Clinical manifestations and treatment outcomes of pulmonary aspergilloma
ORIGINAL RESEARCH ARTICLE
Clinical manifestations and treatment outcomes of pulmonary aspergilloma
Article Summary
- DOI: 10.24969/hvt.2023.432
- CARDIOVASCULAR DISEASES
- Published: 03/11/2023
- Received: 19/08/2023
- Revised: 23/09/2023
- Accepted: 14/10/2023
- Views: 6269
- Downloads: 3760
- Keywords: aspergilloma, clinical manifestations, treatment, surgery procedures, outcome
Address for Correspondence: Amulya Cherukumudi, Department of Cardiothoracic Surgery, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Email: amicool91@gmail
Authors
Department of Cardiothoracic Surgery, Rangaraya Medical College, Kakinada, Andhra Pradesh, India
Department of Cardiothoracic and Vascular surgery Sri Jayadeva Institute of Cardiovascular Sciences and Research Bangalore, Karnataka, India
Popuri Madan, Kiran Ganta, Amulya Cherukumudi
Department of Cardiothoracic Surgery, Rangaraya Medical College, Kakinada, Andhra Pradesh, India
Abstract
Objective: In developing countries like India where tuberculosis is highly prevalent, the incidence of pulmonary aspergilloma is also high. Mortality and morbidity associated with surgical treatment of aspergilloma in previous studies has discouraged surgeons from taking up surgery as the preferred treatment. This study focuses on the clinical outcome of patients with pulmonary aspergilloma and its surgical management.
Methods: Fifty-one patients who underwent thoracotomy for pulmonary aspergilloma from 2015 to 2017 were studied retrospectively by reviewing their medical records.
Results: The most common clinical presentation of pulmonary aspergilloma was hemoptysis, which occurred in 76.0% of patients. Tuberculosis was the most common pre-existing disease (72%). High resolution computed tomography of chest, showed the typical "air-crescent" sign in all patients. Systemic antifungal therapy neither palliated the clinical symptoms nor eradicated the aspergilloma, and transarterial embolisation was also unsuccessful. Surgery offered the only chance of cure for both unilateral and bilateral disease. Procedures varied from segmentectomy to pneumonectomy with most (75%) undergoing lobectomy. There was no death following surgery and postoperative complications occurred in 5 patients. Postoperatively, most of the patients were symptom-free.
Conclusion: Symptomatic pulmonary aspergilloma patients are best treated by early surgical intervention with good results in experienced centers.
Key words: aspergilloma, clinical manifestations, treatment, surgery procedures, outcome
Introduction
Aspergillus is a genus of saprophytic fungi that is ubiquitous in nature, and therefore, makes their way to the airways with ease through inhalation. Pulmonary aspergilloma (PA) generally forms from saprophytic colonization of pre-existing pulmonary cavities producing a fungus ball or a mycetoma (1, 2). Healed tuberculous lesions, benign lung abscess, and cavitary bronchiectasis are fertile grounds for Aspergillus to develop. It is often observed that following the development of the intra-cavitatory fungal colony, medications are ineffective, as they cannot access the fungal agent. The most common species involved in such a process in Aspergillus fumigatum (3). The annual incidence of invasive aspergillosis in India is an estimated 250,900 cases, including 79,100 to 239,000 cases in people with chronic obstructive pulmonary disease. However, globally, A re-estimation of the prevalence of PA was found to be around 1.5 million. Over 42,000 deaths occur within 12 months of misdiagnosis of pulmonary tuberculosis (3).
Surgical resection offers the only realistic chance of a permanent cure for aspergilloma (4–6). The goals of the surgery are prevention of hemoptysis with preservation of lung parenchyma. Although successful lobectomy for PA was described in 1948 (7), surgical indication is still controversial. Belcher and Pulmmer (8) classified aspergilloma into simple and complex types; complex aspergilloma had been reported with high mortality and morbidity (9). Some authors have advocated the prophylactic resection of all PAs because of the risk of massive hemoptysis (10-12). Other authors recommend surgical treatment only after hemoptysis has occurred (13, 14). A proportion of the patient population will have advanced chronic lung disease to a degree that eliminates the surgical option. Some authors consider that surgical resection should be avoided because of the high incidence of postoperative complications (15).
