Clinical and ultrasound features of Mondor's disease of the breast: a case series
ORIGINAL RESEARCH ARTICLE
Clinical and ultrasound features of Mondor's disease of the breast: a case series
Article Summary
- DOI: 10.24969/hvt.2023.428
- CARDIOVASCULAR DISEASES
- Published: 22/10/2023
- Received: 10/08/2023
- Revised: 01/10/2023
- Accepted: 03/10/2023
- Views: 9913
- Downloads: 3787
- Keywords: Mondor's disease, breast, benign and malignant diseases of the breast, sonography, Doppler
Address for Correspondence*: Aliya Kadyrova, I.K. Akhunbaev Kyrgyz State Medical Academy, 92A, Akhunbaev str., 720020, Bishkek, Kyrgyz Republic
Email: al-kadyrova@yandex.ru ORCID: 0000-0002-5305-1042
Aliya Kadyrova*, Aziza Abdullaeva, Nurgasibat Musaeva, Begaim Kulbaeva, Kamilla Kozhanova, Aidana Medik Kyzy, Nurjan Sapharbek Kyzy
Radiology Department, Faculty of Medicine, I.K. Akhunbaev Kyrgyz State Medical Academy, Bishkek, Kyrgyz Republic
Abstract
Objective: Mondor's disease (MD) is a rare disease, more commonly known as thrombophlebitis of the superficial veins of the anterior chest wall. Patients with Mondor's disease, usually middle-aged women, have a cord-like, subcutaneous tender induration with or without infiltration of the skin and subcutaneous tissue that tends to resolve on its own within three to four weeks. However, these cases are fairly rare and the lack of clear diagnostic criteria makes them often misdiagnosed. In 50–60% of cases, no cause is identified (primary idiopathic disease), and in 40–50% of cases, some factors may be present, such as pregnancy or breast cancer.
We aimed to demonstrate case series of MD of the breast, as a replenishment of the clinical base of this pathology.
Methods: All patients underwent clinical examinations and breast sonography with triplex Doppler.
Results: We described the clinical and sonographic picture of thrombophlebitis of the superficial veins of the mammary glands in 5 patients with an idiopathic course, during pregnancy, and in combination with breast cancer to indicate clear diagnostic criteria.
Conclusion: Thus, the clinical cases presented in the article demonstrate different clinical features of Mondor's disease with a single outcome. The disease is a spontaneously regressive disease within one, rarely more than one month.
Key words: Mondor's disease, breast,
Introduction
Mondor’s disease is a benign, self-replicating condition of the breast, characterized by thrombophlebitis of the superficial veins of the breast area. The disease was first described by Faage in 1869 as a form of scleroderma. However, in 1939, the French surgeon Henri Mondor identified it as superficial thrombophlebitis, and the disease bears his name to this day.
MD has been described in the literature as a rare benign and self-limiting disease, but there is an opinion that this condition may be more common than reported. This is due to the fact that some patients, being in a panic, deliberately delay a visit to the doctor. Later they feel relieved due to rapid self-regression of the disease and do not seek medical care. The etiology and mechanism of development of MD are not fully understood yet. The frequency of cases in the population has not been established. However, few data in the literature highlights the incidence rate of 0.5–0.8%. This information is based on symptomatic manifestations and imaging features of the disease (1-3).
The condition most often occurs without any reason and can be confused with intercostal neuralgia, mastopathy, myositis or lymphangitis due to pain in the chest wall. Diagnosis of Mondor's disease is predominantly clinical based on a palpable subcutaneous painful cord-like mass, and sometimes are visible on the skin. Sonography is the method of choice not only for the primary diagnosis of Mondor's disease, but also for differential evaluation due to its higher spatial resolution than computed tomography and magnetic resonance imaging, and consequently has greater sensitivity (2-5). Sonography reveals MD as an enlarged superficial vein that looks like beads. Color Doppler or power Doppler are used for confirmation, which helps to evaluate quantitative and qualitative characteristics of blood flow.
The described pattern will easily help specialists avoid diagnostic errors associated with ductal ectasia (2) or lymphangiectasia. Sometimes it is possible to find a superficial anechoic cord-like structure with intraluminal thrombus that is seen as a persistent feeling defect on color Doppler (5-7).
Methods
We presented five clinical and sonographic cases of Mondor's disease of the breast, identified in females aged 25 to 56 years.
