Management of arrhythmias during pregnancy
EDITORIALS
Management of arrhythmias during pregnancy
Article Summary
- DOI: 10.24969/hvt.2023.411
- CARDIOVASCULAR DISEASES
- Published: 15/08/2023
- Received: 07/08/2023
- Accepted: 08/08/2023
- Views: 6760
- Downloads: 4591
- Keywords: Pregnancy, HRS Consensus Statement, maternal arrhythmias, fetal arrhythmias
Address for Correspondence*: Zhenisgul Tlegenova, West Kazakhstan Marat Ospanov Medical University, 68, Maresyev Street, 030019, Aktobe, Kazakhstan. Phone: +7 707 4998565, E-mail: zhenisgul.tlegenova@zkmu.kz
Zhenisgul Tlegenova ORCID: 0000-0002-3707-7365 Vadim Medovchshikov ORCID: 0000-0001-5996-8305
Zhenisgul Tlegenova*, Vadim Medovchshikov
West Kazakhstan Marat Ospanov Medical University, Aktobe, Kazakhstan
Pregnancy is a complex physiological state marked by various hormonal, cardiovascular, and hemodynamic changes, which can make pregnant women more susceptible to arrhythmias (1). Physiological changes in the cardiovascular system occur during pregnancy: heart rate increases by 10-25% and cardiac output by 45-50%. Also, pregnancy is associated with increased sympathetic and decreased parasympathetic activity. This, together with hormonal changes, can lead to a change in the structure and function of the myocardium and have a proarrhythmic effect (1-4). In addition, maternal age, prevalence of cardiovascular risk factors, e.g. obesity, and comorbidity, including congenital heart diseases, are increasing (6).
The presence of arrhythmias during pregnancy varies across different populations, and more prevalent in the setting of structural heart disease (SHD). While most arrhythmias observed in pregnant patients are generally benign, such as sinus arrhythmia (60%), supraventricular tachycardia (SVT, 14%), and premature beats (19%), life-threatening arrhythmias like significant SVT or ventricular tachycardia (VT) are far less common (6). Vaidya et al. found a significant increase in hospitalizations due to atrial fibrillation (AF) by 111% and VT by 127% over 12 years (2). Of particular concern, AF is emerging as the most commonly diagnosed sustained arrhythmia during pregnancy (2). The presence of arrhythmias during pregnancy has significant implications for both the mother and the developing fetus. Maternal outcomes can involve palpitations, chest pain, syncope, heart failure, and an increased risk of thromboembolic events, preterm labor, and delivery. Poorly controlled arrhythmias may result in reduced blood flow to the placenta, potentially leading to fetal distress, growth restriction, or even fetal demise. Additionally, certain antiarrhythmic medications may pose risks to the developing fetus, necessitating careful consideration of maternal treatment choices to ensure fetal safety.
Diagnosing arrhythmias during pregnancy presents challenges due to overlapping symptoms with normal pregnancy-related physiological changes. Non-invasive techniques like electrocardiography, echocardiography, and ambulatory monitoring play a vital role in diagnosing arrhythmias and evaluating their severity.
The treatment options must carefully weigh the potential risks and benefits for both the mother and the fetus, depending on the presence of underlying structural heart disease, type and severity of the arrhythmia, and the stage of the pregnancy. Interventions may include adenosine, beta-blockers, and specific arrhythmic drugs with safety data during pregnancy, rarely, catheter ablation with minimal/ zero fluoroscopy can be used (3, 4).
According to a survey, a significant number of cardiology professionals expressed discomfort when it comes to providing care for this patient population (5).
In this editorial, we would like to give a brief understanding of 2023 HRS Consensus Statement on the Management of Arrhythmias during Pregnancy (6).
Key features of treating arrhythmias in pregnant women
1. Multidisciplinary approach. A team of specialists collaborates, including obstetricians, cardiologists and/or electrophysiologists, pediatric electrophysiologists, neonatologists and anesthesiologists, to ensure comprehensive care for both mother and baby.
2. Risk assessment. Before initiating treatment, the healthcare team evaluates the potential risks associated with the arrhythmia and proposed interventions, considering factors such as arrhythmia type, maternal health, gestational age, and fetal well-being.
3. Timing of treatment. Some treatments may be delayed until after the first trimester to minimize potential risks during critical periods of fetal development.
4. Conservative management. In many cases, well-tolerated and low-risk arrhythmias may be managed conservatively through close monitoring of the mother's heart rhythm and fetal status, without the need for pharmacological intervention.