This study focuses on the clinical outcome of patients with pulmonary aspergilloma. Our primary objectives were to assess the risk of surgical treatment and to evaluate outcomes of the surgical resection in the treatment of pulmonary aspergilloma.
Methods
This was a retrospective observational study conducted over a 3-year period, 2020 to 2023, in the department of thoracic surgery in a tertiary care center. All patients who underwent surgery for pulmonary aspergilloma in last 3 years, aged between 15-65 years were identified. The patient’s records were retrieved, and 51 consecutive cases were studied with reference to clinical profile, radiological findings, and indications for surgery, surgical procedures used and short- and long-term post-operative outcomes. There were 41 male and 10 female patients in the age group of 15 to 65 years (mean 38.6 years).
Overall, 59 definitive surgical procedures were carried out, including eight re-operations for post-operative complications and for recurrent disease.
The diagnosis of PA was confirmed by mycological smears and cultures. All the patients were initiated on antifungal drugs based on culture and sensitivity: itraconazole- 100-mg capsules (loading dose: 200 mg orally 3 times a day for the first 3 days of therapy, maintenance dose: 200 mg orally once or twice a day), 65-mg capsules (loading dose: 130 mg orally 3 times a day for the first 3 days of therapy, maintenance dose: 130 mg orally once or twice a day). Duration of therapy was at least 3 months and until clinical parameters and laboratory tests indicate the active fungal infection has subsided. Amphotericin B, indicated for treatment of Aspergillus species, Candida species, and/or Cryptococcus species infections was used in a dose of 3-5 mg/kg IV per day.
All the patients planned for surgery for pulmonary aspergillosis underwent laboratory tests: complete hemogram, blood urea, serum creatinine; chest X‑ray (posteroanterior view) and computed tomography (CT) scan of thorax, bronchoscopy, pulmonary function test subjected to a frequency of hemoptysis.
Operative steps
An epidural catheter was secured in all cases before administrating anesthesia. All the cases were operated under general anesthesia, with double-lumen endotracheal tubes in situ for adequate isolation and selective ventilation, through standard posterolateral thoracotomy. The thorax was entered through the fifth or sixth intercostal space depending on the location of the aspergilloma as depicted in the CT scan. In ten cases, we had to resect portions of 3rd and 4th ribs when densely adherent to the lesions. Adhesiolysis was done to set the lungs free. Meticulous hemostasis was done from the very beginning of the operation. The affected segment of the lung was identified.
The interlobar fissure was dissected, branches of the pulmonary artery and vein supplying the lobe were ligated and transfixed. In four cases, we had to resort to intrapericardial ligation of pulmonary vessels, as the extra pericardial hilum was unapproachable. The lobar bronchus was divided, and the specimen was removed and sent for histopathological study. The bronchial stump was closed with 3–0 Prolene interrupted stitches. Care must be taken to prevent endotracheal contamination by using suctioning. After closure, the anesthetist was asked to inflate the lungs. The bronchial stump and the lungs thoroughly checked for any air leak. Hemostasis thoroughly secured with special attention to the adhesiolysis sites on the chest wall. Two chest drains were inserted. Chest closed with 2.0 Vicryl sutures. Most of the patients were extubated in the operating room and sent to the Intensive care Unit. Some patients required ventilator support.
Postoperative care
On the day of the surgery, the patients were administered intravenous fluid for 6 h postoperatively, following which they were allowed oral diet. Adequate postoperative pain management is done by epidural administration of Sensorcaine, intravenous administration of paracetamol, intramuscular nonspecific anti-inflammatory drugs, and transdermal fentanyl path application. This aggressive pain management helps in the early mobilization of patients. The patients were encouraged to do breathing exercises with an incentive spirometer as early as 0 postoperative day. Postoperative chest X‑ray was done daily until the chest drains were removed. Bronchoscopy was done in patients showing collapsed lung and unable to perform adequate respiratory physiotherapy to rule out endobronchial obstruction. Chest drains were usually removed by 48 h after the lungs are satisfactorily inflated. Intravenous antibiotics continued for 3 days. Intravenous antifungals are given on postoperative day 0 following which they are continued in tablet form for a period of 3 weeks.