All patients underwent clinical examinations. Three cases were unilateral, and two cases were bilateral. Two of them were identified as independent diseases, the other two cases occurred during pregnancy, and the last one was presented with breast carcinoma combination. In all cases, the affected vein was palpated in the form of a cord-like structure of various sizes.
The idiopathic variant was detected accidentally, the patient had no complaints. The skin appeared normal; palpation of the dilated vein was painless. In two out of five cases, there was pain. In three out of five cases, there were signs of local tissue induration on the background of risk factors.
Sonography study of the breast was performed with a 7-9 MHz linear transducer using triplex Doppler.
Results and Discussion
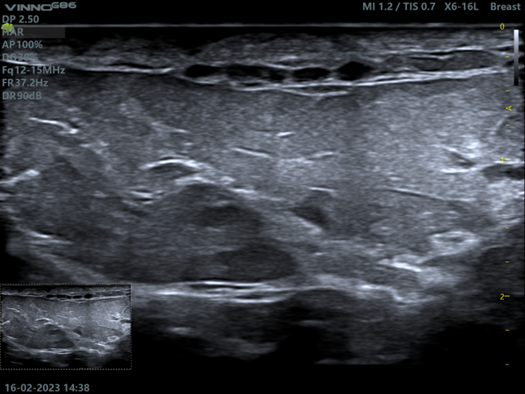
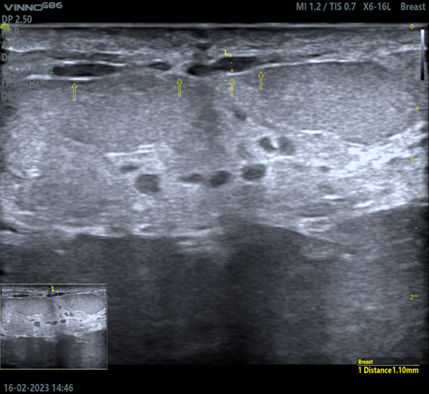
The first clinical case is an idiopathic MD: a 25-year-old patient presented to the clinic for breast ultrasound. She had no complaints; palpation of the breast was painless. The menstrual cycle is regular and painless. Scanning revealed small ductal ecstasies in the center of the upper and outer quadrants up to 2.5 mm in diameter. Additionally, in the center of the upper quadrants of the left mammary gland (at 12 o’clock) in the subcutaneous layer of the periareolar area, a painless anechoic beads-like structure (2.0 mm-22.0 mm in diameter) was determined. (Fig. 1). The skin and subcutaneous tissue remain with no signs of induration and thickening. Differential diagnosis of the dilated superficial vein and ductal ecstasies of the gland is shown on the sonogram (Fig. 2), the arrow points to the anterior layer of the split fascia: above the fascia, the anechoic structure is represented by the superficial vein, under the fascia - ductal ecstasies. Power Doppler mode helped to detect blood flow signals, but the spectral parameters were not identified due to extremely low blood flow. Physical examination revealed palpated vessels as painless small-caliber cords with a bluish tint.
|
|
|
|
Figure 1. In the subcutaneous layer of the periareolar region, an anechoic structure in the form of beads with a diameter of 2.0 mm, painless upon compression by the transducer, is determined (sagittal scan) |
Figure 2. The arrows indicate the anterior layer of the split fascia. The anechoic structure above the fascia is represented by an enlarged superficial vein, under the fascia - ductal ecstasies (sagittal scan) |
The patient was recommended to undergo a second ultrasound after 4 weeks. At the next appointment there were no signs of dilated veins, which were interpreted as a self-limited process with an idiopathic course (Fig. 3).
