From Editor-in-Chief: On current issue, our SCOPUS metrics and databases, ICMJE updates on artificial intelligence in manuscript preparation, ESC 2023 congress trials, 2023 ESC and ACC/AHA guidelines and statement documents, long COVID
EDITORIALS
From Editor-in-Chief: On current issue, our SCOPUS metrics and databases, ICMJE updates on artificial intelligence in manuscript preparation, ESC 2023 congress trials, 2023 ESC and ACC/AHA guidelines and statement documents, long COVID
Article Summary
- DOI: 10.24969/hvt.2023.415
- CARDIOVASCULAR DISEASES
- Published: 31/08/2023
- Received: 29/08/2023
- Accepted: 30/08/2023
- Views: 5935
- Downloads: 4220
- Keywords:
Address for Correspondence: Gulmira Kudaiberdieva, Editor-in-Chief Heart, Vessels and Transplantation
Email: editor-hvt-journal.com

Dear readers,
In current September 2023 issue, you can find editorial comments on - 2022 ESC guideline on cardiovascular (CV) risk assessment and management in patients undergoing non-cardiac surgery, 2023 HRS guideline on management of arrhythmias in pregnancy, AHA statement of dual heart-lung and heart –kidney transplantation, two editorials on recent ESC EAPCI documents on coronary physiology assessment and percutaneous coronary intervention (PCI); research articles on - role of fragmented QRS in prediction of outcomes in patients with myocardial infraction (MI) undergoing PCI, risk factors in prediction of severity of coronary artery disease (CAD) in young patients undergoing coronary bypass surgery (CABG), percutaneous transvenous balloon commissurotomy in children and adults with mitral stenosis, experience with zero-fluoroscopy ablation of arrhythmias and mortality rate and dynamics in population; comprehensive review on combined surgery - mitral valve repair and septal myectomy in hypertrophic cardiomyopathy; case reports on –management of atrial myxoma presenting as hemiplegia in a child, subclavian coronary steal syndrome after CABG, late presentation of ALCAPA syndrome discovered during primary PCI, coil embolization of saccular celiac aneurysm; interesting historical note on history of cardiac pacemaker invention and journey to current days of leadless devices; and quiz on cardiovascular surgery.
I would like to share the updates on our indexing in databases status and new requirements for submissions of manuscripts.
Good news are: we received our rank in SCOPUS database (Fig 1.): our CiteScore rank in surgery is – quartile - Q4, rank – 456/496 journals; cardiology and cardiovascular medicine – quartile 4, rank 334/354 journals. CiteScore 2022 - 0.2 and SNIP 2022 – 0.034. Good result for starting point and we need to move up in rank by improving quality of our content.
Another one is that we now indexed in BIOSIS Clarivate database. We are working on inclusion of our journal in PUBMED/ PMC – sources for evidence --based medicine knowledge pools and Clarivate Emerging sources indexes (latest is the starting point with further inclusion in Web of Science) – evidence –based medicine knowledge and journals and scientists performance evaluation databases.
ICMJE published update on their guidelines for medical journals (1). Update is in large part is about the use of artificial intelligence (AI) in publishing – writing manuscripts and evaluation of manuscripts.
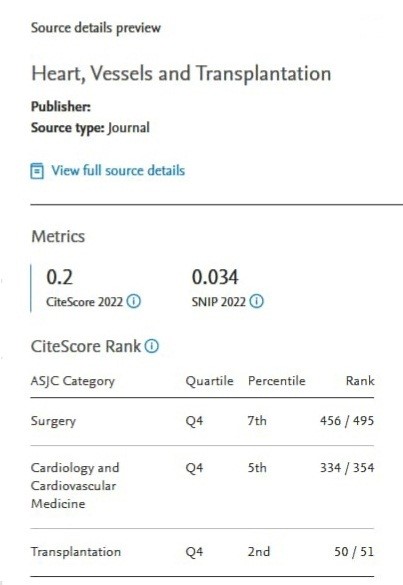
Figure 1. SCOPUS CiteScore rank for Heart, Vessels and Transplantation
Due to the latest advances in AI technology – we require now that authors of manuscripts submitted to our journal should declare if they used the AI technology (LLM, ChatGPT, etc) in writing manuscripts or used AI in preparation of pictures, figures and other media. Authors should not include AI in the authors list. In addition, as journal we further require authors to acknowledge they critically read, corrected and revised the manuscript or parts prepared by AI technology as the authors only not machine are experts on the topic of their research and responsible for intellectual content. Reviewers are also required to declare if the used AI technology in evaluation of manuscripts. Authors are also advised to use a more comprehensive language and follow the Sex And Gender Equity in Research (SAGER) guidelines for reporting the sex and gender information. The last update is regarding that all authors should critically read and approve the manuscript for publication – we already have been using this rule since 2017.
We continue our effort to bring to your attention latest evidence-based recommendations prepared by international societies and associations so you can study and use in your clinical practice
ACC/AHA guideline on chronic coronary heart disease management was in July 2023 (2) and 5 ESC guidelines were released during ESC 2023 congress at the end of August, 2023 – on management of acute coronary syndromes (3), endocarditis treatment (4), focused update on heart failure (HF) ESC 2022 guidelines (5), cardiomyopathies (6) and management of CV diseases in diabetes (7).
All these guidelines will be presented by our Editors and invited experts in form of editorials in forthcoming issues.
