Effect of isolated protein diet on remodeling of the bronchial-alveolar-vascular microaxis of the lungs
ORIGINAL RESEARCH ARTICLE
Effect of isolated protein diet on remodeling of the bronchial-alveolar-vascular microaxis of the lungs
Article Summary
- DOI: 10.24969/hvt.2023.408
- Page(s): 296-305
- RELEVANT DISCIPLINES
- Published: 13/08/2023
- Received: 09/05/2023
- Revised: 03/08/2023
- Accepted: 05/08/2023
- Views: 6096
- Downloads: 3753
- Keywords: structural changes of the respiratory tract, exposome, rats, isolated protein diet
Address for Correspondence Elmira M Mamytova, Department of Neurology and Clinical Genetics named after A.M. Murzaliev, Kyrgyz State Medical Academy named after I.K. Akhunbaev, Bishkek, Kyrgyzstan
Mobile: +996551325314 Email.: elmiramamytova@yahoo.com
ORCID: Aycholpon T. Israilova - 0009-0004-7373-5814; Elmira M. Mamytova - 0000-0002-4322-5555;
Yusuf Kh-M Shidakov - 0000-0002-2779-5574; Ayna Dj. Mamytova - 0009-0007-1637-6984
Aycholpon T. Israilova1, Elmira M. Mamytova*1, Yusuf Kh-M. Shidakov2, Ayna Dj. Mamytova3
1Neurology and Clinical Genetics Department named after A.M. Murzaliev, Kyrgyz State Medical Academy named after I.K. Akhunbaev, Bishkek, Kyrgyz Republic
2Laboratory of modeling of pathological processes of the medical faculty of the Kyrgyz-Russian Slavic University named after B.N. Yeltsin, Bishkek, Bishkek, Kyrgyz Republic
3Department of Internal Diseases of the Kyrgyz State Medical Institute for Retraining and Advanced Training named after S.B. Daniyarov, Bishkek, Kyrgyz Republic
Abstract
Objective: to establish the remodeling mechanisms of the micro-axis of the bronchi-alveoli-vessels exposed to isolated protein diet.
Methods: Research design - randomized experimental study, the population of sixteen Wistar rats is divided into a main and control group. The main group was subjected exclusively to a protein diet, and the control group was on standard feed for a month. On the 15th and 30th days, the animals were phased out of the experiment and a histological analysis of the lungs was carried out to detect changes in the bronchio-alveolar-vascular microaxis. Age and body mass of animals were measured and compared at the beginning of the experiment and before autopsy. The independent and paired samples t-test has been applied for statistical analysis.
Results: Animals in both groups were comparable in age and body weight. Over time, the body mass increased in each group (217.5 (18.5) vs 246.2(18.2) gr., (p=0.0001) for the main group and 211.8 (10.6) vs 240.6 (11.7) gr, (p=0.0001) for the control group), but the weights of the main group did not differ from the control group (246.2 (18.2) gr vs 240.6 (11.7) gr, p=0.47). The isolated protein diet has led to an increase in collagen and elastin in the stroma surrounding the ventilation and perfusion pathway, leading to dystrophic changes not only in the organ’s stroma, but also in the bronchial walls and blood vessels of the lungs during a 30-day experiment. The above morphological changes showed significant remodeling of the microaxis of the broncho-alveolo-vascular exposome. At 15-day, only adaptive compensatory changes were observed with small differences from the control group.
Conclusion: The 30-day isolated protein diet disrupts the interaction and interdependence of the functioning and structural organization of the components of the bronchial-alveolar-vascular microaxis of the lungs. Relatively 15-day results showed adaptive and compensatory changes. Our findings may serve as a basis for future major clinical trials based on exposomal factors.
Key words: structural changes of the respiratory tract, exposome, rats, isolated protein diet
Introduction
In recent years, the exposome has gained wide popularity in the biomedical sciences, defined as a set of measures of all effects on the body throughout the life cycle and the health-related impacts of these factors (1). The complex interaction of the axes has been defined at the macro and micro levels of the exposome determined by genetic and epigenetic factors. Diet is considered the key factor of exposome with significant effects on the body both at the gross and cellular levels.
Investigations have shown that some diet types cause serious disturbances in the structure and functioning of organs, while other diets eliminate these disturbances (1, 4). For example, high-calorie diets contribute to obesity-related disorders, and diets with insufficient protein intake cause muscle wasting, metabolic disorders and reduced immunity (5).