|
|
|
|
Figure 3. Re-examination of the first patient: the superficial vein is not dilated, under the fascia there are milk ducts with cystic changes |
Figure 4. Sonography of the soft tissues of the left anterior chest and lower quadrants of the left breast reveals subcutaneous anechoic beads-like structure consistent with superficial thrombophlebitis (sagittal scan) |
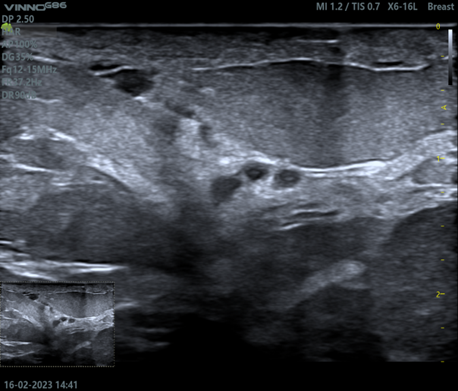
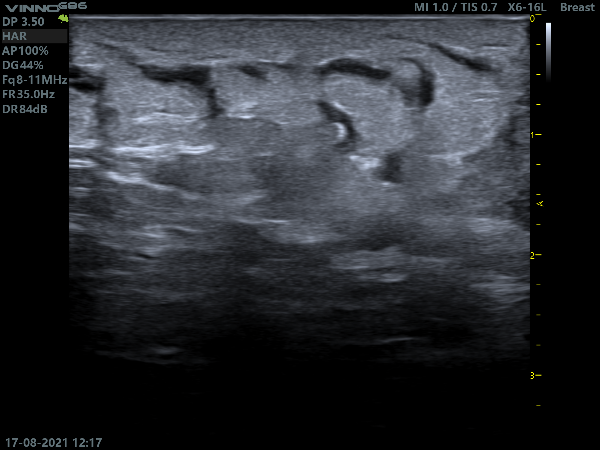
The second clinical case: a 34-year-old female presented to the clinic with complaints of a painful lump in her left breast. She felt discomfort during physical exertion a week ago, but for the last three days, she has started to feel pain. Physical examination revealed moderate erythema of the skin, which was extended from the level of the left costal arch towards the inner quadrant of the left breast, pastosity of skin was identified; a slightly painful cord-like structure (up to 3 mm in diameter) of a thick consistency was palpated.
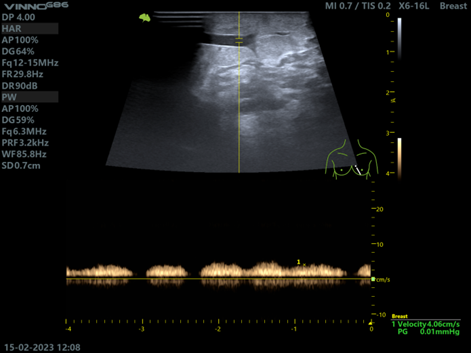
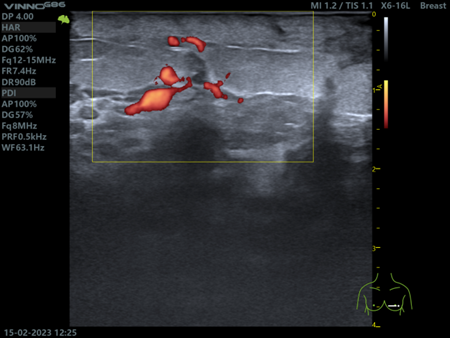
Ultrasound scan defined the palpable cord as an anechoic subcutaneous structure in the form of beads (Fig. 4), with Doppler mode, laminar venous blood flow was detected (Fig. 5). Soft tissues were moderately infiltrated, on ultrasound image appeared as hyperechoic, with lack of clarity of fascial layers. Axillary lymph nodes are not structurally changed.
|
|
Figure 5. Duplex ultrasound shows the laminar linear spectrum of blood flow is 1.8 cm/sec
The patient was diagnosed with Mondor's disease; she was referred to a mammologist and received anti-inflammatory therapy and local anticoagulant treatment. The patient applied for a follow-up examination 3 weeks later, where the previously identified dilated vein was not detected, soft tissues had no signs of infiltration, and palpation was painless.
The next clinical cases of MD include two pregnant patients, 25 and 28 years old, at 24 and 30 weeks of pregnancy, respectively. Clinical manifestations in both patients were the same: no complaints of pain, objective signs of bilateral inflammatory infiltration of the soft tissues of the lower quadrants of the breast and subareolar areas (Fig. 6).
