The role of coronary physiology in the management of percutaneous coronary intervention: Insights from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Consensus
EDITORIALS
The role of coronary physiology in the management of percutaneous coronary intervention: Insights from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Consensus
Article Summary
- DOI: 10.24969/hvt.2023.416
- CARDIOVASCULAR DISEASES
- Published: 02/09/2023
- Received: 01/09/2023
- Accepted: 02/09/2023
- Views: 5912
- Downloads: 4201
- Keywords: percutaneous coronary intervention, coronary physiology, instantaneous wave-free ratio, fractional flow reserve, longitudinal vessel analysis
Address for Correspondence: Marco Bernardi, Department of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, Piazzale Aldo Moro 5, Rome, Italy.
Email: marco.bernardi23@gmail.com Twitter: MarcoBernardiMD ORCID: 0000-0001-9269-8829
Dario Mafricaa, ,Luigi Spadaforaa, Kristian Galantib, Giuseppe Biondi-Zoccaic,d , Marco Bernardia
aDepartment of Clinical, Internal Medicine, Anesthesiology and Cardiovascular Sciences, Sapienza University of Rome, Rome, Italy
bDepartment of Neuroscience, Imaging and Clinical Sciences, G. D’Annunzio University of Chieti-Pescara, Chieti, Italy
cDepartment of Medical-Surgical Sciences and Biotechnologies, Sapienza University of Rome, Latina, Italy;
dMediterranea Cardiocentro, Napoli, Italy
Abstract
The European Association of Percutaneous Cardiovascular Interventions (EAPCI) recently released a consensus statement on coronary physiology's role in managing percutaneous coronary interventions (PCI).
Indeed, in recent years, significant advancements have been made in coronary imaging techniques, which have greatly improved our ability to assess stenosis features. Techniques like instantaneous wave-free ratio (iFR), fractional flow reserve (FFR), and longitudinal vessel analysis have evolved, providing insights into the hemodynamic significance of coronary lesions and guiding treatment decisions, particularly in PCI. This commentary aims to enlighten the critical issues of the EAPCI statement, briefly reviewing the main techniques for the study of coronary physiology and their applications.
Key words: percutaneous coronary intervention, coronary physiology, instantaneous wave-free ratio, fractional flow reserve, longitudinal vessel analysis
“Physiology and psychology cover, between them, the field of vital phenomena…”
Wilhelm Wundt
Traditionally, coronary stenoses were assessed by estimating the percentage of flow-limiting seen in coronary angiography, recognizing stenoses that limit blood flow more than 70% as significant (1). However, it has been demonstrated by several studies that percutaneous coronary intervention (PCI) guided by angiography does not always determine the restoration of regular blood flow, and it can lead to suboptimal results (2, 3). Indeed, coronary physiology is complex and requires to be analyzed through physiological tools, such as instantaneous wave-free ratio (iFR), fractional flow reserve (FFR), and longitudinal vessel analysis, enabling the assessment of functional characteristics of stenoses and potential optimization of the results. Furthermore, there are some tricky situations where coronary angiography alone cannot determine the appropriate treatment (e.g., the presence of multiple stenoses, suboptimal PCI, and borderline stenoses).
Using physiological tools during coronary angiography can help address these issues, despite their use is inherently limited by cost (4). Indeed, they guarantee a better understanding and quantification of the ischemic impact caused by the stenoses, better decision-making in terms of intervention, and a precise post-PCI assessment. In specific subgroups, such as elderly patients, management of coronary artery disease (CAD) remains challenging, and treatment choices are made difficult by the frailty of older patients and the presence of comorbidities (5). In this background, the recently published FIRE trial found a significantly lower risk of the composite of death, myocardial infarction, stroke, or any revascularization at 1-year patients aged ≥ 75 years who underwent physiology-guided complete revascularization than patients who received culprit-lesion–only PCI (6).