Per se, lungs play a huge role in the metabolism of macronutrients beside the gas exchange (6). Meanwhile, there is little evidence in the literature about the interaction of changes in the components of the bronchial-alveolar-vascular microaxis of the lung exposome in different diets. It can be explained by rheological alterations of the blood associated with increased cholesterol, total protein and albumin levels (7).
In this study, we aimed to establish the interactions of the components of bronchial alveoli-vascular microaxis of the lung animals subjected to the isolated protein diet. The surrogate indicator of the microaxis was histomorphological changes in the lungs of lab rats.
Methods
Subject of study: a study of microaxis interaction of bronchial-alveolar-vascular components of animal lungs, reflected as the histomorphological changes. Animals were subjected to isolated protein diet.
Study population and intervention: A sixteen healthy and sexually mature male Wistar rats were enrolled into our study. Rats younger than 7 months and females were excluded. Baseline age and body weight was compared to values measured prior to slaughtering. The animals were divided into main and control arms randomly on the basis of isolated protein “diet” vs standard feeding. Isolated protein diet consisted of egg white, while standard feeding contained second-class wheat flour, oat cereals, cow milk, table salt, greenery, meat - young pork. The animals were fed ad libitum with corresponding ``diets`` and free access to water for up to 15 and 30 days. On the 15th and 30th days, laboratory rats were randomly selected and slaughtered for histomorphological analysis of the lungs. Animals were equally planned for each time of excision.
Study venue and ethical issues: The study was carried out on the basis of the laboratory of experimental modelling of pathological processes of the Kyrgyz Russian Slavic University (KRSU) in compliance with the rules of ARRIVE guidelines and laboratory practice, approved by the order of the Ministry of Health and Social Development of the Russian Federation from August 23, 2010 708 «On approval of the rules of laboratory practice». Rats were cared for, and fed by vivarium personnel in accordance with international standards of experimental work on animals (Consensus Guidelines on Animal Ethics and Welfare 2010).
The research protocol was approved by the local ethical committee of the NGO «Preventive medicine» of the Ministry of Health of the Kyrgyz Republic.
Age and body mass of animals were measured and compared at the beginning of the experiment and before autopsy.
Histomorphological analysis was performed on the 15th day to establish the beginning of pathological changes, which could be taken as a point of report when studying the nature of restorative reactions in the future and 30th day for observing substantial morphologic outcomes. The pulmonary fragments were fixed in a 10% neutral solution of formalin, dehydrated in increasing-concentration alcohols followed by the manufacture of paraffin blocks. Histological slices 5-7μm thick were stained with hematoxylin-eosin and studied for both gross and microscopic changes. For microscopic analysis a light microscope Olympus BX40 equipped with digital camera Levenhuk C130 NG and PC was used. The histomorphological data of the control and main animal groups were further compared.
Statistical analysis
Continuous variables are denoted by mean and standard deviation. A p value of less than 0.05 accepted statistically significant. An independent two-samples t-test for comparison of age and body weight between main and control groups. Baseline and pre-slaughtering values were analyzed separately. Furthermore, paired samples t-test was conducted to see potential changes. The statistical analysis was achieved through a STATA 16 software.
Results
Baseline demographics and comparison results
Eight laboratory rats underwent isolated protein diet with equally matched counterparts fed on standard diet, thus sixteen animals equally distributed into experimental and control groups. During experimental period no premature deaths or other events observed. Baseline mean age of main group was 7.6 (0.18) months, whereas control group’s values 7.5 (0.18) months with non-significant differences (p=0.49). Baseline mean body weight constituted 217.5(6.5) gr vs 211.8(3.7) gr, (p=0.46) in main and control groups, respectively. Values obtained just prior to slaughtering also did not reveal significant alterations between groups. Animals of both arms become elder and gained precise weight during follow-up (p=0.0001 for both).