|
|
|
|
Figure 6. Clinical manifestations represented by hyperemia, moderate swelling of the skin and no pain |
|

Figure 7. The affected vein of the left breast in the picture is visible along the edge of the areola in the form of a thin subcutaneous cord. Palpation caused pain. Signs of inflammatory infiltration are visible in the inner and lower quadrants
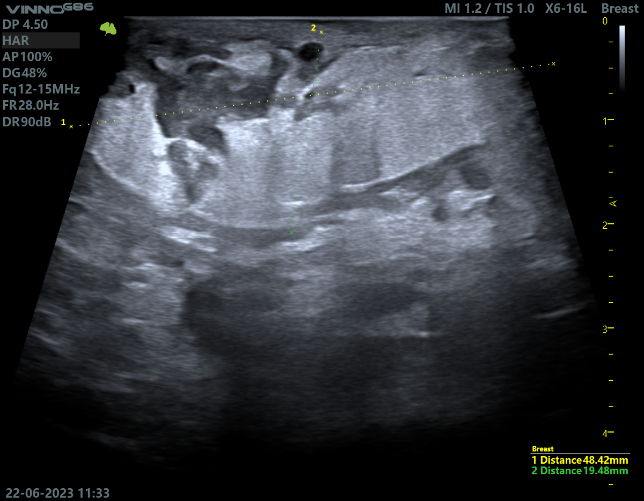
The 25-year-old patient had the last ultrasound examination six months ago. She was diagnosed with fibroadenoma of the left breast. With the onset of pregnancy, the patient underwent a control examination of the breast. On palpation, the right dilated vein was painless, pain was noted on the left breast (Fig. 7). Sonography revealed duct ecstasies: on the right side at 8 o'clock up to 4.6x2.8 mm in size; on the left at 9 o'clock - 17.3x4.1 mm; at 6 o'clock there is cluster type - 7.8x5.2 mm. At 8 o’clock and 2.5 cm from the edge of the areola, there was a fibroadenoma, measuring 6.7x3.0 mm, with no signs of progression. It was against this background, that signs of thrombophlebitis of the superficial veins in the form of cords in the lower quadrants of both breasts were determined. On the right breast, we identified cord-like structure, with length up to 15.0 cm and diameter up to 3.2 mm. The walls of the vein appear thickened, bloodstream was normal; there was a slight infiltration, moderate swelling of the skin (3.0 mm) and subcutaneous tissue (Fig. 8).
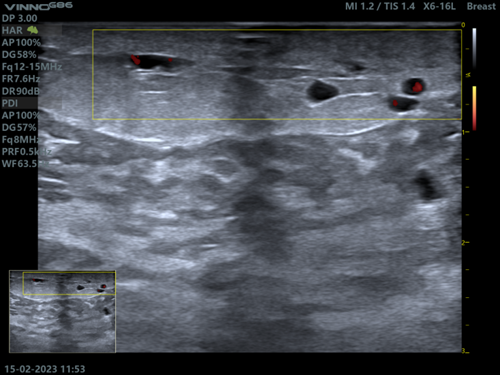
On the left side, in the center of the lower and outer quadrants there was uneven dilatation of the superficial vein with a diameter of up to 3.8 mm over its length with the low-velocity laminar blood flow (Fig. 9).
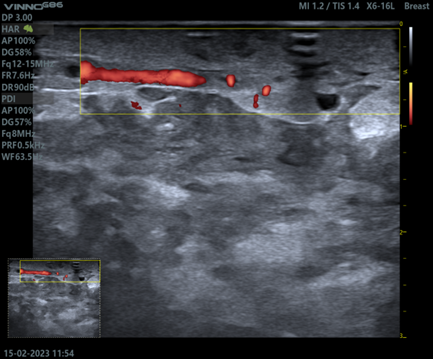
In the subareolar area of the left breast there was abnormal vein dilation 6.5x24.0 mm, there were no signs of thrombosis, the vein walls were uneven, and the blood flow could not be determined with spectral Doppler. This pattern, in view of the lack of knowledge, can be diagnosed as an enlarged duct, and against the background of skin inflammation (Fig. 10), especially in the absence of a color signal on Power Doppler. The dilated vein had a tortuous course going 17.0 mm deep from the skin surface, where it became thinner and disappeared (Fig. 11)
|
|
|
|
Figure 8. Infiltration, swelling of the skin and subcutaneous tissue against the background of tortuous enlarged vein.