Statistical analysis
All data from case records: presenting complaints, diagnosis, surgeries performed, laboratory and functional tests, and follow up records were collected and analyzed in excel spreadsheet. Continuous data are presented as mean and standard deviation, categorical data as percentages.
Results
The patient sample (Table 1) included 41 men and 10 women with a median age of 35 years, range 15 to 65 years; mean 38.6 (11.82) years. Eight patients had no underlying lung disease and were classified into the simple aspergilloma group (SA) and 43 patients were classified into the complex aspergilloma group (CA).
The underlying lung diseases of the CA group were tuberculosis (30, 59%), bronchiectasis (2, 4%), and 1 case of immunocompromized-steroid abuse (1%), 7 patients had multiple etiologies (all patients with multiple etiologies had tuberculosis associated with other disease conditions like superadded bacterial infection, bronchiectasis, etc.) (13%), and 5 patients had recurrence of symptoms post-surgery (9%).
|
Table 1. Demographic and clinical characteristics |
||
|
Variables |
Number or Mean (SD) |
|
|
Sex, n |
Male |
41 |
|
Female |
10 |
|
|
Age, years |
38.6 (11.82) |
|
|
Body mass index, kg/m2 |
18.7 (3.1) |
|
|
Type, n |
Single |
8 |
|
Chronic cavitary pulmonary aspergilloma |
43 |
|
|
Etiology, n |
Tuberculosis |
30 |
|
Bronchiectasis |
2 |
|
|
Steroid abuse |
1 |
|
|
Multiple causes |
7 |
|
|
Recurrence |
5 |
|
The main signs and symptoms were hemoptysis in 39 (76%), cough or sputum in 38 (74%), fever in 4 (7.8%), chest pain in 1 (1.96%), and weight loss in 5 patients (9.8%) , shortness of breath in 2 patients (3.92%) (Fig. 1).
The lesions were in the right or left upper lobes in a majority of patients. In 7 patients, lesions were found in more than one lobe (Fig. 2).
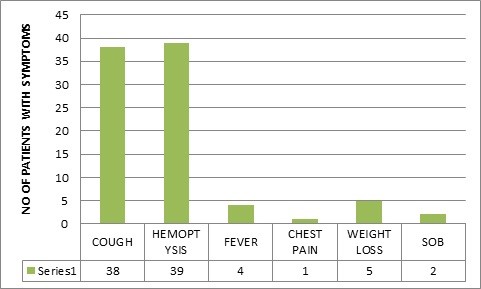
Figure 1. Presenting symptoms of patients with PA
PA - pulmonary aspergilloma, SOB – shortness of breath
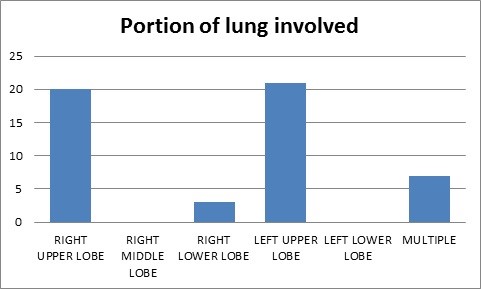
Figure 2. Location of the lesions patients with pulmonary aspergilloma
Surgical management of PA
Lobectomy was the most common procedure performed. Other procedures included segmentectomy, pneumonectomies, and cavernostomies. Cavernostomy was performed in 2 patients with complex aspergilloma with dense adhesions and heavy bleeding with poor respiratory reserve at the time of operation. These patients subsequently underwent lobectomy. Wedge resection was done in 2 patients who had peripheral fungal balls.
