Evaluation of the possibility of using spectral analysis of a single-channel ECG for the diagnosis of diastolic dysfunction of the left ventricle of the heart
ORIGINAL RESEARCH ARTICLE
Evaluation of the possibility of using spectral analysis of a single-channel ECG for the diagnosis of diastolic dysfunction of the left ventricle of the heart
Article Summary
- DOI: 10.24969/hvt.2023.424
- Page(s): 329-337
- CARDIOVASCULAR DISEASES
- Published: 05/10/2023
- Received: 24/07/2023
- Revised: 20/09/2023
- Accepted: 20/09/2023
- Views: 6104
- Downloads: 3849
- Keywords: preclinical diagnosis of chronic heart failure, diastolic dysfunction of the left ventricle, Doppler echocardiography, electrocardiogram, spectral analysis of a single-channel electrocardiogram
Address for Correspondence: I.K.Moldotashev, 720020, Bishkek, Baytik Baatir st. 1/ 4, fl.12. Bishkek, Kyrgyzstan
E-mail: moldotashev53@mail.ru Phone: 996550302053
Ishenbay K. Moldotashev -ORCID: 0000-0001-5525-3599 Yuriy A. Bogdanov - ORCID: 0000-0002-8289-6888
A.A. Sorokin - ORCID: 0000-0002-9682-8085
Ishenbay K. Moldotashev 1, Yuriy A. Bogdanov 2, Alexander A. Sorokin3
1ADAM University, Bishkek, Kyrgyzstan
2Hebei DSF Geos Technology Co., LTD, China, Kharkiv, Ukraine
3Institute of Mountain Physiology and Medicine, National Academy of Sciences of the Kyrgyz Republic, Bishkek, Kyrgyzstan
Abstract
Objective: Assessment of diastolic function of the left ventricle (LVDF) makes it possible to detect chronic heart failure (CHF) at the preclinical stage of development, when its progression can still be prevented. Doppler echocardiography (echo) is the most accurate non-invasive diagnostic method for left ventricular diastolic dysfunction (LVDD), requiring expensive equipment and trained professionals. The development of an accessible screening method for the diagnosis of LVDD is an urgent and practically significant task.
Purpose of the study was to evaluate the diagnostic value, sensitivity and specificity, positive predictive value and negative predictive value of the method of spectral analysis of a single-channel electrocardiogram (S-ch ECG) proposed by us for the diagnosis of LVDD in comparison with Doppler echo as a reference.
Methods: The study involved 60 people (35 patients on program hemodialysis with arterial hypertension and 25 healthy individuals). Among the patients there were 19 men and 16 women aged 29 to 65 (45.9 (12.8)) years. Among the healthy were 15 men and 10 women aged 25 to 63 (43.2(11.8)). Doppler echo was performed on the SonoSite Micro Maxx Belse X2 apparatus. LVDF was determined according to the generally accepted method. S-ch ECG was taken with portable recorder DuoEK 118 from Lepu Medical. LVDD was determined by S-ch ECG spectral analysis as the ratio of the sum of harmonic power in the period of early diastolic filling to the sum of harmonic power during the period of atrial contraction.
Results: The sensitivity of the method developed by us was 0.74, and the specificity was 0.84. Positive predictive value was 0.87 and negative predictive value was 0.70. Chi-square: 15.043, p<0.0001 - the presence of a relationship is statistically highly significant; Phi=0.514, p<0.0001 - the presence of a connection is highly significant. Area Under the Curve is 0.791 (0.061) with a confidence interval of 0.672 to 0.911. The obtained values indicate that S-ch ECG scores are fairly good predictors of LVDD.
Conclusion: Spectral analysis of S-ch ECG has a high sensitivity and sufficient specificity for the diagnosis of LVDD. This method can be used for remote mass screening studies for the purpose of preclinical diagnosis of CHF.