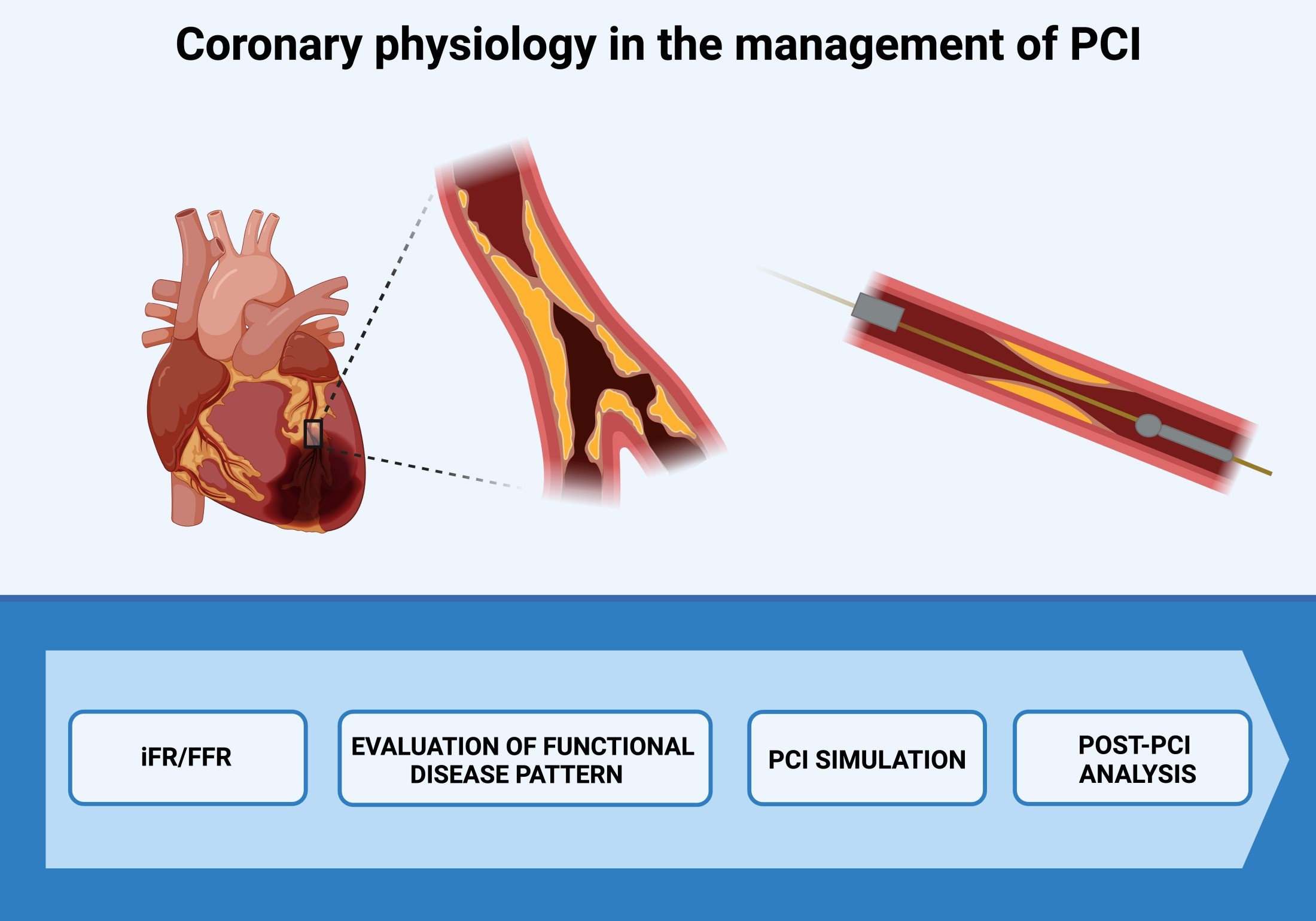
Figure 1. Coronary physiology in the management of PCI
PCI - percutaneous coronary intervention, iFR - instantaneous wave-free ratio, FFR - fractional flow reserve. Created with Biorender.com
In the interesting statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) (7), Escaned and coauthors provided an exhaustive analysis of the possibilities of functional coronary angiography, describing the currently available tools for the study of coronary physiology (Fig. 1). They widely described the main functional tests and their applications in clinical practice, especially stenting decision-making in cath-labs. According to the authors, longitudinal vessel analysis is primarily used to evaluate the potential benefits of PCI. One of the most intriguing aspects of the statement is that coronary stenoses can be assessed by precisely evaluating the pressure parameters, which turn into myocardial perfusion. Furthermore, this kind of evaluation can be applied not only in the pre-PCI assessment but also after the procedure to evaluate its effectiveness. This type of analysis widely overcomes the angiography-only approach, which merely estimates the amount of stenosis determined by the coronary lesion. This method is superficial, as it fails to characterize the real hemodynamic impact of the stenosis. As a result, Escaned and coauthors (7) emphasized the difference between focal and diffuse disease patterns in terms of the hemodynamic effect of the stenoses, which can be assessed using longitudinal vessel analysis and can lead to specific treatments. The authors also proposed two valid pre and post-PCI algorithms using coronary physiology. Recently, the 2023 ESC guidelines for acute coronary syndromes (ACS) (8) suggest considering adjunctive tests other than angiography alone to guide revascularization, such as intravascular imaging and intravascular physiology (class IIa). Those tests are also indicated in the evaluation of the non-culprit lesion in the non-ST elevation myocardial infarction setting (class IIb) during the index procedure (class IIb). The new ACS guidelines also recommend using intravascular imaging when assessing the hemodynamic relevance of ambiguous culprit lesions (Class IIb).