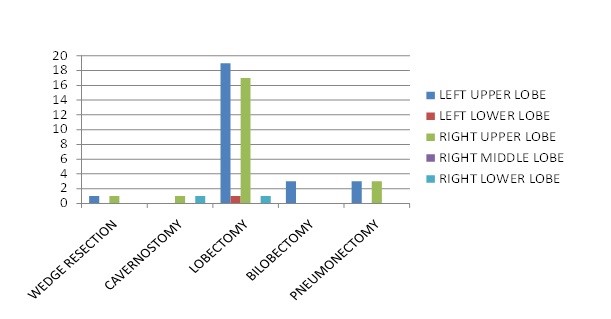
Figure 3. Type of surgeries
|
Table 3. Type of surgeries and perioperative variables and outcomes |
||
|
Characteristics |
Type |
Number or Mean (SD) |
|
Surgical procedure |
Lobectomy |
33 |
|
Wedge resection |
2 |
|
|
Cavernostomy |
2 |
|
|
Bilobectomy |
3 |
|
|
Pneumonectomy |
4 |
|
|
Re-do |
7 |
|
|
Duration of hospital stay, days |
12.23 (3.59) |
|
|
Duration of surgery, minutes |
72.42 (18.11) |
|
|
Duration of ICU stay, days |
2.57 (0.86) |
|
|
ICS-reinsertion, n |
11 |
|
|
Death, n |
0 |
|
|
ICU –intensive care unit, ICS –inhaled corticosteroids |
||
We had one case of intraoperative pulmonary vein bleeding which needed cardiopulmonary bypass support for repair, 4 patients developed bronchopleural fistulas requiring pectoralis muscle flap cover. We had 7 cases with residual cavitation and persisting symptoms requiring redo surgeries. Of these, 1 case was of post-operative wedge resection, one was pneumonectomy and 5 other cases were non-anatomical lobectomies. There was no mortality in our study. Postoperative complications were negligible: one patient had incomplete re-expansion, which resolved spontaneously, and one patient developed a wound infection needing long time wound care management.
Discussion
While the surrounding lung is normal, simple aspergilloma grows in isolated thin-walled cysts with ciliated epithelium lining them. Complex aspergilloma grows in cavities created by gross lung tissue diseases like severe sarcoidosis, bronchiectasis, chronic lung abscess, or tuberculosis. Patients who have CA typically have more severe symptoms and have more surgical problems. Our data showed that 84% of the patients had an underlying lung condition, classifying them as having the complex form. In 16% of the patients, the underlying lung parenchymal illness was not found. In our series, tuberculosis was the most prevalent underlying pulmonary condition. Despite some degree of sickness, there were many people whose lung conditions were not severe. Patients with any indication of a thick cavity or underlying lung illness were categorized as having the complex variant (6).
Hemoptysis has been identified as the aspergilloma symptom that occurs most frequently (6). In our patients, hemoptysis or blood-tinged sputum affected almost 76% of them. Fever, shortness of breath, malaise, weight loss, chest pain, and reactive airway disease are less typical symptoms; comparable findings were found in our data.
In our analysis, the most prevalent illness locations were in the superior segment of the lower lobe and the apical region of the upper lobe, which may be related to pulmonary tuberculosis. It has been demonstrated that a sizable proportion of CA patients also have immunosuppression. Only one patient in our series, nevertheless, displayed signs of immunosuppression. This aspect could be another explanation for our comparatively positive outcome.
Patients with chronic cavitary PA without clinical symptoms can be studied without antifungal medication and followed every 3–6 months, but will need at least 6 months of treatment when the disease develops (16). Chronic cavitary PA patients with severe hemoptysis or failed therapy may undergo surgery, which has greater postoperative complication rates (17). Shen et al. (5) found that 24 chronic cavitary PA patients (68.6%) had recurrent or recurring hemoptysis and needed surgery, 5 of whom had life-threatening hemoptysis and had bronchial artery embolization. After surgery, 5.7% had complications and 8.6% had recurrence. Chronic cavitary PA has similar postoperative complications and recurrence rates to single aspergilloma, contrary to other reports (13, 15, 18).
Chronic fibrous PA is the final fibrosing progression of chronic cavitary PA, and its best treatment is unknown. Continuous antifungal medication frequently delays disease progression or relieves symptoms. There are limited reports on chronic fibrous PA surgery (19-21), possibly due to the high postoperative complication rate and death. Five (38.5%) of 13 patients who underwent surgery had postoperative problems, and one relapsed.