|
Figure 9. Signs of thrombophlebitis of the superficial vein: tortuous, uneven walls, blood flow is identified |
|
|
|
|
Figure 10. The cystic pattern of the superficial vein can be mistakenly identified as an enlarged lactiferous duct, and in view of skin inflammation - as its infection |
Figure 11. On power Doppler a dilated tortuous vein at 17.0 mm deep from the skin surface, becoming thinner and disappearing |
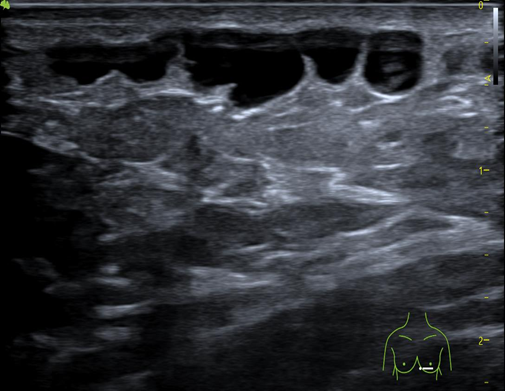
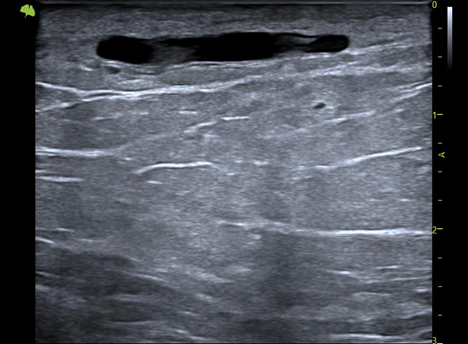
The patient was advised to use cold compresses and undergo further ultrasound studies to control the disease in 1.5 months. Ultrasound of the left breast revealed a thin superficial vein in the form of an anechoic linear structure above the fascia; under the fascia and posteriorly to the premammary tissue there was a complex of ductal ecstasies (Fig. 12).
|
|
|
|
Figure 12. Superficial vein in the form of an anechoic linear structure above the fascia; under the fascia and posteriorly to the premammary fatty tissue there is a complex of ductal ecstasies |
Figure 13. Signs of thrombophlebitis of superficial veins, thickening of the skin, edema of the subcutaneous tissues and fascia with the involvement of glandular tissue of the left breast |
The second pregnant patient from her medical history was suspected by her physicians to have breast cancer: an infiltrative-edematous form of breast cancer based on extensive infiltration and hyperemia of the skin surface of both breasts. Sonography studies of the lower quadrants and in the periareolar region on both sides revealed signs of thrombophlebitis of superficial veins with a diameter of 2.0 mm on the right and 2.5 mm on the left with low-velocity blood flow (2.1 cm/sec), thickening of the skin up to 5.6 mm, edema of the subcutaneous tissues and fascia with the involvement of glandular tissue, mainly on the left side (Fig. 13). This description of ultrasound examination does not correspond to suspicions of malignancy that demonstrates an insufficient acquaintance of physician about MD.
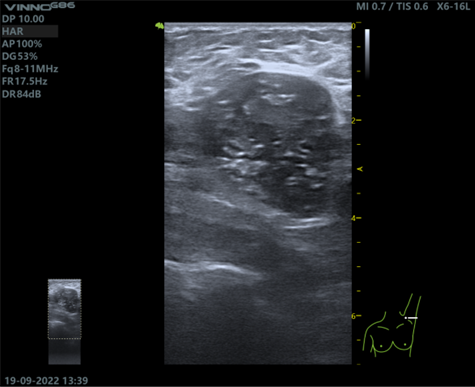
The final clinical case of MD is presented in a 56-year-old patient in combination with a diagnosis of Invasive ductal carcinoma of the left breast grade 2. The history of disease: first identified a painless mass in the upper outer quadrant of the left breast 3-4 months ago. The patient did not go to the doctor. However, as she started to feel pain and it was gradually becoming severe in the lower inner quadrant of the left breast with reddening of the skin, the patient went to the clinic, where a physical examination in the upper outer quadrant revealed a dense immobile nodular formation up to 40.0 mm, the skin over which was not changed. In the lower inner quadrant, skin erythema was determined with swelling of the underlying tissues; from inframammary fold and down a straight line to the left hypochondrium. The subcutaneous tubular structure, painful to the touch, was determined visually. Raising the left arm above shoulder level contoured this tubular structure and aggravated the pain. The patient was referred to the ultrasound examination.