Besides these major guidelines several statements (AHA) and consensus, position (ESC) documents deserve your attention: on heart-lung and heart kidney transplantation – you can find comment in our current issue (8), on management of perioperative cardiac ischemia in cardiac surgery (9), management of pulmonary hypertension in congenital heart disease and management of cardiomyopathies in children (10, 11), EACVI document on transesophageal echocardiography (12). These documents will be also presented by our editors and invited experts.
Among trials presented at ESC 2023 Congress and studies published recently, few caught my attention. Two studies in the field of cardiac surgery and intervention worth mentioning: The alternative for bioprosthetic and mechanical aortic valve replacement, Ross procedure (the switch procedure with pulmonary autograft) has been shown in meta-analysis to increase survival in children and young patients from 85% in mechanical valve replacement to 95% with Ross procedure. It is important that mismatch of other types of valves with growth of children is less with Ross procedure (13).
Transcatheter aortic valve replacement (TAVR) has been shown to improve survival of patients with cardiogenic shock in elderly patients >75 years old and STS score 10; 30 days mortality was 13% with TAVR as compared to 33-47% without TAVR (here balloon valvuloplasty was performed in 7.8% and PCI in 1.52% of patients). Thus patients with cardiogenic shock appropriate for TAVR procedure, may benefit the procedure and have good survival (14).
Studies presented at 2023 ESC congress and I would like to briefly mention include: STEP-HFpEF, NOAH-AFNET 6, CASTLE HTx, DELIVER, OCTIVUS, and TAVR –CMR. Studies on management of HF with obesity, with worsening of symptoms and AF in end-stage HF, as well as anticoagulation in patients with atrial high-rate episodes (AHRE) and use of advanced imaging techniques to guide PCI and TAVR.
Semaglutide (a potent glucagone –like peptide (GLP) 1 agonist, is used for weight reduction) has been shown to have multiple positive effects in HF with preserved ejection fraction (HFpEF) patients with obesity (>30 kg/m2) beyond weight reduction in STEP-HFpEF trial (15): significant reduction in weight but also increase in 6-minute walking distance, improvement in HF
symptoms (Kansas City Cardiomyopathy Score), reduction in C-reactive protein values by half, decrease in death from any case during 57 weeks of follow-up as compared to placebo group. GLP 1 agonist in HF patients reduces not only weight but also reduces inflammation, improves symptoms and physical capacity.
NOAH-AFNET 6 trial (16) that evaluated anticoagulation with edoxaban in patients with cardiac implanted electronic devices and AHRE did not find benefit of anticoagulation in prevention of stroke and embolism but was associated with increased bleeding risk. Therefore, anticoagulation should be prescribed by indication based not only on presence of AHRE but also supported by electrocardiogram documented atrial fibrillation (AF).
Catheter ablation of AF in patients with end-stage HF (CASTLE HTx trial) reduced mortality during 18 months of follow-up by 71% (HR-0.29%, 95% CI 0.12-0.72) – 6% of patients in ablation group and 20% of patients in control group died during follow- up (17). Catheter ablation reduced not only death but also need for left ventricular assisted devices and transplantations compared to medical therapy. These studies demonstrate that more aggressive management as ablation of AF in end-stage HF can reduce mortality.
Of interest is the analysis of DELIVER trial on effects of dapagliflozin in patients with HFpEF with worsening of HF symptoms. Worsening of HF symptoms was defined as need for diuretic intensification. Diuretic intensification alone was associated with 50% increase in adverse outcomes and treatment with dapagliflozin reduced the need for diuretic intensification by 28% and reduced composite outcome of HF worsening and cardiovascular death by 24% (18).
Two interesting trials were presented regarding the guidance of PCI by intracoronary imaging: optical coherence tomography (OCT) versus angiography and intravascular ultrasound (IVUS) -guided PCI (19, 20). OCT- guided PCI appeared to be non-inferior to IVUS in terms of outcomes – mortality, target vessel MI and target vessel revascularization, however procedural complications were lower in OCT group (p=0.047) (19). In another trial (20) OCT-guided PCI versus angiography- guided PCI resulted in larger stented vessel diameter (p<0.001) in patients with CAD and diabetes. New imaging modalities can be used to guide PCI not only stenting as recommended in current guidelines.
Choice of imaging technique in favor of magnetic resonance (MRI) guided TAVR vs computed tomography (CT) guided TAVR was the goal of TAVR -CMR study: MRI - guided implantation was successful in 93% and CT guided implantation in 90.7% of patients, thus MRI was non-inferior to CT in terms of procedural outcomes. MRI may be preferred for those with allergy to contrast injection during CT (21).
Pandemics public emergency ended in May 2023, however virus continue evolving with new mutations. New vaccines have been developed targeting new variants. Bivalent vaccines has been shown to be effective in reducing hospitalizations and emergency room visits not only in adults but recently in children > 6 months old as well (22).
Long COVID or PASC syndrome is being investigated extensively, including NIH and other agencies (23, 24). Recent study from New York demonstrated that new onset persistent hypertension is by 2.23 times (95%CI 1.48-3.54, p<0.001) more often developed in hospitalized COVID patients and by 1.53 times more often in non-hospitalized COVID patients (95%CI 1.22-1.90, p<0.01) as compared to patients with influenza. The risk was higher in population older than 65 years with comorbidities, male and those receiving pressors and corticosteroids. It should be mentioned that 1/5 of COVID patients developed persistent hypertension during hospitalization (24). Thus, healthcare professionals should recommend their patients to sustain protection and make vaccinations.
Gulmira Kudaiberdieva
Editor-in-Chief
Heart, Vessels and Transplantation
Peer-review: Internal
Conflict of interest: None to declare
Authorship: G.K.
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

