages in terms of its large caliber approximately the same diameter as the iliac artery, its robustness, and resistance to recurrent infection. After excision of the diseased tissue and infective material, in-situ reconstruction using an autologous femoral vein is also proven to provide an effective and durable treatment.
Conclusion
From our findings, we can state that early diagnosis using combination of clinical, laboratory, and radiological findings was proven to be effective. In such scenarios, early surgical intervention in the form of in-situ reconstruction with an autologous femoral vein as a conduit to repair was proven effective.
Ethics: Written informed consent was obtained from the patient before all procedures and for publication of this case
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: T.S., H.M., and A.K. contributed to the case management and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