|
Table 1. Age and weight of animals before and pre-autopsy |
|||
|
Independent samples t-test results |
|||
|
Parameters |
MG (n=8) |
CG (n=8) |
p |
|
BL age, months |
7.6 (0.53) |
7.5 (0.53) |
0.49 |
|
BL weight, gr |
217.5 (18.5) |
211.8 (10.6) |
0.46 |
|
PA age, months |
8.4 (0.72) |
8.2 (0.53) |
0.56 |
|
PA weight, gr |
246.2 (18.2) |
240.6 (11.7) |
0.47 |
|
Paired test results |
|||
|
Parameters |
Baseline (n=8) |
Pre-autopsy (n=8) |
p |
|
MG age, months |
7.6 (0.53) |
8.4 (0.72) |
0.0001 |
|
MG weight, gr |
217.5 (18.5) |
246.2 (18.2) |
0.0001 |
|
CG age, months |
7.5 (0.53) |
8.2 (0.53) |
0.0001 |
|
CG weight, gr |
211.8 (10.6) |
240.6 (11.7) |
0.0001 |
|
BL- baseline, CG – control group, gr – grams, MG – main group, PA – pre-autopsy |
|||
Morphological analysis
On the 15th day of the experiment, most of the large bronchi and parallel pulmonary arterial branches of experimental animals did not differ between groups.
In the medium-sized and small bronchi, the smooth muscle of the media cells was hypertrophied in the main group. The fibrous layers, the partial smooth muscle cells with finger-like projections protruded into the bronchial lumen. Together with the epithelial lining, they formed a kind of bridge with the formation of “multibarrel bronchi” (Fig. 1).
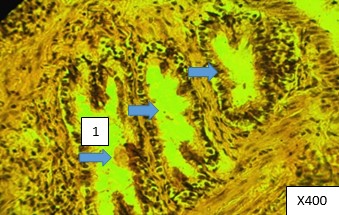
Figure 1. “Multibarrel bronchus” formation on the 15th day of egg white feeding (1-lumen of the multi-barrel bronchus) Paraffın fıllıng, hematoxylin -eosin staining, 400Х.
Epithelial cells have been detached into the bronchial lumen. The branches of the pulmonary artery at this level were characterized by the hypertrophy of the media, narrowing of lumen, and sometimes bizarrely widened perimeter (Fig. 2). Broncho-pulmonary anastomoses and collateral-type vessels (Fig. 3, 4) were also found.
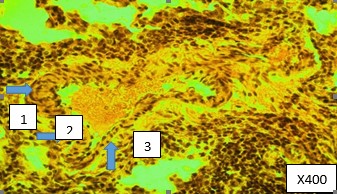
Figure. 2 - Pulmonary artery. Medial hypertrophy in some areas and atrophy in other parts of the vascular wall, with a bizarrely changed perimeter (1-lumen of the pulmonary artery, 2- hypertrophy of the media, 3- atrophy of other areas). Paraffın fıllıng, hematoxylin -eosin staining, 400Х
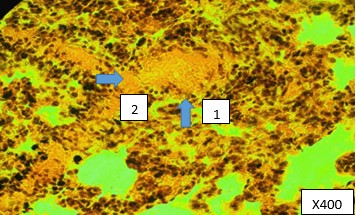
Figure 3. Bronchial vein plethora (1-accumulation of blood in the lumen of the vessel, 2-vascular wall ) Paraffın fıllıng, hematoxylin -eosin staining, 400Х
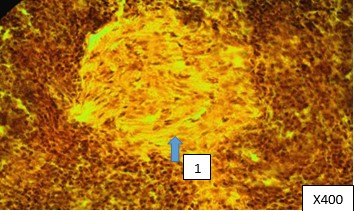
Figure 4. Collateral-type vessel ( 1-vessel clearance) Paraffın fıllıng, hematoxylin -eosin staining, 400Х
In general, structural compensation of vascular motion was observed by means of alternating activity of gas exchange in affected alveoli, we called this event the «dancing motion» of terminal bronchioli (Fig. 5, 6).
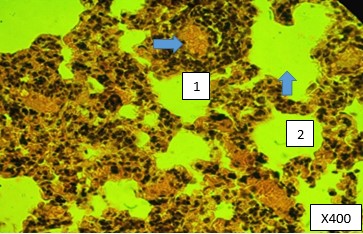
Figure 5. Hyperemic vessels in the physiological atelectatic zone of the lungs (1- full-blooded vessel, 2- atelectasis zone) Paraffın fıllıng, hematoxylin -eosin staining, 400Х
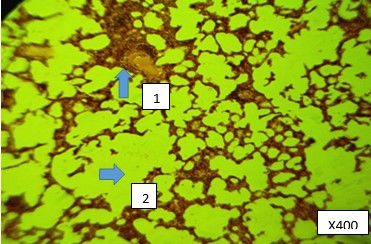
Figure 6. Narrowed vessels in the physiological emphysema zone of the lungs (1-blood vessel, 2-emphysema zone) Paraffın fıllıng, hematoxylin-eosin staining, 400Х.