5. Medications. When drug therapy is necessary, medications with the most extensive history of safe use during pregnancy and lactation, administering the lowest effective dose, and regularly reassessing the necessity for the same dose or type of antiarrhythmic medication, including during the postpartum period.
6. Electrical cardioversion or defibrillation may be necessary to restore normal heart rhythm for the cases of hemodynamically significant maternal arrhythmias and should be performed under close fetal monitoring.
7. Non-pharmacological interventions like catheter ablation and implantable devices may be considered to treat the arrhythmia while minimizing/ zero radiation exposure to the fetus.
8. Regular fetal monitoring is crucial throughout the treatment process to assess the baby's well-being using ultrasounds, fetal heart rate monitoring, or specialized tests.
9. Genetic screening and counseling for parents with a suspected or known inherited syndrome to assess potential fetal risks and for therapeutic optimization.
10. Lifestyle modifications. Pregnant women with arrhythmias may be advised to make certain lifestyle changes, such as avoiding stimulants like caffeine and nicotine that can worsen arrhythmias.
11. Postpartum care. Management of arrhythmias may continue after delivery, as hormonal changes and stress during labor can sometimes trigger or worsen arrhythmias.
12. Patient education. Pregnant women with arrhythmias receive education about their condition, treatment options, and the importance of compliance with medical recommendations, including understanding warning signs and when to seek immediate medical attention.
Management of the most common arrhythmias presented in Figure 1.
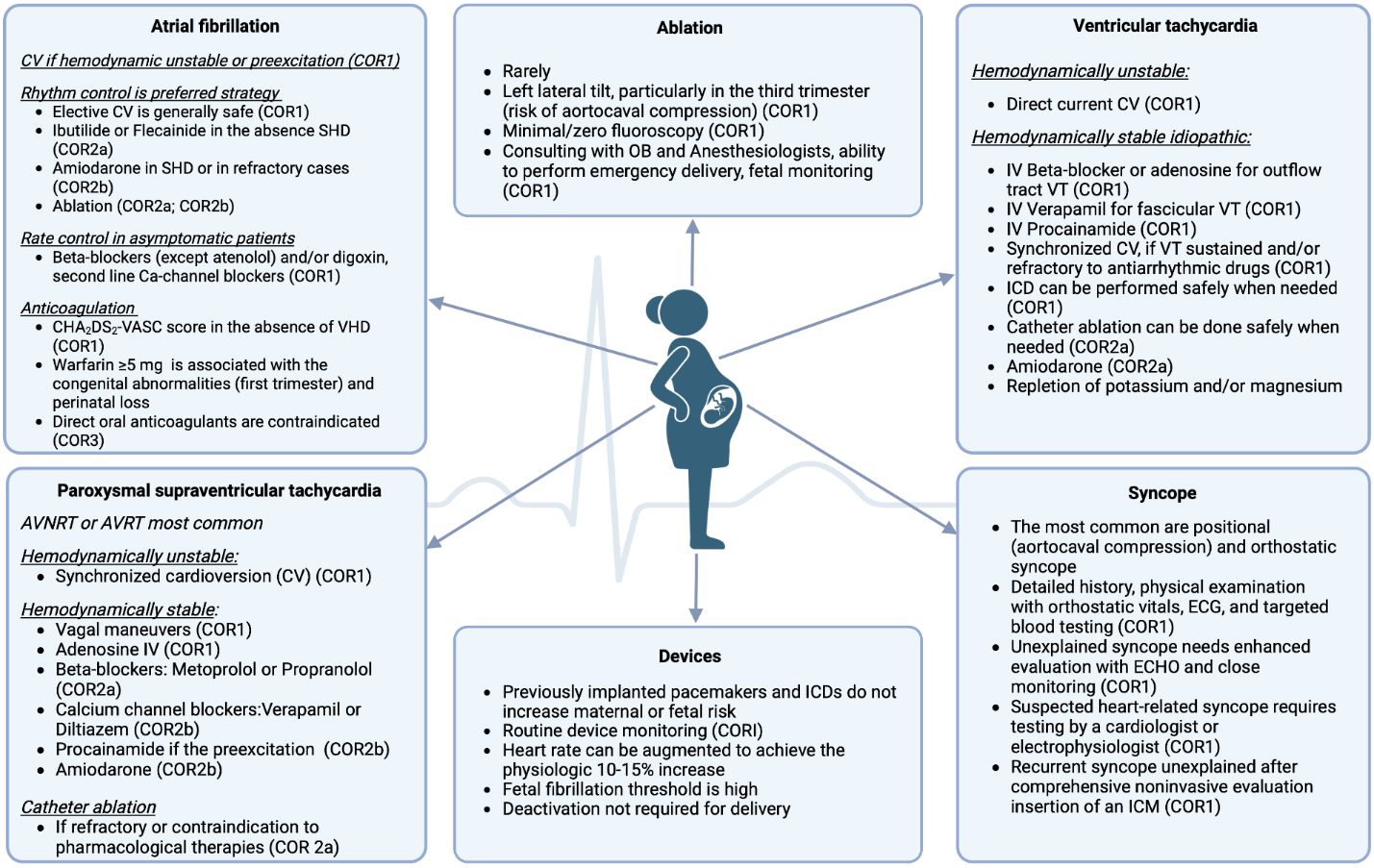
Figure 1. Arrhythmia management during pregnancy
Recommendations for management of fetal arrhythmias
Fetal arrhythmias are abnormal heart rhythms of the developing baby during pregnancy, detectable via prenatal ultrasound or monitoring heart rate. Fetal arrhythmias are diagnosed in approximately 2% of pregnancies and account for 10-20% of the referrals to fetal cardiologists (7). Fetal tachycardia is diagnosed when the ventricular rate exceeds 180 bpm (normal rate: 110-160 bpm). The majority of fetal tachycardias are SVT, of which SVT associated with atrioventricular accessory pathway and atrial flutter are most common (8). The majority of fetal SVTs can be effectively treated through maternal/transplacental administration of antiarrhythmic medications. Digoxin, propranolol, flecainide, sotalol, propafenone, verapamil and amiodarone have been reported for the management of fetal SVT (8). Ventricular tachycardia is very rare in the fetus.
Here are some common approaches to treating fetal arrhythmias:
1 Underlying etiology. The treatment approach may vary depending on the cause of the fetal arrhythmia.
2. Presence of cardiac failure. Fetal hydrops is often associated with severe heart dysfunction, and immediate intervention is necessary in such cases.