Computed tomography to identify the Aspergillus nodules, which look like cancer, is a vital investigative tool (8), which can be further confirmed by histopathology. In our study, 11 patients had aspergillus nodules on thorax CT, of which 2 patients were asymptomatic, 3 had cough and sputum, and 7 had hemoptysis. It is unclear if asymptomatic patients need surgery or other treatment. Lung cancer suspicion led to surgery for two patients, who underwent pneumonectomy. Our department recommends serial low-dose chest CT scans for asymptomatic patients.
The first choice is open thoracic surgery, but vieo-assisted thoracic surgery (VATS) are becoming more common. However, owing to the cost incurred to the patient, open thoracotomy is preferred in our institution.
Some studies have suggested bronchial artery embolization. In high-risk patients, we advise bronchial artery embolisation; in the event that it is unsuccessful, we consider alternative treatments including cavernostomy with muscle flap transposition. As a result, our series would not be representative of the entire CA population.
In a research comparing medical and resection therapy, Jewkes and colleagues (11) discovered that in a patient group with minimal or no hemoptysis, the medical (65%) and resectional (75%) choices had comparable 5-year survival rates. However, the 5-year survival rate for individuals with recurrent hemoptysis or a single significant hemorrhage was 41% for medical treatment and 84% for resectional therapy, indicating the need for resectional therapy for this group of patients.
Preoperative assessment (cardiac and pulmonary reserve are computed), adequate infrastructure availability, qualified nursing personnel, an experienced anesthesiologist and surgeon, followed by intense postoperative physiotherapy, all contributed to our surgical success of 100% overall survival.
The extensive fibrosis surrounding the cavity, the destruction of the pleural space and fissures, the swollen and convoluted bronchial arteries, and the sick pulmonary parenchyma surrounding the lesion make CA operations frequently technically difficult. The residual lung may not be able to fully expand to fill the pleural space following excision due to inflammatory fibrosis of the pulmonary parenchyma and pleura.
Our outcomes in CA are significantly better, with 0% mortality and 12% morbidity (2 patients developed bronchopleural fistulas, 4 patients had persistent symptoms). The variations in the underlying pulmonary illness and its severity, as well as a stricter patient selection, may be one explanation for the improved results (12-14).
The underlying pulmonary illness plays a significant role in the outcome since chronic respiratory failure or pneumonia account for the majority of fatalities (6, 9). The survival rates of patients with SA appear to be equivalent to those of the general population (10, 12). A prospective study in Gulu, Uganda over 2 years, in both HIV-positive and HIV-negative survivors of PTB, found the annual rate of development of PA to be 6.5% in those with residual cavitation and 0.2% in those without (a mean of 4.9-6.3%) 2–7 years after antitubercular treatment (15). There was a non-significant difference between HIV-positive and HIV-negative patients, with a higher loss to follow up in the former. There are very few data on occurrence and survival beyond 5 years, which is why our study did not attempt to extend the estimate beyond this time. As a result, our prevalence and mortality estimates are likely to be slightly lower than the true values.
Conclusion
In conclusion, surgical treatment for both SA and CA in a chosen patient population could function to produce favorable long-term outcomes even though postoperative morbidity was higher in CA. Surgical resection is the only effective treatment for aspergilloma. Hemoptysis is the commonest presentation of aspergilloma.
Ethics: All patients provided informed consent for all procedures and treatment.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: K.G. and P.M. equally contributed to the study, preparation of manuscript and fulfilled authorship criteria
Acknowledgment and funding: None to declare
References
- 1.Denning, DW, Cole DC, Ray A. New estimation of the prevalence of chronic pulmonary aspergillosis (CPA) related to pulmonary TB - a revised burden for India. IJID 2022; 6: 7–14. Doi: 0.1016/j.ijregi.2022.11.005
- 2.Fréalle E, Reboux G, Le Rouzic O, Bautin N, Willemin M-C, Pichavant M, et al. Impact of domestic mould exposure on Aspergillus biomarkers and lung function in patients with chronic obstructive pulmonary disease. Environ Res 2021; 195. doi: 10.1016/j.envres.2021.110850
- 3.Glaziou P, Floyd K, Raviglione MC. Global epidemiology of tuberculosis. Semin Respir Crit Care Med. 2018; 39: 271–85. doi: 10.1055/s-0038-1651492.