On the 30th day of the experiment there was a partial transition of adaptive and compensatory reactions of bronch-oalveolar structures of the lungs to pathological changes. Primarily, increased secretion of proteinous mucus was noted by the clot formation in the bronchial lumen, attached to the epithelium of the fibrillary structures. In addition, admixture of blood in mucus secretion was rarely observed (Fig. 7).
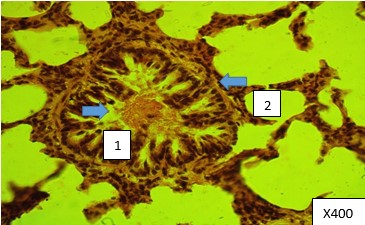
Figure 7. Admixture of blood in mucus secretion (1-blood admixture, 2-bronchus). Paraffın fıllıng, hematoxylin -eosin staining, 400Х.
A thickening of the bronchial epithelium was observed, possibly determined by the physiological proliferation of the cell population. As a result, the lumina of the small-sized bronchi and bronchioli was extensively narrowed compared to 15 days of experience. Epithelial microvillus formed a dense membrane and lost the ability to motion, which led to the accumulation of mucus in bronchi. Epithelial cells were exposed to mucoid swelling. The media of the bronchi was divided into separate segments, interspersed with slits and vacuoles (Fig. 8).
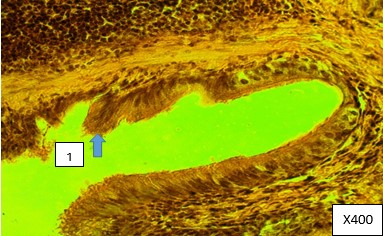
Figure 8. Epithelial microvilli are coated with dense film and unable to blinking (1-bronchial microvilli). Paraffın fıllıng, hematoxylin-eosin staining, 400Х
In contrast to previous morphological patterns, most of the pulmonary artery branches found hypotonic, with vascular edema and bloody streaks in the lumina. Bronchial arteries were constricted, and collateral-type vessels were apparent (Fig. 9).
In the lung parenchyma peribronchial lipodystrophic areas, metaplastic connective tissue and microhemorrhages were observed (Fig.10).
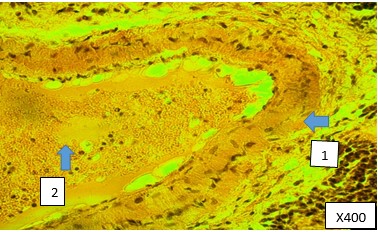
Figure 9. Pulmonary artery hypotonia with stasis and edema (1-pulmonary artery, 2- blood stasis). Paraffın fıllıng, hematoxylin -eosin staining, 400Х
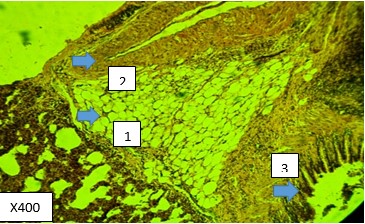
Figure 10. Lipodystrophy of lung parenchyma (1-fatty degeneration. 2- artery, 3- bronchus). Paraffın fıllıng, hematoxylin -eosin staining, 400Х.
On the basis of abovementioned histomorphological findings we presented comparison of 15th and 30th day results in a Table 2.
|
Table 2. Histomorphologic alterations of lungs on the 15th and 30th days autopsies |
||
|
Main group characteristics on 15th day (compensatory-adaptive changes) |
Main group characteristics on 30th day (pathological changes) |
Control group findings |
|
Hypertrophy1 of smooth muscle cells of medium-sized and small bronchi |
Marked narrowing of bronchial lumen (due to exaggerated epithelial hypertrophy) |
The pseudo-stratified and ciliated columnar epithelium in medium-sized bronchi and single-layer cuboid epithelium in small bronchi of healthy rats were unchanged. |
|
Detachment of epithelial cells into the lumen of bronchi |
Formation of a clump in the bronchial lumen (due to mucosal oversecretion) |
Neither epithelial cell rejection nor protein-mucosal oversecretion observed in control group animals |
|
Hypertrophy of smooth muscles of pulmonary arterial media |
Pulmonary artery atonia with swelling of the wall and congestion of blood |
Normal histophysiological patterns of pulmonary artery in animals fed on standard diet |
|
Formation of broncho-pulmonary anastomoses and collateral-type vessels |
Vasospasm of bronchial arteries and presence of collateral-type vessels |
Rare bronchial-pulmonary anastomoses and collateral vessels noted in control group animals. Bronchial artery spasm was not observed. |
|
Physiological atelectasis with vascular overflow and physiologic emphysemas with vascular spasm |
Adipose dystrophy of peribronchial parenchyma with proliferation of young connective tissue and microhemorrhages |
Occasional physiological atelectasis and emphysemas of certain lung segments, as an intermittent activity of the acini, with the corresponding vasoconstriction were noted. No adipose dystrophy was observed. |
|
1Defined by Kernogan index |
||
Discussion
Among environmental factors, diet is one of the key factors of exposome. The scientific justification for such a statement is based on a huge number of studies on the subject of caloric content of diets (with limited calories, Western, ketogenic, etc.) to organ-orientation (brain, heart, liver, kidneys, etc.).
Despite all the importance for theoretical, applied dietetics and medicine, the results of these studies have a significant drawback, namely, most studies do not take into account the interaction between the studied diet and different organs (1).
There are a number of studies on the effect of high-protein or low-protein diets (6) on the metabolism of the body (7), brain (8), kidneys (9), intestines (10), liver (11) and in patients with cancer (12).
As for the effect of protein and its connection with its concentration in the daily diet on the supporting apparatus of the lungs, there is one work (13) in which the effect of protein deprivation on the level of collagen and elastin in the lungs of newborn rats was studied, the animals were subjected to protein deprivation for 6 weeks. The study showed that protein deficiency leads to a decrease in the amount of collagen and elastin in the lungs.
Thus, the analysis of the above works testified to both positive and negative effects of a high-protein diet on various organs of experimental animals, which were associated with short-term (no more than 2 months) compliance with a daily diet with high protein intake. It should be noted, as we believe, that the effects of a high-protein diet depend not only on the duration of the diet itself, but also on the studied object (healthy animals or animals with simulated pathological conditions under experimental conditions), the type of protein (it is a protein of animal or vegetable origin), the age of the animal and the proportion of protein in the diet (35%, 50%, 70%).
Along with this, we did not find the information concerning on the impact of isolated protein diet on the lungs in biomedical literature databases. Our study showed a number of changes in the lungs on the 15th and 30th days of feeding rats only with the protein of chicken eggs.
On the 15th day of the experiment, changes in the lungs were generally characterized by adaptive and compensatory reactions of the respiratory and circulatory systems of the lungs. The changes mainly concerned the bronchi of small and medium caliber. For example, in small terminal bronchi and bronchioles, there were phenomena of granular epithelial dystrophy, hypertrophy of the muscular membrane with the formation of a kind of sphincter. In the respiratory compartment, physiological atelectasis alternated with areas of physiological emphysema, equipped with thin partitions with narrow vessels. In general, there was a structural provision of intermittent gas exchange activity in individual alveoli associated with vasomotion, the "dancing" of terminal bronchi and bronchioles. And it is not possible to interpret these data because there is no similar information in the literature.
Of particular interest is that the presence of hypertrophic changes in smooth muscle cells is caused by the interaction of remodeling of the wall of the medium and small bronchi, as well as the branches of the pulmonary artery that go with them in pairs. The reticular stroma, where they lie, contributes to the reduction of the walls of the medium and small bronchi and the branches of the pulmonary artery that go with them in pairs. Unlike collagen, the reticular stroma does not rigidly fix the walls of the bronchi and arteries, which gives them the opportunity to regulate their lumen ventilation of the alveoli. This is how the interaction of changes in the micro-axis of the bronchi-alveoli-vessels is really manifested when rats are fed only with the protein of chicken eggs.
In the small terminal bronchi and bronchioles, there are phenomena of granular epithelial dystrophy, hypertrophy of the muscular membrane with the formation of a kind of sphincter, which apparently regulate the alternate flow of air into the alveoli. The branches of the pulmonary artery at this level and arterioles differ in ambiguous remodeling, when some of them are sharply narrowed, others are expanded or not changed. Against this background, full-blooded bronchial arteries and veins stand out. Activation of the bronchial blood flow against the background of pulmonary disorganization contributes to the transfer of the high-energy flow of the large circulatory circle to the energy-intensive small circle by forming bronchopulmonary anastomoses.