3. Gestational age. The stage of pregnancy plays a role in deciding the course of action. In some instances, deliverу of fetus may be preferred instead of in utero treatment.
4. Benign arrhythmias. Presence of premature atrial contractions or ventricular contractions are usually benign and may not require additional surveillance or changes in delivery planning unless SHD is present.
5. Channelopathies. For fetus with channelopathies avoiding factors that worsen maternal electrolyte imbalances and medications is crucial. Pregnant patients with genetic conditions like long QT syndrome should be educated about fetal bradycardia as an in utero manifestation of the condition rather than an adverse effect of maternal medication. Maternal beta-blocker therapy may need to continue in such cases.
6. Sustained fetal tachycardias. Usually treated with transplacental (maternal) administration of antiarrhythmic drugs, but delivery might be considered if appropriate.
7. Pharmacological considerations. The dosing of medications is generally based on maternal dosing, with direct fetal administration reserved for cases where absorption is likely to be inadequate (e.g., hydropic fetuses).
8. Baseline maternal assessment monitoring and precautions. Baseline maternal assessment, including history, examination, electrocardiogram, and echocardiogram, is appropriate before prescribing maternal antiarrhythmics for a fetal arrhythmia indication. During antiarrhythmic drug administration, monitoring the mother is crucial to mitigate potential drug-related side effects, such as excessive QT prolongation. Adhering to FDA-mandated dosing and precautions is essential.
9. Multidisciplinary planning. Significant fetal arrhythmias should involve a multidisciplinary team in planning the timing and location of delivery, considering potential risks to both the mother and fetus and the response to therapy. Fetuses with complex arrhythmias and those associated with SHD should be delivered in centers with experience in managing such cases.
10. Lack of randomized trials. Currently, there are no randomized trials of medical therapy for fetal arrhythmias, so treatment algorithms are based on observational studies, local experience, and monitoring fetal response to therapy.
Arrhythmias during pregnancy demand increased attention and research due to the growing number of pregnancies in women with pre-existing heart conditions and the increasing age and comorbidities of pregnant women in modern society. Advancing our knowledge in this area empowers healthcare professionals to provide better care to pregnant women with arrhythmias, ensuring safer pregnancies and healthier outcomes for both the mother and her baby.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: Z.T. and V.M. equally contributed to the preparation of manuscript
Acknowledgement and funding: None to declare
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

