Complications of endoscopic ligation of varicose veins in patients with portal hypertension
ORIGINAL RESEARCH ARTICLE
Complications of endoscopic ligation of varicose veins in patients with portal hypertension
Article Summary
- DOI: 10.24969/hvt.2023.420
- Page(s): 306-311
- Cardiac Surgery
- Published: 10/09/2023
- Received: 11/02/2023
- Revised: 14/08/2023
- Accepted: 30/08/2023
- Views: 6008
- Downloads: 3754
- Keywords: esophagus, esophageal varices, endoscopic ligation, endoscopic ligator
Address for Correspondence: Talgat A. Abdykadyrov, Department of Hospital Surgery, Faculty of Medicine, KRSU, Bishkek, Kyrgyzstan ORCID: 0000-0003-2029-5742
Bahadyr H. Bebezov, Talgat A. Abdykadyrov.
Department of Hospital Surgery, Faculty of Medicine, KRSU, Bishkek, Kyrgyzstan
Objective: The aim of the investigation is to analyze the results of endoscopic varicose vein ligation (EVL) in patients with portal hypertension; to estimate the character and frequency of early and late postoperative complications after EVL; to evaluate the possibility of endoscopic ligation at the moment of active bleeding.
Methods: This work includes an analysis of 138 procedures for endoscopic ligation of the esophageal varices in 111 patients from 2016 to 2020. Intrahepatic form of portal hypertension was in 90 patients, extrahepatic form - in 21 patients. The total number of interventions performed was divided into 2 groups. In the first group of patients with EVL was performed urgently, and the second group includes patients, if necessary, with targeted prescription and secondary prevention of portal esophageal bleeding.
Results: In 74 (53.6%) cases out of 138, different types of complications were detected. There were 2 lethal cases (1.4%). It should be noted that there were no lethal outcomes in second group after EVL, and after urgent operations, the mortality rate was 33.3%. The most critical complication of ligation was the resumption of hemorrhage due to the site of ligation in the early (1-3 days) and late periods after surgery (5-10 days).
Conclusion: In this analysis of the studied cases of complications after EVL, the most common complication was pain syndrome and early and late bleeding were also identified. We showed that control esophagogastroscopies helped to identify bleeding recurrences; examination algorithms in case of detection of bleeding complication after EVL, and measures to prevent the development of recurrent hemorrhage were also necessary.
Key words: esophagus, esophageal varices, endoscopic ligation, endoscopic ligator
Introduction
Currently, endoscopic hemostasis is the method of choice in the treatment of patients with bleeding from esophageal varices (EV) (1, 2). Endoscopic ligation of esophageal varices (EVL) with latex rings developed by G.V. Stiegmann in the mid-80s in the USA and ligators with nylon loops developed in Japan in the beginning and middle 90s of the last century are the most widely used in our clinic (3, 4). As endoscopic interventions experience in patients with portal hypertension (PH) has been the accumulated, it becomes possible to analyze the risks and complications of endoscopic interventions, to propose a treatment algorithm for recurrent esophagogastric bleeding.
The aim of the investigation is to analyze the results of EVL in patients with portal hypertension; to estimate the character and frequency of early and late postoperative complications after EVL; to evaluate the possibility of endoscopic ligation at the moment of active bleeding.
Methods
Study design: a cohort study.
Study population: During the period from 2016 to 2020, 138 sessions of EVL were performed in 111 patients with PH syndrome.
The total number of interventions was divided into 2 groups. In the first group were patients with urgent EVL, and in the second group were the patients who underwent the intervention for primary and secondary prevention of esophageal bleeding of portal genesis.
All patients provided informed consent for all procedures.
Clinical evaluation
We collected and analyzed the following variables: demographic as age and sex, etiology of portal hypertension, duration of hospitalization and complications of EVL: early and late bleeding recurrence, pain syndrome, dysphagia, liver failure, bleeding from an esophageal ulcer, ligature slippage and bleeding, and hyperthermia, and outcome as liver transplantation and mortality.
In addition, clinical and biochemical blood tests, ultrasound of the abdominal organs, ultrasound of the portal system were taken to establish the patient's diseases severity.
Esophagogastroduodenoscopy
Esophagogastroduodenoscopy remains the only method for diagnosing EV bleeding; EGDS was performed to all patients regardless of the presence or absence of signs of ongoing EV bleeding.
To establish the diagnosis and to determine the localization of the bleeding site, esophagogastroduodenoscopy (EGDS) was performed using video endoscopy system "Olympus CV-V1 Axeon" or fibrogastroscope Olympus "GIF E" (Japan).
This examination was performed immediately or within the first hours after hospitalization. To evaluate the severity of varicose veins, we used the three-degree classification of varices developed by A.K. Yeramishantsev and co-authors in 1986, according to which vein dilatation of the I degree is considered to be up to 3 mm, II degree - 3-5 mm, III degree - 5 mm and more.
Endoscopic varicose vein ligation
EVL is performed in the following way: after evaluation of varices condition, the gastroscope is removed from the esophagus and a ligator in the form of a cylinder loaded with latex ring is placed on its distal end, the gastroscope is reintroduced into the esophagus, an enlarged vein or an enlarged nodule is visualized, then starting from the cardioesophageal transition this vein is aspirated inside the cylinder and a latex ring is dropped on its base, thus the vein is bent and clamped. As a result, the blood flow through this vein is completely stopped (Fig. 1.). The practice of EVL at the height of bleeding was introduced in our clinic for patients with signs of ongoing bleeding. In order to improve visualization and determine the source of bleeding, EGDS was performed in the operating room with anesthetic support; the patient was lying on his left side with the head end elevated to 35-45º. In this position, bleeding blood drains into the stomach without filling the esophageal lumen, additional lavage allows clear identification of the bleeding varices, which can then be ligated. After hemostasis was achieved, the correctness of the ring was assessed; if in doubt, a second ring was placed on this node.
Surgical interventions were also performed using the Olympus CV-V1 Axeon video endoscopic system and the Olympus GIF E fibrogastroscope (Japan) and four types of ligators:
1. Cook Medical's ligator (6 Shooter® Universal Saeed® Multi-Band Ligator) (Fig. 2).
2. Olympus ligator (Quick-Loop reusable ligator device, reusable basket and ligator handle, MAJ-339 disposable plastic loop) (Fig. 3).
3.Sumitomo Bakelite pneumatic ligator (Endoscopic Esophageal Varix Ligation Device) (Fig. 4)
4.Modified Stigman-Goff ligator (Kyrgyzpatent utility model patent No. 290 dated 11/22/2011. (Device for IVL ligation for portal hypertension) (Fig. 5).
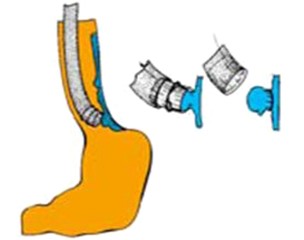
Figure 1. Endoscopic varices ligation
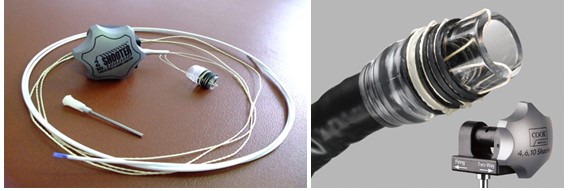
Figure 2. Cook Medical's ligator (view before and after assembly)

Figure 3. Olympus ligator

Figure 4. Sumitomo Bakelite pneumatic ligator

Figure 5. Modified Stigman-Goff ligator
Protocol of treatment
When a patient with bleeding signs was admitted to the emergency room the blood hemoglobin level, liver, kidney function indices were determined urgently, and simultaneously EGDS was performed in the operating room. After the source of bleeding had been identified, EVL was immediately performed (5, 6). At the same time a central or peripheral vein was catheterized, after which the patient was administered hemostatics, proton pump inhibitors, and transfusion of blood components (fresh frozen plasma, red blood cell mass) was performed. In patients with no signs of bleeding, the EVL was performed routinely.
To prevent early and late recurrence of bleeding in our clinic the patient was prescribed strict bed rest for 1 day and 6 hours after the procedure; he was allowed to drink cold liquids in small portions and to eat ice cream in small portions. Hemostatics, proton pump inhibitors, hepatoprotectors, enveloping agents with benzocaine were administered parenterally to relieve pain syndrome. On the 2nd day the patient was prescribed semi-bed rest mode, nutrition - broths, liquids, propranolol, diuretics in the presence of ascites were added. On the 3rd day, the patients were prescribed a general regime, table №5 by Pevzner diet, but meals were given only in mashed form.
Statistical analysis:
Data are presented as number, percentage.
Results
There were 61 men and 50 women, and the age of the patients ranged from 8 to 70 years.
Six patients were admitted to the clinic with signs of active EV bleeding. In 138 cases they were routinely hospitalized, all of them were hospitalized due to the high risk of EV bleeding after routine EGDS.
Out of 111 patients, 90 (81.1%) were diagnosed with liver cirrhosis (LC), of which viral hepatitis B -8(7.2%), viral hepatitis B with delta agent - 27(24.3%), viral hepatitis B+C - 1(0.9%), viral hepatitis B with delta agent + C - 1(0.9%), viral hepatitis C - 20(17.5%) were the cause of cirrhosis; LC developed as the outcome of autoimmune hepatitis was detected in 2(1.8%), hepatitis of unknown etiology - 30(27.0%), and alimentary etiology - 1(0.9%); 21(18.9%) of patients had extrahepatic form of portal hypertension (Table 1).
|
Table 1. Distribution of patients by etiological factor |
||
|
Etiology of portal hypertension |
Patients (n =111) |
|
|
n |
% |
|
|
LC due to viral hepatitis B, |
8 |
7.2 |
|
LC due to viral hepatitis B+D, |
27 |
24.3 |
|
LC due to viral hepatitis C, |
20 |
17.5 |
|
LC due to viral hepatitis B+C, |
1 |
0.9 |
|
LC due to viral hepatitis B+C+D |
1 |
0.9 |
|
LC due chronic hepatitis of unspecified etiology |
30 |
27.0 |
|
LC due to autoimmune hepatitis, |
2 |
1.8 |
|
LC due to toxic hepatitis, |
1 |
0.9 |
|
Anomaly of portal vein development |
19 |
17.1 |
|
Thrombosis of portal vein |
1 |
0.9 |
|
Alveococcosis of the liver with compression of the portal vein |
1 |
0.9 |
|
LC- liver cirrhosis |
||
EVL and its complications
Overall 138 sessions of endoscopic ligation were performed in 111 patients, complications were registered after 74 (53.6%) procedures, and the most dangerous complications as recurrence of bleeding were 3 (2.2%). During the procedure at the moment of varices aspiration, there was a rupture of subepithelial telangiectasias, the so-called "supervariax", to prevent ring slippage an additional ring was put on this varix, which allowed to achieve reliable hemostasis.
|
Тable 2. Type and number of complications of endoscopic esophageal varices ligation |
||
|
Type of complication |
Number of complications of EVL (n=74) |
|
|
Urgent |
Routine |
|
|
Liver failure, n(%) |
1(1.3) |
0(0) |
|
Bleeding of an esophageal ulcer, n(%) |
1(1.3) |
0(0) |
|
Ligature slippage and bleeding, n(%) |
2(2.6) |
0(0) |
|
Pain syndrome, n(%) |
1(1.3) |
36(48.6) |
|
Hyperthermia, n(%) |
1(1.3) |
32(43.2) |
|
Total, n(%) |
6(8.1 |
68(91.9) |
The most serious and life-threatening complication of the procedure is bleeding from the ligated esophageal varices. In our practice, this complication occurred after 4 (2.9%) procedures. Bleeding recurrences after endoscopic ligation are divided into early and late.
Patients with early bleeding recurrence underwent urgent esophagoscopy and the cause of bleeding was found to be ligature slippage from the esophageal varicose vein hemorrhage when coughing or vomiting. This complication occurred in 3 (2.2%) cases. EVL with the application of rings below the bleeding site was performed repeatedly in two patients, thus, final hemostasis was achieved. One patient died of disseminated intravascular coagulation syndrome despite the use of the obturator tube.
Late recurrence of bleeding after endoscopic ligation (5-10 days) was noted in 1 (0.7%) patient, considering the pronounced encephalopathy, hemostasis was achieved by conventional conservative hemostatic therapy.
Another patient (0.7%) died of liver failure, with no signs of recurrent bleeding.
Pain syndrome was the main complication after the ligation. Besides bleeding from the ligation site, pain syndrome in esophageal projection was reported in 37 (26.8%) cases. Pain intensity was moderate and lasted for 1 to 6 days. The pain syndrome was controlled by intravenous administration of narcotic and non-narcotic analgesics. In 33(23.9%) cases there was an increase in temperature to subfebrile digits, hyperthermia normalized without correction (Table 2).
Duration of hospitalization was 7.7 days.
Liver transplantation and mortality
Of all the observed patients, three patients underwent liver transplantation after discharge, 4(2.8%) died of liver failure, and one died in the department from profuse esophageal bleeding 3 years after the last EVL session. After EVL of esophageal varices, 2 (1.4%) patients died in the early postoperative period.
Discussion
Our results demonstrated that pain syndrome is the most common after EVL, we also observed development of early and late bleeding. Our results are in the agreement with those reported in literature (5-7).
The analysis of the treatment results allowed us to draw up an algorithm of treatment measures in case of complications after EVL. Early and late bleeding from EVL sites is a major complication that a clinician should pay attention to and undertake urgent measures to stop it (7). In our observation, the cause of early bleeding recurrence was the ring slippage and the cause of late recurrence was bleeding from an ulcer formed after ligation and ring rejection.
In the meantime, we performed measures to stabilize hemodynamics. Patients with decompensated cirrhosis in extremely severe condition did not undergo EVL. Taking into account the presence of complications after the EVL, in-patient treatment was 7.7 bed days. The first control EGDS was performed between 2 and 3 weeks after the procedure. Follow-up EGDDs were performed 3, 6, 9 and 12 months later. Then if there was no recurrence of varices - twice a year. Ligation was performed routinely if a recurrence of bleeding was detected.
Based on the analysis of the study data, EVL is the method of choice for the treatment of complications of portal hypertension syndrome such as hemorrhage. In addition, this manipulation should be performed by a specialist with experience, to reduce the percentage of early and late complications. If the operator is sufficiently experienced, such endoscopic interventions can be performed at the height of the bleeding. EVL prevents recurrence of bleeding in more than 90% of patients (8).
Study limitations
The main limitation is the descriptive nature of our study.
Conclusion
In this analysis of the studied cases of complications after EVL, the most common complication was pain syndrome and early and late bleeding were also identified. We showed that control esophagogastroscopies helped to identify bleeding recurrences; examination algorithms in case of detection of bleeding complication after EVL, and measures to prevent the development of recurrent hemorrhage were also necessary.
Ethics: All patients provided informed consent for all procedures
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: B.H.B. and T.A.A. equally contributed to the study and preparation of manuscript
Acknowledgement and funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