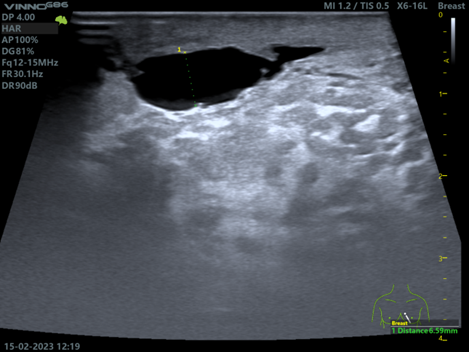
In the upper outer quadrant of the left breast, a hypoechoic solid formation was revealed (47.6x29.3x31.1 mm in size), with signs of spiculation, microlobulation, angulation of the margins and a zone of desmoplasia (Fig. 13). The cluster of destructive axillary lymph nodes are revealed on the left side (7.8x5.2 mm and up to 60.5x30.4 mm in diameter). Multiple petrifications in the stroma of the lymph nodes appeared (Fig. 14). In the lower-inner quadrant of the gland (at 7-9 o’clock) there was found superficial limited infiltration of the stroma, thickening of the skin up to 4.2 mm, fragmentary dilatation of the superficial vein. In this situation, differential diagnosis should be carried out with lymphangiectasia, which is also characteristic of malignant changes of the breast. The lymphangiectasia never has the sonographic appearance of Mondor’s disease, but is represented by small, short and winding tubular structures immediately under infiltrated, edematous, and thickened skin (Fig.16).
|
|
|
|
Figure 13. Hypoechoic mass with spiculation, microlobulation, angulation of margins; zone of desmoplasia are noted. |
Figure 14. A cluster of destructive axillary lymph nodes on the left with multiple petrification of the stroma |
|
|
|
|
Figure15. Limited stromal infiltration, skin thickening, fragmentary dilatation of the superficial vein, isoechoic thrombus in the lumen, no blood flow signals on power Doppler. |
Figure 16. The lymphangioectasia never have the sonographic appearance of Mondor’s disease, but are represented by small, short and winding tubular structures immediately under infiltrated, edematous, and thickened skin |
This case was defined as BI-RADS-5, and diagnosed as left breast cancer with metastasis in the left axillary lymph nodes; Mondor's disease of the soft tissues of the anterior chest on the left and lower quadrants of the left breast.
Conclusion
Thus, the clinical cases presented in the article demonstrate different clinical features of Mondor's disease with a single outcome. The disease is a spontaneously regressive disease within one, rarely more than one month. According to the literature, superficial vein thrombosis is more often localized in the upper outer quadrant, whereas in our series of studies, we found the lesion predominantly in the lower quadrants, bilateral lesions are extremely rare and probably may occur due to pregnancy. Correct interpretation of the data obtained and clear criteria for the sonographic pattern will help specialists to determine the disease in a timely manner and avoid errors associated with ductal ecstasies, and in combination with breast cancer - with lymphangiectasia.
Ethics: Informed consent was obtained from patients before all procedures and pictures of physical examination are published with patients permission
Peer-review: External and internal
Conflicts of interest: None to declare
Authorship: A.K., A.A., N.M., B.K., K.K., A.M.K., N.S.K. equally contributed to the study and manuscript preparation
Acknowledgement and funding: None to declare
References
- 1.Weerakkody Y. Mondor disease (breast) 2022: Available at: URL: https://radiopaedia.org/articles/mondor-disease-breast
- 2.Caruso M, Catalano o, Bard R, Corvino A, Corvino F, Cariazzo C, et al. Non-glandular findings on breast ultrasound. Part I: a pictorial review of superficial lesions. J Ultrasound 2022; 25: 783–97.
- 3 Alvarez‐Garrido H, Garrido‐Ríos AA, Sanz‐MuNoz C, Miranda‐Romero A. Mondor’s disease. Clin Exp Dermatol 2009; 34: 753–6. Doi: 10.1111/j.1365-2230.2009.03430
- 4. Amano M, Shimizu T. Mondor's disease: a review of the literature. Intern Med 2018; 57: 2607-12. doi: 10.2169/internalmedicine.0495-17
- 5.Shetty MK, Watson AB. Mondor's disease of the breast: sonographic and mammographic findings. AJR Am J Roentgenol 2001; 177: 893-6. doi: 10.2214/ajr.177.4.1770893
- 6.Ben Hamida K, Ghalleb M, Triki A, Jebir I, Makhlouf R, Touinsi H. Mondor’s disease of the breast: a case series. J Med Case Rep 2021: 15; 188.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER