Evolution of cardiac pacemakers: a journey from Galvanic experiments to leadless pacemakers
HISTORICAL NOTE
Evolution of cardiac pacemakers: a journey from Galvanic experiments to leadless pacemakers
Article Summary
- DOI: 10.24969/hvt.2023.407
- CARDIOVASCULAR DISEASES
- Published: 09/08/2023
- Received: 03/08/2023
- Accepted: 04/08/2023
- Views: 14471
- Downloads: 4392
- Keywords: pacemakers’ history, external pacemaker, first pacemaker, leadless pacemaker
Address for Correspondence: Abay Bakytzhanuly JCS “National Research Cardiac Surgery Center”, Astana, Kazakhstan
Email:Bakytzhanuly@gmail.com
ORCID: 0000-0001-78167327; Facebook: abay.bakytzhanuly Twitter: @AbayBakyt
Abay Bakytzhanuly
JCS “National Research Cardiac Surgery Center”, Astana, Kazakhstan
Abstract
The development of cardiac pacemakers has a rich history spanning over two centuries, beginning with Luigi Galvani's discovery of the heart's response to electrical currents in the late 18th century. Paul Zoll's pioneering work in the 1950s introduced external pacemakers and defibrillators, followed by the first successful implantation of a fully implantable pacemaker in Sweden in 1958. Since then, pacemakers have undergone major improvements, including advancements in lead design and battery technology, as well as the development of telephony and microprocessors. Recent innovations have led to leadless pacemakers with wireless communication capabilities, transforming patient care and monitoring. This evolution has made pacemakers highly sophisticated devices that synchronize with the heart's rhythm, offering hope and improved quality of life for millions of individuals with cardiac rhythm disorders.
Key words: pacemakers’ history, external pacemaker, first pacemaker, leadless pacemaker
Cardiac pacemaker implantation is one of the common procedures in cardiology. Nowadays we have leadless pacemakers which can be implanted directly into the heart chamber. But in the beginning, the pacemakers were different. The history of pacemaker development is interesting and lasts over 200 years, improving the therapy of arrhythmias which saved many human lives.
In the late XVIII century, Luigi Galvani identified that passing an electrical current through the frog’s heart could cause its contraction. About 100 years later Guilliame de Boulogne saved a child’s life following the concept of Luigi Galvani by introducing an electrical current to the chest with a return electrode on the leg of the patient (1). In 1862, Walshe proposed the idea of a cardiac sympathetic nerve to restart cardiac arrest (2). Later the view of using electrical pacing to control the cardiac rhythm was announced in the late 19th century. John Alexander McWilliam, a British physiologist, in 1889 suggested the practical importance of “artificial excitation” of the heart (3). In the era of experiments, scientists tried to understand the ways of influencing cardiac rhythm. In the beginning, cardiac arrest was induced and restarted in different ways to understand the physiology of the heart. Thus, Pratt noted, in 1924, that cardiac rhythm can be regulated by the chemicals entering the venous blood and returning to the right atrium (4). Sloan produced cardiac arrest by vagal stimulation in animals with hypoxia and hypercapnia (5). According to Nathanson, carotid sinus pressure produced cardiac arrest for up to 15 seconds (6). Rothberger et al. in 1911 described that vagus nerve stimulation lead to cardiac arrest (7). According to Barber’s study, the heart restarted after cardiac arrest using cardiac massage and injection of adrenaline but only 33% survived (8).
In the 1930th an American physiologist, Albert Hyman, developed the external needle, the first pacemaker prototype, to restart cardiac contraction in animals (9). Electrical stimulation of the sino-atrial node during operation in humans was described by Sweet (10). According to the results of previous research works Wilfred Bigelow and John Callaghan studied the significance of electrical artificial pacemakers in cardiac arrest.
For a long time, cardiac massage and intraventricular injection of drugs were used with poor results. In 1949 Wilfred Bigelow (Fig. 1) was conducting experiments on performing cardiac surgery in dogs under hypothermia. During one of these experiments, he identified that he can restart the dog’s heart by stimulation with the transvenous catheter. Years later Wilfred G. Bigelow in collaboration with Canadian electrical engineer John Hopps (Fig. 2) and John Callaghan invented the first cardiac pacemaker (Fig. 3) (11, 12).
