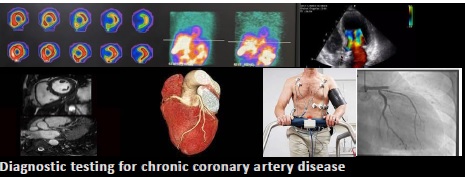
The changing paradigm of diagnostic testing for chronic coronary artery disease: An overview of the 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease
EDITORIALS
The changing paradigm of diagnostic testing for chronic coronary artery disease: An overview of the 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease
Article Summary
- DOI: 10.24969/hvt.2023.430
- Page(s): 262-263
- CARDIOVASCULAR DISEASES
- Published: 29/10/2023
- Received: 24/10/2023
- Accepted: 25/10/2023
- Views: 6557
- Downloads: 3931
- Keywords: editorial
Address for Correspondence: Andrea De Lorenzo, Instituto Nacional de Cardiologia, Rua das Laranjeiras 374, Rio de Janeiro, RJ, Brazil
E-mail: andlorenzo@hotmail.com Mobile: +55 21 30372288
Coronary artery disease is a major issue in daily medical practice. According to NHANES 2017-2020, total coronary heart disease (CHD) prevalence in United States adults ≥20 years of age is 7.1%, while the overall prevalence of angina pectoris is 3.9% (1). Despite an approximate 25% decline in death from CHD over the past decade, it remains the leading cause of death in the US and worldwide and is associated with large individual, economic, and societal burdens (2).
The 2023 American Heart Association (AHA)/American College of Cardiology (ACC) Multisociety Guideline for the Management of Patients with Chronic Coronary Disease (3) was released with the intent of providing an evidenced-based and patient-centered approach to management of patients with CHD, updating and consolidating new evidence since the publication of the 2012 Guideline for the Diagnosis and Management of Patients with Stable Ischemic Heart Disease and the 2014 Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease. The 2023 Guideline displays a change of terminology, from “stable ischemic heart disease” to “chronic coronary disease (CCD)”, with the latter encompassing obstructive and nonobstructive coronary artery disease with or without previous myocardial infarction or revascularization, ischemic heart disease diagnosed only by noninvasive testing, and chronic angina syndromes with varying underlying causes.
And what is new about diagnostic testing?
It is noteworthy that, among the 10 top take-home messages listed by the Guideline, #9 states that “routine periodic anatomic or ischemic testing without a change in clinical or functional status is not recommended for risk stratification or to guide therapeutic decision-making in patients with CCD.” (3) This represents a paradigm shift from the past, when routine diagnostic/prognostic testing was almost universal; also, it carries the strength of the endorsement of several medical societies.
The concept behind this statement is that, in patients with CCD, medical treatment should be initially optimized whenever possible, and testing deferred. According to the 2021 AHA/ACC Chest Pain Guideline, the optimization of anti-ischemic and preventive therapies is the mainstay to reduce patients´ angina burden and improve clinical outcomes. Indeed, the COURAGE, ISCHEMIA, and BARI-2D studies have shown that there is no reduction in major cardiovascular events with routine cardiovascular revascularization. (4-7)
Class 1 recommendations for testing are limited to patients with CCD and a change in symptoms or functional capacity that persists despite optimized medical treatment, in whom 1) stress single-photon emission computed tomography (SPECT) or positron emission tomography (PET) imaging, cardiac magnetic resonance imaging, or stress echocardiography are recommended to detect the presence and extent of myocardial ischemia, estimate the risk of major adverse cardiovascular events, and guide therapeutic decision-making (Level of evidence: B-non-randomized), or 2) invasive coronary angiography is recommended for guiding therapeutic decision-making with the goal of improving anginal symptoms (Level of evidence: B-randomized).
Regarding testing options, all available methods may be employed, keeping in mind the particular strengths and weaknesses of each method. The Guideline highlights, as Class 2a, that in patients selected for rest/stress nuclear imaging, PET may be preferred instead of SPECT, to improve diagnostic accuracy; that exercise treadmill testing can be useful to determine if symptoms are consistent with angina pectoris, and to evaluate functional capacity; that myocardial blood flow reserve determination can be useful to improve diagnostic accuracy and enhance risk stratification; and that computed tomography coronary angiography can be useful to evaluate bypass graft or stent (if ≥3mm) patency
In summary, the Guideline displays a more “conservative” approach towards diagnostic testing in CCD, which may be considered to be in line with the recent literature of observational studies and clinical trials in CCD, and which may, ultimately, be “salutary” when compared to a past of diagnostic testing overuse, with its accompanying risk of excessive radiation exposure and increased costs.
Andrea De Lorenzo
Instituto Nacional de Cardiologia,
Rio de Janeiro, RJ, Brazil
Peer-review: Internal
Conflict of interest: None to declare
Authorship: A.L.
Acknowledgment and funding: None to declare
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023; 147: e93–e621
- 2.WHO. Cardiovascular diseases. Available at: URL: https://www.who.int/health-topics/cardiovascular-diseases
- 3.Virani SS, Newby LK, Arnold SV, Bittner V, Brewer LC, Demeter SH, et al. 2023AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2023; 82: 833-955.
- 4.Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356: 1503–516.5.Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O`Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med 2020; 382: 1395–407.
- 6.Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, et al. BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009; 360: 2503–515.
- 7.Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021. AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022; 145: e18–e114.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