Key words: preclinical diagnosis of chronic heart failure, diastolic dysfunction of the left ventricle, Doppler echocardiography, electrocardiogram, spectral analysis of a single-channel electrocardiogram
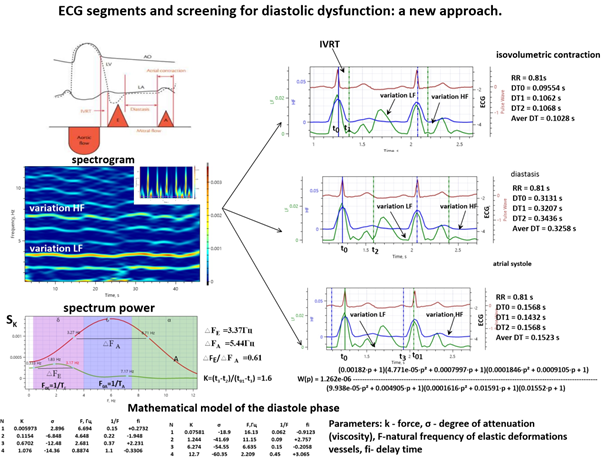
Graphical abstract
Introduction
Chronic heart failure (CHF) is the outcome of almost all cardiovascular diseases. Its prevalence increases with age, from about 1% for people under 55 years of age to over 10% for people aged 70 years and older. Its causes in most cases are coronary heart disease and arterial hypertension (1). A study combining the Framingham Heart Study and the CVD study cohorts reported a mortality rate of 67% within 5 years of CHF diagnosis (2).
From the point of view of modern ideas about the cardiovascular continuum, cardiovascular diseases occur under the influence of risk factors and then steadily progress, eventually complicating CHF. At the same time, left ventricular diastolic dysfunction (LVDD) is first detected as a compensatory reaction to an increase in pressure in the left ventricle and / or the development of atherosclerotic cardiosclerosis, which later turns into diastolic heart failure, when clinical signs of CHF already appear. This stage is called CHF with a preserved left ventricular ejection fraction (LVEF), which can last for quite a long time, subsequently being complicated by systolic heart failure, leading to a tragic ending (3). To prevent the progression of CHF, it is very important to diagnose it at the stage of LVDD, when therapeutic and prophylactic interventions are most effective. Currently, for this purpose, the Doppler echocardiography (echo) in various modifications is widely used in clinical practice. In this paper, we studied the possibility of using spectral analysis of a single-channel electrocardiogram (S-ch ECG) to diagnose LVDD, comparing it with Doppler echo as a reference.
Purpose of the study was to evaluate the diagnostic value: sensitivity and specificity, positive predictive value and negative predictive value of the method of spectral analysis of a S-ch ECG proposed by us for the diagnosis of left ventricular diastolic dysfunction in comparison with Doppler echo as a reference.
Methods
Study design and population
This is the study on diagnostic accuracy of spectral analysis of S-ch ECG in prediction of LVDD.
The study involved 60 people (35 patients on program hemodialysis with arterial hypertension and 25 practically healthy individuals). Among the patients were 19 men and 16 women aged 29 to 65 (45.9(12.8)) years. Among the healthy were 15 men and 10 women aged 19 to 30 (23.2 (2.8)) years. We have obtained the approval of the University Ethics Council for the study protocol, and declare that the planning, conduct, presentation of the study involving humans and the procedures used in the study are in accordance with the Declaration of Helsinki as amended in 2013. Informed consent from patients for the procedures performed in the study was obtained.
Among patients with chronic renal failure receiving program hemodialysis, 35 patients with LVDD diagnosed by Doppler echo were selected for the study. All patients received antihypertensive therapy due to arterial hypertension. The selected patients had no cardiac arrhythmias or conduction disturbances.
We assessed age, sex and blood pressure of patients and controls.
All patients immediately after the Doppler echo study had a single-channel ECG taken for one minute and sent via a chat bot for spectral analysis. Similarly, Doppler echo and S-ch ECG were taken in healthy individuals.
Echocardiography and Doppler echocardiography
Echo and Doppler echo were performed on the Sono Site Micro Maxx Belse X2 apparatus. We evaluated end diastolic size of left ventricle (LV), end systolic size of LV, LVEF, diameter of the aorta, left atrial size, interventricular septum thickness, LV posterior wall thickness, ratio of early and late velocity of mitral blood flow (E/a), size of the right ventricle and average pulmonary arterial pressure.
Left ventricular diastolic function (LVDF) was determined according to the generally accepted method (4).
Spectral analysis of S-ch ECG
S-ch ECG was taken with portable recorder Duo EK 118 from Lepu Medical (Fig. 1).
The LVDD using spectral analysis of the ECG was determined as the ratio of the sum of the power of harmonics in the period of early diastolic filling to the sum of the power of the harmonics in the period of atrial contraction within a given time interval. An improved Bartlett and Welch method (5) was used for temporal averaging.
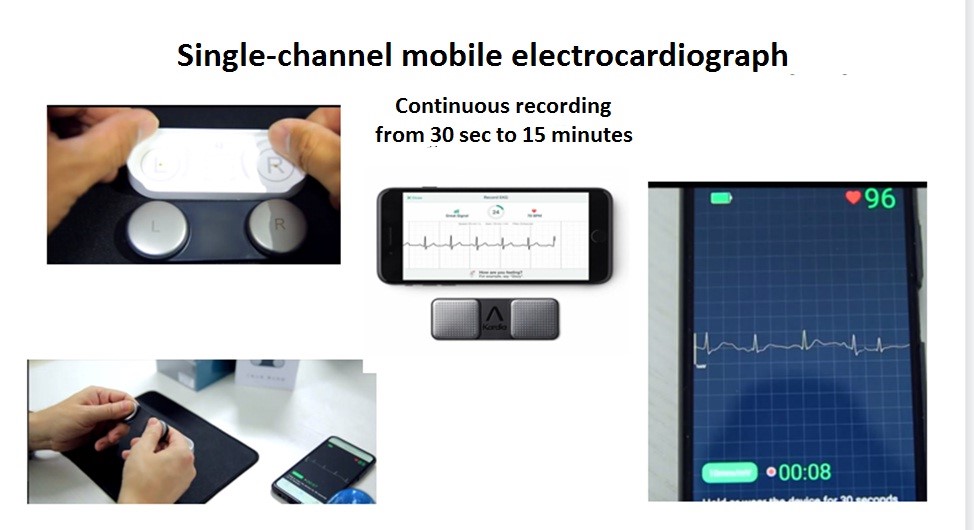
Figure 1. A single-channel mobile cardiograph is used to take an ECG from the fingers, followed by signal transmission via a smartphone to a center for spectral analysis
Where, the time series of the ECG recording is divided into overlapping segments. Then a modified periodogram is calculated for each segment, and then these estimates are averaged to obtain an estimate of the power spectral density of the signal.
The most common representation of a spectrogram is a two-dimensional diagram: the horizontal axis represents time t, the vertical axis represents frequency F; the third dimension - the power at a certain frequency at a particular point in time is displayed by the brightness or color of each point of the image (Fig. 2).

Figure 2. Typical view of the ECG spectrogram (on the left) and diagram of the time delay of the spectral power of signals of low frequency LF variability relative to high frequency HF (on the right)
Thus, the cardiosignal processing algorithm is based on the principle of selecting variations in broadband signals of the cardiogram low frequency (LF) of the time series components, high frequency (HF) variational cycles and determining their delay relative to each other (signal response delay). Average time delay between the first maximum of the variability of the spectral power of signals (HF), coinciding in time with the R-wave and the neighboring maximum of variability (LF) of the vascular system of the body determines the interval of isovolumetric contraction of the heart (Fig. 2). It is typical that the time is formed by the cardiovascular system itself and is its main property.