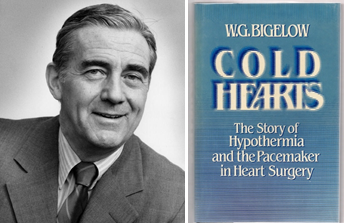
Figure 1. In the left panel Dr. Wilfred Gordon (“Bill”) Bigelow, emeritus professor of cardiac surgery University of Toronto, Ontario, Canada died from congestive heart failure on 27 March 2005 (11). The right panel is a book about his invention, Cold Hearts: The Story of Hypothermia and the Pacemaker in Heart Surgery (13).
(Reproduced from Dr Wilfred G. Bigalow. Bibliographical Sketch. Cardiovascular Science Collaborative Sopecialization. Copyright 2005©University of Toronto and
https://www.martinsquared.com/2019/09/11/p-comp-week-one-in-class-activity/)
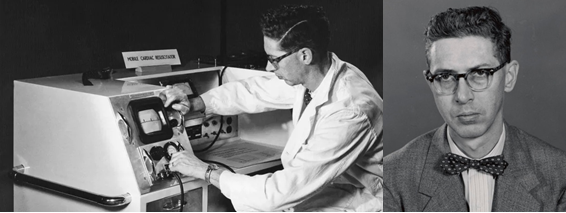
Figure 2. On the left John Hopps, a Canadian electrical engineer, tested the world’s first pacemaker. In the right panel is John Hopps.
(Reproduced from https://www.cbc.ca/2017/meet-the-canadian-engineer-who-casually-invented-the-pacemaker-1.4000971 and
https://recherche-collection-search.bac-lac.gc.ca/eng/home/record?app=fonandcol&IdNumber=4997379)
It was huge but a key instrument in developing electrophysiology. In 1984 he published a book about his invention, ``Cold Hearts: The Story of Hypothermia and the Pacemaker in Heart Surgery`` (13). The appearance of heartbeats was noted not only after the application of electrical stimulus but also after the mechanical effect in the region of the sinoatrial node (14).

Figure 3. First world’s external pacemaker. Invented by Wilfred G. Bigelow in collaboration with electrical engineer John Hopps and Dr. John Callaghan in 1950.
(Reproduced from https://www.cbc.ca/2017/meet-the-canadian-engineer-who-casually-invented-the-pacemaker-1.4000971)
Paul Zoll, an American cardiologist, was inspired by the research works of Wilfred Bigelow and John Callaghan to develop an external pacemaker. In 1952 he presented a method of cardiac stimulation in patients with intact chests. The electrodes were attached to the patient’s chest and 2-millisecond duration pulses with 100–150 volts passed across the chest which led to the cardiac construction (Fig. 4) (15). Since then the cardiac pacing practice spread rapidly and become “a standard procedure” in cardiology and cardiac surgery. However, it was not the kind of pacing that we used to know in the present day. The pacemaker had a huge generator with cables plugged into electrical spots and involved bedridden, basically sedated or unconscious patients. The pacing was performed with high voltage and caused painful chest muscle contractions. Later in 1956, Paul Zoll described a termination of ventricular fibrillation with an externally applied countershock (16). His alternating current shock became standard cardioversion-defibrillation but later was replaced by direct current shock. In collaboration with the chief engineer of Electrodyne Company, Alan Belgrad, Paul Zoll produced external monitored-automatic pacemakers with heart rhythm alarms and chest surface defibrillators. Because of his contribution to the development of cardiology, he was called “the father of modern cardiac therapy” (17).
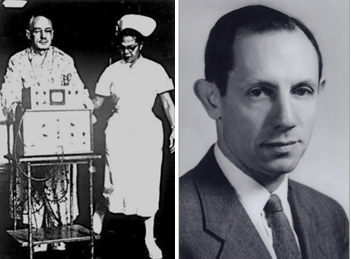
Figure 4. On the left: patient with external surface pacemaker accompanied by a nurse. On the right is a photo of Paul Zoll, “the father of modern cardiac therapy”.
(Reproduced from https://twitter.com/zollemsfire/status/626788517599932416/photo/1 and
https://alchetron.com/Paul-Zoll)
In the 1950s there was a great growth in cardiac surgery. Techniques of entering the heart, and correcting congenital defects with circulation stoppage had been developed. C. Walton Lillehei in that period was “an ascending star” in cardiac surgery at the University of Minnesota, Minneapolis. Nevertheless, despite successful correction of congenital defects, 10% of procedures were complicated with complete heart block. This took place because of conduction system damage during the cardiac surgery. Thus, there was a necessity for a temporary pacemaker for the period of conduction system repair. Invented by Paul Zoll’s transthoracic pacemaker was inappropriate because of the traumatic effect and pain after open heart surgery. Lillehei and his team created a special wire in which the distal tip was connected to the myocardium and the other end was connected to the external stimulator. This lead to less painful cardiac stimulation and no damage to the beating heart. On the 30th January 1957 first epicardial wire was implanted in 3-years old girls after Fallot’s tetralogy correction complicated by heart block. Afterwards, the patient survived and the conduction was restored. Nevertheless, they were problems like the external pacemaker’s huge size, especially for pediatric patients, hard to transport and dependency on the external electricity supply. In 1957 there was a two-and-a-half-hour blackout. The hospital had generator backup in its surgical suites and recovery area but not in the patient’s room. The young patient died. The next day Lillehei asked Earl E. Bakken, co-founder of Medtronic, to develop a better pacemaker. Later Bakken demonstrated an external wearable pacemaker with its battery (Fig. 5).
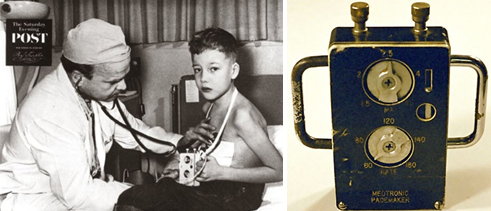
Figure 5. C. Walton Lillehei with a child. On the right: external portable pacemaker.
(Republished under CC-BY license rules from reference 19.)
In Sweden, in 1958, the first fully implantable pacemaker was fitted to Arne Larsson, the first human who received a fully implantable pacemaker. Arne Larsson was presented to the hospital with a complete atrioventricular block and had Stokes-Adam attacks for a half year. The pacemaker was invented by Rune Elmqvist and Ake Senning (Fig.6) (18). At that time the experiments were not finished but the patient's wife, Else Marie, pleaded with both scientists to implant the pacemaker. Finally, the scientists decided to perform the pacemaker implantation but without publicity. At the end of the working day when the operating room was empty, Ake Senning was implanted the first pacemaker in history with full components under the patient’s skin. Because of the procedure performed when the experiment was not finished the pacemaker’s generator worked only 8 hours. Later Senning commented on it that he damaged the output transistor or capacitance during the implantation procedure. The next morning Senning implanted another pacemaker which functioned for about 1 week before the lead was fractured. This invention was presented at Second International Conference on Medical Electronics in 1959 (19). The device had nickel-cadmium batteries, an electronic circuit, and a recharging antenna (Fig. 7). The scientists were active in the research field after this invention. Thus, Rune Elmqvist changed the medical field, and Ake Senning continued cardiac surgery. Arne Larsson survived both scientists and died on December 28th, 2001 at the age of 86. During his life, he changed 22 pacemakers, and 5 leads (19).
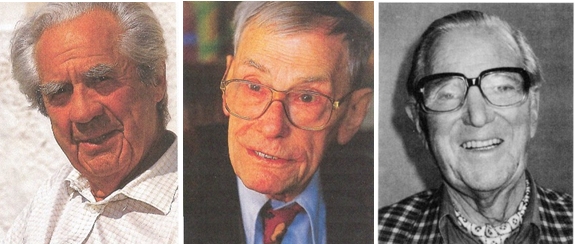
Figure 6. From left to the right: Ake Senning, the cardiac surgeon; Rune Elmqvist, a medical engineer; Arne Larsson, the first human to receive an implanted pacemaker (19). (Republished under CC-BY license rules from reference 19.)
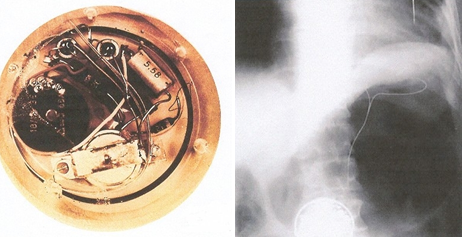
Figure 7. In the left: first implantable pacemaker. In the right: the X-ray after the pacemaker was implanted.
(Republished under CC-BY license rules from reference 19.)
In medicine, some inventions are made by mistake. Hence, an electrical engineer, Wilson Greatbatch, University at Buffalo in New York, made an important discovery accidentally. He was making an oscillator to record heart sounds and mistakenly changed the resistor, unknowingly plugging it and the oscillator started to generate a 1,8 ms pulse with a 1-second interval. He was also interested in medical research works and he understood that this rate was like a
heartbeat (20). At that moment Dr. William Chardack was chief surgeon at Buffalo's Veteran's Hospital. In 1958 Greatbatch, Chardack, and another surgeon Dr. Andrew Gage connected to the dog’s heart with their experimentally designed pacemaker and were happy to see the heart beating in synchrony with the pacemaker stimulation. They spent plenty of time in the lab improving the future pacemaker and always wearing a bow tie. Later they were called “the bow tie team” (Fig. 8). In 1960 they implanted a pacemaker in a 77-years old man with a complete atrioventricular block who lived for 2 years after implantation and died from natural causes. Since 1960 the pacemaker implantation procedure become common and spread worldwide (21).
In the 1970s the lead design was improved, becoming “screwable” and “tiny”. The lithium-iodine battery replaced the mercury oxide-zinc battery which increased pacemaker longevity. A titanium case was developed to cover the pacemaker. Pacemakers became non-invasive programmable with the use of radio-frequency telemetry. Dual chamber pacemakers were developed with synchronization of the atrium and ventricles while pacing. The steroid-eluting leads were developed in the 1980s which led to the decrease of the inflammatory reaction to the lead’s tip and the early rise of capture was minimalized.
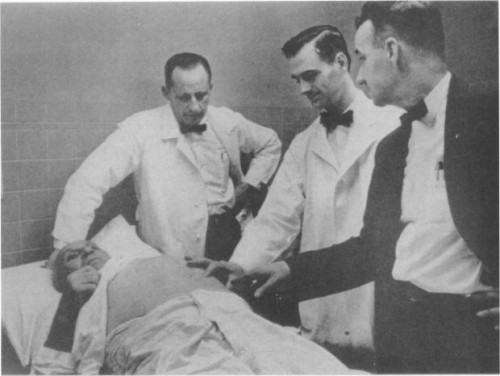
Figure 8. “The bow tie team” while examining the patient after the pacemaker implantation in 1960.
(Republished under CC-BY license rules from reference 19.)
The rate-response function was developed and pacemakers became more physiological. In the 1990s microprocessors were developed and pacing algorithms were improved. In the 2000s bi-ventricular pacing was demonstrated in patients with heart failure. In 2011 FDA approved the first magnetic resonance imaging compatible pacemakers which improved patients' life’s (22). Further developed telemetry to send information from distant places to the physician's computer made follow-up of patients with pacemakers easier.
Medtronic and Abbott developed leadless pacemakers which are delivered directly into the right ventricle via a special catheter. The latter one is the first leadless dual-chamber pacemaker (23). The devices are retrievable and the expected longevity of the battery is up to 10 years (Fig. 9).
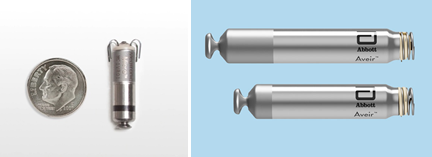
Figure 9. Leadless pacemakers developed by Medtronic on the left and by Abbott on the right. The latter one is the first leadless dual-chamber pacemaker.
( Reproduced from https://news.medtronic.com/Pacemakers and
Nowadays, the pacemaker has immense programs, components, and available wireless communication, which helps physicians to monitor the devices while patients are at home. Sixty-five years after the first pacemaker was implanted they developed from a huge external simple asynchronous pacing system that stimulated the heart regardless of the rhythm to small leadless pacemakers with atrioventricular synchronization. Remote monitoring of implantable devices simplified the patient's life and saved the physician's time. Thanks to the relentless efforts of researchers, engineers, and medical professionals, pacemakers have evolved into highly sophisticated and life-saving medical devices, providing hope and improved quality of life for millions of people with heart rhythm disorders.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: A.B.
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