|
Table 1. Coronary physiology assessment: pros and cons |
||
|
Methods |
PROS
|
CONS
|
|
FFR |
Quick assessment of the damping pressure across the stenosis |
Hyperemia-based à needs adenosine infusion |
|
iFR |
Does not need hyperemia |
Might not evaluate the effective coronary flow reserve (non-hyperemic method) |
|
Virtual FFR based on angiography |
Pre-PCI simulation, evaluation of the pressure among the vessel |
Inaccurate computed segmentation that might lead to errors |
|
Virtual FFR based on CCTA |
Does not need invasive angiography |
Possible artifacts on the image, multiple factors might overestimate the degree of the stenosis (e.g. calcific stenosis) |
|
CCTA - coronary computed tomography angiography, FFR - fractional flow reserve, iFR - instantaneous wave-free ratio |
||
On the other hand, functional assessment of the infarct-related artery (IRA) is not recommended for ST-elevation myocardial infarction: in the acute setting, FFR might underestimate the degree of the culprit coronary stenosis (9).
The two invasive functional tests guiding the first functional assessment of coronary stenoses are iFR and FFR (Table 1).
FFR is defined as the pressure distal to a stenosis relative to the pressure before the stenosis (10). An FFR value of < 0.8 indicates a functionally severe stenosis. FFR measurements must be obtained during a period of maximal blood flow or maximal hyperemia. To achieve that, a hyperemic stimulus is administered intravenously or intracoronary through the guide catheter, and FFR is monitored for 3 to 4 minutes. Intravenous adenosine is the most widely used method to induce maximal hyperemia.
One of the most used methods is iFR, which is calculated by measuring through a guidewire the pressure gradient across the coronary lesion during the diastolic phase of the cardiac cycle.
Non-hyperemic pressure ratio measurements have been validated in previous studies with a standard threshold of 0.89. They might overestimate the hemodynamic significance of some lesions but remain useful whenever hyperemic agents are contraindicated (11). Longitudinal physiological vessel analysis is obtained utilizing a pressure wire pullback. With dedicated softwares, it is possible to assess pressure loss patterns across the vessel, differentiating between diffuse and focal disease. iFR is extremely useful when evaluating CAD in patients presenting multiple stenoses in a single coronary artery, which look hemodynamically similar to coronary angiography but have a different functional meaning in the coronary circulation. Thus, this aspect is crucial in terms of treatment decisions because some patients may not have indication for PCI at all if a vessel has diffuse plaques, while others may benefit from PCI if they have a focal disease pattern. Hence, when evaluating tandem coronary stenoses, longitudinal physiological vessel analysis is helpful to analyze the single stenosis to treat only the flow-limiting ones. Quantitative flow ratio (QFR) is a novel method to assess the hemodynamic relevance of coronary lesions based on a three-dimensional vessel reconstruction and estimation of its contrast media flow velocity (12). It does not require pressure wires, drug-induced hyperemia, or an angiography-based approach. QFR is also applicable to coronary computed tomography angiography, which has the advantage of being a non-invasive imaging exam; this allows for assessing the functional features of coronary lesions before coronary angiography, so the physician may decide earlier which treatment is most appropriate for the patient (e.g., medical therapy, PCI, cardiac surgery). The functional aspect of coronary imaging also occurs in PCI simulation, in which it is possible to predict hemodynamic results of a PCI.
Similarly, a post-PCI assessment can be conducted. When associated with intracoronary imaging techniques like intravascular ultrasound (IVUS), this approach enhances understanding of the hemodynamic enhancements due to the coronary angioplasty. Furthermore, post-PCI evaluation helps in detecting potential suboptimal PCI outcomes due to complications such as stent malapposition, stent underexpansion, plaque protrusion, or intrastent thrombosis. These complications cannot be adequately characterized by coronary angiography alone.
In conclusion, the study of coronary physiology serves a dual purpose:
First, in the pre-procedural setting, it aids in assessing lesion features, distinguishing between focal and diffuse diseases, identifying the most hemodynamically significant stenosis, and guiding optimal treatment decisions, including through the use of PCI simulations.
Second, in the post-PCI phase, it optimizes the results by detecting potential issues arising from suboptimal PCI, potentially undetected through classical angiography alone.
Peer-review: Internal
Conflict of interest: Giuseppe Biondi-Zoccai has consulted for Amarin, Balmed, Cardionovum, Crannmedical, Endocore Lab, Eukon, Guidotti, Innovheart, Meditrial, Microport, Opsens Medical, Terumo, and Translumina, outside the present work.
All other authors report no conflict of interest.
Authorship: D.M., L.S., K.G., G.B.-Z. and M.B. equally contributed to the preparation of manuscript
Acknowledgement and funding: None to declare
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