In the respiratory compartment there are physiological atelectases, thick interalveolar septa equipped with full-blooded vessels. Perhaps these vessels serve as a reservoir for depositing blood and play a minor role in external gas exchange. On the contrary, the alveoli in a state of physiological emphysema are equipped with thin partitions with narrow vessels. It must be assumed that the blood flow through these vessels is accelerated, which ensures adequate external gas exchange. In this aspect, it is appropriate to agree that gas exchange under experimental conditions occurs not only in capillaries, but also on arterioles and venules.
On the 30th day of the experiment, a partial transition of adaptive and compensatory reactions of the respiratory and circulatory systems of the lungs into the category of pathological was observed.
There was a thickening of the bronchial epithelium, which may be determined by the physiological proliferation of the cell population. As a result, the lumen of the small bronchi and bronchioles are narrowed to a greater extent than on the 15th day of the experiment. On the microvilli of the epithelium, a dense film consisting of a protein-mucous secretion is formed and the ciliated epithelium loses its ability to flicker, which contributes to the accumulation of mucus in the bronchi. In this regard, it must be assumed that a protein diet stimulates the secretion of mucus by the protein-mucous glands of the bronchial epithelium.
In contrast to the data of previous experiments, the following changes were observed from the circulatory system: many branches of the pulmonary artery were with signs of atony, with edema of the vascular wall, contained plasma mixed with shaped blood elements in the lumen. There are no similar data in the literature, which complicates the results of our research.
Along with the above-mentioned changes in the lung parenchyma, there were areas of fatty degeneration located in the vicinity of the bronchi, as well as overgrowth of tender young connective tissue and microbleeds. Here, the phenomena of fatty degeneration and the presence of sclerotic changes in the paravasal and peribronchial environment, with certain reservations, can be explained by the fact that in the absence of fat in the diet, proteins break down into glucogenic and ketogenic amino acids. In turn, ketogenic amino acids break down into fatty acids and ketogenic bodies. Fatty acids may well lead to fatty degeneration, as well as an increase in cholesterol in the blood serum.
A high concentration of cholesterol, causing sclerotic changes in blood vessels in other organs, could have repercussive changes in the lungs. An increase in albumin content is usually the cause of temporary cessation of blood flow in the capillaries, which could lead to hypovascularization of the respiratory muscles and diaphragm with a corresponding violation of external respiration. Maybe that is why the alternation of areas of alveolar decline with their increased airiness was clearly revealed in the lungs. It must be assumed that this has an adaptive value, because it is better to combine intensive work of the alveoli with the allocation of time for rest than ineffective simultaneous activity.
However, uncontrolled constant change of functional activity causes hypertrophy of the muscular membrane of the bronchi and branches of the pulmonary artery. This causes insufficient intake of air into the alveoli and blood, into the vessels surrounding them. Ventilation and circulation in the lungs decreased synchronously in the first 15 days of the experiment and not consistently - on the 30th day.
The absence of fats, carbohydrates and a high concentration of proteins in the diet, in all probability, led to an increase in collagen and elastin in the stroma surrounding the ventilation and perfusion pathways. It is quite possible that this was the cause of dystrophic changes not only in the stroma of the organ, but also in the walls of the bronchi and blood vessels in our experiments.
As noted above, on the 30th day of the experiment, the relationship between changes in the components of the micro-axis of the bronchi-alveoli-lung vessels was disrupted, which in pathophysiology is designated as the absence of a normal relationship between ventilation and perfusion.
It is possible that the presence of a dense border covering the microvilli of the lung epithelium is due to a violation of the metabolic function of the organ, and foci of atelectasis are caused by the synthesis of surfactant by alveolocytes.
Study limitations
Experiments were conducted to study the short-term effects of an isolated protein diet. For a more complete picture of the effects of an isolated protein diet on the body of the studied object, it is necessary to conduct a study on the effect of a long-term high-protein diet.
Conclusion
Thus, a 30-day isolated protein diet disrupts the interaction and interdependence of the functioning and structural components of the bronchial-alveolar-vascular microaxis of the lungs. Relatively 15-day results showed adaptive compensatory changes. Our findings regarding the lung exposome may serve as a basis for future large-scale randomized clinical trials.
Ethics: The study complies with local and international standards (Consensus Guidelines on Animal Ethics and Welfare 2010) of animal care and regulations on experimental studies. The study protocol was approved by the local ethical committee of the NGO «Preventive medicine» of the Ministry of Health of the Kyrgyz Republic.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: A.T.I., E.M.M., Y.Kh-M. Sh., A.Dj.M. equally contributed to the study and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