In view of the inertia of the walls of the vessels, the achievement of the highest pressure value occurs with a time delay. At the same time, stretching of the walls is accompanied by their tension and a concomitant increase in the intensity of the cardiosignal. In this case, the intensity signal changes its shape, which is reflected in the spectral composition of the radiation and, accordingly, in the variability of the spectral power of the signals (LF) and (HF) of the vascular system of the body. Thus, both diastole and systole phase signals are present in the ECG signal spectrum. On the graphs of the spectral power, this manifests itself in the form of two-level vertices (Fig. 3).
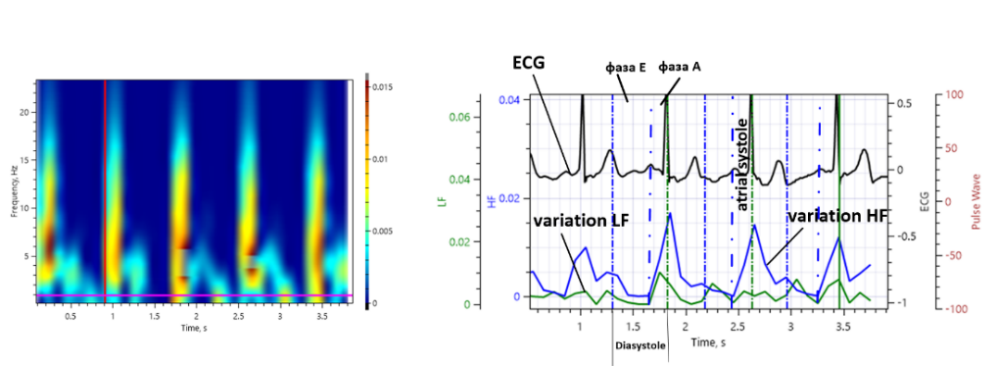
Figure 3. A typical view of the S-ch ECG spectrogram (on the left) with short segments of analysis and a diagram of the delay of the spectral power of the LF and HF variability signals (on the right)
Figure 3 shows how diastole and atrial systole intervals are determined. At these intervals, we obtain ECG signals of the power spectra for fragments of phase E and phase A, which is illustrated in Figure 4.
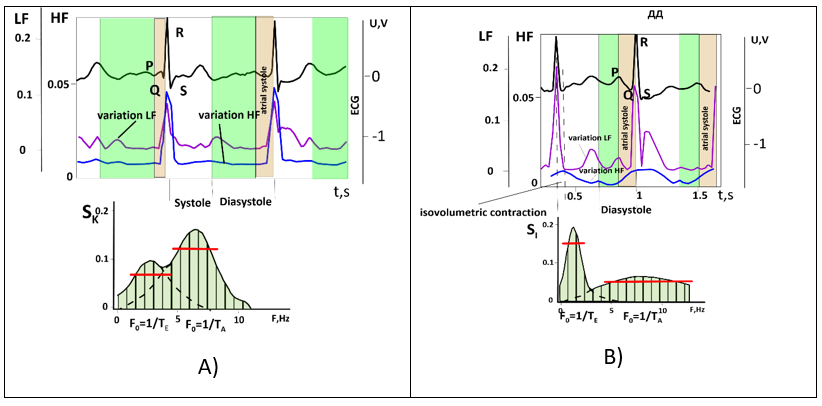
Figure 4. Diagram of sums of harmonic power during early diastolic filling and sum of harmonic power during atrial contraction: a) - for a healthy body, c) with signs of diastolic dysfunction, where TE, TA are the period of the fundamental harmonic of oscillations of the signal of phase E (early diastole) and A (atrial systole), respectively, FE and FA - frequencies of fundamental harmonics
LVDD was determined by ECG spectral analysis as the ratio of the sum of harmonic power during early diastolic filling (E) to the sum of harmonic power during the period of atrial contraction (A). If the E/A ratio was greater than 1, normal diastolic function was diagnosed, if less 1 that was determined as LVDD. The frequency intervals were determined by the width of the cardiosignal power at a level of 0.7 from the maximum value of the power spectrum of the E and A components in the vicinity of their fundamental harmonic frequencies F0=1/TE and F0=1/TA.
Statistical Analysis
The statistical analysis was conducted using IBM SPSS Statistics software version 26 (New York, USA). The differences between groups in continuous variables were compared using t test for independent samples and for comparison of categorical variables we used Chi-square test.
We calculated sensitivity, specificity, negative and positive predictive values of test using cross-tabulation method.
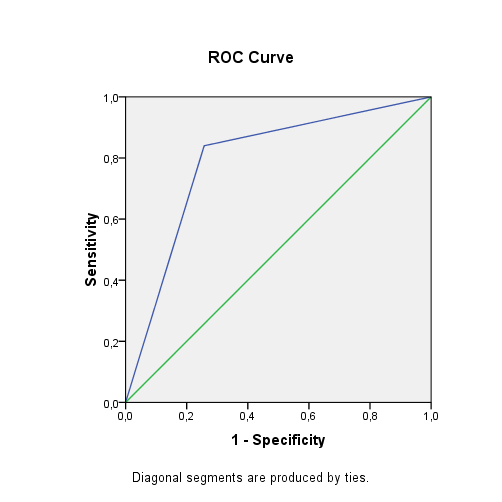
In order to determine the most effective classifier for diagnosis, receiver operating characteristics (ROC) curves were constructed and the area under the curve (AUC) was analyzed. ROC curves are a widely used method for evaluating the diagnostic performance of a test. By plotting the true positive rate (sensitivity) against the false positive rate (1 - specificity) for a range of cut-off values, the curve provides an estimation of the test's overall accuracy in distinguishing between the positive and negative cases. The AUC is a summary statistic of the ROC curve, with values ranging from 0.5 (indicating a random guess) to 1.0 (indicating perfect discrimination). The higher the AUC value, the better the diagnostic performance of the test. We compared categorical variables between groups using χ² and Pearson's phi tests, which are measures of the association between two dichotomous variables.
Results
Among the patients were 19 men and 16 women aged 29 to 65 (45.9(12.8)) years. Among the healthy were 15 men and 10 women aged 19 to 30 (23.2 (2.8)) years. Patients and healthy individuals did not differ significantly by sex, though healthy controls were younger, but did not reach statistical significance. According to Doppler echo data (Table 1), the patients had a statistically significant increase in systolic and diastolic blood pressures, mean pulmonary arterial pressure, all sizes of the heart, the thickness of the interventricular septum and the posterior wall of the LV were increased (p<0.0001 for all) as compared to healthy controls. An E/A ratio of 0.6 indicated the presence of LVDD of the heart in patients. According to echo, there were no signs of LVDD among healthy individuals.
|
Table 1. Blood pressure and Doppler echocardiography parameters of patients and healthy persons |
|||
|
Variables |
Healthy |
Patients |
p |
|
Systolic BP, mmHg |
110(12.7) |
140(21) |
< 0.0001 |
|
Diastolic BP, mmHg |
71(9) |
88(10) |
< 0.0001 |
|
End diastolic size of LV, mm |
48.2(2.3) |
50.4(3.4) |
0.012 |
|
End systolic size of LV, mm |
30.3(2.3) |
32.6(3.5) |
0.008 |
|
Ejection fraction of LV, % |
68.9(3.6) |
63.5(4.2) |
0.0001 |
|
Diameter of the aorta, mm |
28.2(1.9) |
32.1(2.2) |
< 0.0001 |
|
Size of the left atrium, mm |
26.0(2.0) |
34.0(3.6) |
<0.0001 |
|
Thickness of the interventricular septum, mm |
7.6(0.5) |
11.0(1.5) |
<0.0001 |
|
Thickness of LV posterior wall, mm |
8.3(0.5) |
11.4(1.3) |
<0.0001 |
|
E/A |
1.5(0.18) |
0.6(0.14) |
< 0.0001 |
|
Size of the right ventricle, mm |
18.1(1.8) |
20.8(3.0) |
<0.0001 |
|
Average pulmonary arterial pressure, mm |
21.7(2.5) |
26.9(4.6) |
<0.0001 |
|
Data are presented as mean (SD) BP – blood pressure, E/A - ratio of early and late velocity of mitral blood flow, LV- left ventricle |
|||
According to the results presented in the Table 2 the Sch-ECG test sensitivity is 0.74 , specificity - 0.84, positive predictive value - 0.87, and negative predictive value - 0.70.
|
Table 2. Cross-correlation table comparing the results of using Doppler echocardiography and the method of spectral analysis of a single-channel electrocardiogram for the diagnosis of diastolic dysfunction of the left ventricle
|
||||
|
|
Doppler echo |
|||
|
Yes LVDD |
No LVDD |
Total |
||
|
S-ch ECG |
Yes LVDD |
26 |
4 |
30 |
|
No LVDD |
9 |
21 |
30 |
|
|
Total |
35 |
25 |
60 |
|
|
echo – echocardiography, LVDD – left ventricular diastolic dysfunction, S-ch ECG - single-channel electrocardiogram |
||||
The ROC analysis (Fig. 5, Table 3) demonstrated that the sensitivity of the method developed by us was 0.74, and the specificity was 0.84 - Chi-square: 15.043, p<0.0001 - the presence of a relationship is statistically highly significant; Phi=0.514, p<0.0001 - the presence of a connection is highly significant. Area under the curve is 0.79 1(0.061) with a 95% confidence interval of 0.672 to 0.911. The obtained values indicate that S-ch ECG scores are fairly good predictors of LVDD.
|
Table 3. ROC analysis - area under the curve (AUC) estimates |
||||
|
Area |
Std. error |
Asymptotic Significance |
Asymptotic 95% Confidence Interval |
|
|
lower bound |
upper bound |
|||
|
0.791 |
0.061 |
p<0.0001 |
0.672 |
0.911 |
 oi
oi
Figure 5. The ROC curve of accuracy of S-ch ECG in diagnosis of LVDD (see Table 3 for statistics)
S-ch ECG – single channel electrocardiogram, LVDD – left ventricular diastolic dysfunction
Discussion
Diastolic dysfunction is a pathophysiological condition associated with impaired myocardial relaxation and/or decreased compliance of the left ventricle, leading to increased filling pressure in the left ventricle (6). At the beginning, it is compensatory in nature, but sooner or later the compensatory mechanisms are depleted, clinical symptoms of CHF appear, and the stage of diastolic heart failure sets in, which is now also called heart failure with preserved left ventricular ejection fraction (7, 8). However, it is important to understand that, although diastolic dysfunction is the main factor leading to the development of heart failure with preserved left ventricular ejection fraction, these terms are not interchangeable in the light of current understanding (9). Considering the inevitable progression of LVDD to diastolic and then to systolic heart failure, it becomes clear that preclinical diagnosis of CHF at the stage of diastolic dysfunction is necessary (10,11). The urgency of such a task also increases due to its high prevalence, from 20 to 36% in the population (3, 12). The value of diagnosing LVDD has also been proven for predicting the outcomes of cardiac surgery (13-15).
The most accurate diagnosis of diastolic dysfunction can be made invasively, but this method cannot be used for wide clinical practice (3, 7). Doppler echo is currently the most commonly used non-invasive tool in the assessment of LVDD (3, 4, 6). The identification of LVDD is based on a comprehensive assessment of a large number of echocardiographic parameters: the size and volume of the left atrium, the Doppler indicators of the transmitral flow and the flow of the pulmonary veins, data from tissue Doppler echocardiography, computed tomography and two-dimensional tracking of grayscale spots (speckle tracking imaging or 2D-strain) (6, 16-18). In general clinical practice, the Doppler echo method is most often used (19). This determines the ratio of the rate of early diastolic filling (E) to the rate of blood flow in the phase of atrial contraction (A). According to the E/A ratio, the degree of diastolic relaxation is assessed, which can characterize myocardial stiffness. According to the results of Doppler echo, LVDD is divided into 3 stages: 1) mild (grade I or Ia), defined as impaired relaxation without or with mild signs of increased filling pressure, respectively; 2) moderate (Grade II), defined as impaired relaxation associated with a moderate increase in filling pressure or pseudo-normal filling; and 3) severe, defined as marked reduction in compliance or reversible (grade III) or fixed (grade IV) restrictive filling (3).
Tagged cardiac magnetic resonance imaging (MRI) can be used as a non-invasive method to obtain information about myocardial deformity and assess LVDD (20). However, the limited temporal resolution of MRI, along with high costs, limits its widespread use.
Doppler echo methods also cannot be used for mass screening studies due to the need for expensive equipment and the need for trained specialists. In this regard, the evaluation of LVDD using ECG deserves attention. Holmqvist et al. (21) proposed to use the new Tend-P / (PQxAge ECG index for LVDD, the accuracy of which increases with the addition of the left atrial volume index. The disadvantage of this method is the need for joint use of ECG and echocardiography.
There are known studies that used 12-lead ECG data to detect CHF. In this case, such ECG parameters were taken into account as the P wave, fragmented QRS complex, ST-T segment, T wave (22-24). A machine learning model has been created to determine the LV diastolic pressure of the heart based on the wavelet transformation of a 12-channel ECG (25, 26 ).
Kuznetsova et al. (27, 28 ) used spectral analysis of a S-ch ECG to diagnose systolic and diastolic dysfunction of the left ventricle of the heart. The studied ECG parameters reflected the amplitude and temporal characteristics of the complexes, the energy of the ECG signal in the target zones of the complexes and asymmetry indices. ECG parameters were identified that have a high correlation with the presence of significant diastolic and systolic dysfunction of the left ventricle of the heart.
The method we propose for diagnosing LVDD is also carried out on the basis of spectral analysis of a S-ch ECG, but unlike the method of Kuznetsova and co-authors (27, 28), we measure frequency variations in the vicinity of the frequency ranges (HF) of the alpha rhythm and the reticular formation (LF) of selected cardiac cycles, which establish the intervals between the beginning of early filling of the LV and the beginning of atrial systole, as well as between the beginning of atrial systole and the beginning of the complex QRS. Then the spectral power of the ECG signal in these intervals is determined. Then the ratio of spectral power in the frequency ranges of early filling of the LV of the heart (E) and atrial systole (A) is calculated, which is used to estimate LVDF. Our proposed method has the following advantages: automatic determination of the onset and end of phase E and phase A, determination of the contribution of each harmonic to the total cardio-signal, which allows mathematical modeling of various pathological conditions of the body (29). The method of spectral analysis of S-ch ECG proposed by us has high diagnostic accuracy, high sensitivity and sufficient specificity for diagnosing of LVDD.
Study limitations
Our studies were conducted in patients with chronic renal failure who are on program hemodialysis and have LVDD of the heart according to Doppler echo data. Further research is needed in patients with cardiovascular diseases as hypertension, coronary heart disease, etc.
Conclusion
Spectral analysis of S-ch ECG has a good diagnostic accuracy, high sensitivity and sufficient specificity for the diagnosis of LVDD. This method can be used for remote mass screening studies for the purpose of preclinical diagnosis of CHF.
Ethics: All patients provided informed consent for all procedures
Peer-review: External and Internal
Conflict of interest: None to declare
Authorship: I.K.M., Y. A.B, A. A. S. equally contributed to the study, preparation of manuscript and fulfilled authorship criteria
Acknowledgement: We thank Mustafa Imran for technical assistance with the survey
Funding: We declare did not receive any material support for the study
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