- 4.Guitard J, Sendid B, Thorez S, Gits M, Hennequin C. Evaluation of a recombinant antigen-based enzyme immunoassay for the diagnosis of noninvasive aspergillosis. J Clin Microbiol 2012; 50: 762–5. doi: 10.1128/JCM.01257-11.
- 5.Shen C, Qiao G, Wang C. Outcomes of surgery for different types of chronic pulmonary aspergillosis: results from a single-center, retrospective cohort study. BMC Pulm Med 2022; 22: 40. Doi: 10.1186/s12890-022-01836-z
- 6.Zheng S, Li X, Hu B, Li H. Is adjuvant antifungal therapy after video-assisted thoracic surgery for pulmonary aspergilloma necessary? J Thorac Dis 2018; 10: 6060–5.
- 7.Jhun BW, Moon SM, Jeon K, Kwon OJ, Yoo H, Carriere KC, et al. Prognostic factors associated with long-term mortality in 1445 patients with nontuberculous mycobacterial pulmonary disease: a 15-year follow-up study. Eur Respir J 2020; 55. doi: 10.1183/13993003.00798-2019
- 8.Kim C, Moon J-W, Park Y-B, Ko Y. Serological changes in anti-Aspergillus IgG antibody and development of chronic pulmonary aspergillosis in patients treated for pulmonary tuberculosis. J Fungi 2022; 8: 130. doi: 10.3390/jof8020130.
- 9.Koyama K, Ohshima N, Suzuki J, Kawashima M, Okuda K, Sato R, et al. Evaluation of clinical characteristics and prognosis of chronic pulmonary aspergillosis depending on the underlying lung diseases: Emphysema vs prior tuberculosis. J Infect Chemother 2015; 21: 795–801. doi: 10.1016/j.jiac.2015.08.006
- 10.Kwizera R, Katende A, Bongomin F, Nakiyingi L, Kirenga BJ. Misdiagnosis of chronic pulmonary aspergillosis as pulmonary tuberculosis at a tertiary care center in Uganda: a case series. J Med Case Reports 2021; 15: 140. doi: 10.1186/s13256-021-02721-9
- 11.Kwizera R, Parkes-Ratanshi R, Page ID, Sekaggya-Wiltshire C, Musaazi J, Fehr J, et al. Elevated Aspergillus-specific antibody levels among HIV infected Ugandans with pulmonary tuberculosis. BMC Pulm Med 2017; 17: 149. doi: 10.1186/s12890-017-0500-9
- 12.Lowes D, Al-Shair K, Newton PJ, Morris J, Harris C, Rautemaa-Richardson R, et al. Predictors of mortality in chronic pulmonary aspergillosis. Eur Respir J 2017; 49. doi: 10.1183/13993003.01062-2016.
- 13.Maitre T, Cottenet J, Godet C, Roussot A, Abdoul Carime N, Ok V, et al. Chronic pulmonary aspergillosis: prevalence, favouring pulmonary diseases and prognosis. Eur Respir J 2021; 58. doi: 10.1183/13993003.03345-2020
- 14.Matsuda J, Wanke B, Balieiro AA, da S, Santos CS, Cavalcante RCDS, Muniz M, et al. Prevalence of pulmonary mycoses in smear-negative patients with suspected tuberculosis in the Brazilian Amazon. Rev Iberoam Micol 2021; 38: 111–8. doi: 10.1016/j.riam.2020.12.004
- 15.Page I, Byanyima R, Hosmane S, Onyachi N, Opira C, Richa M, et al. Chronic pulmonary aspergillosis commonly complicates treated pulmonary tuberculosis with residual cavitation. Eur Respir J 2019; 53. doi: 10.1183/13993003.01184-2018
- 16. Karas A, Hankins JR, Attar S, Miller JE, McLaughlin JS. Pulmonary aspergillosis: An analysis of 41 patients. Ann Thorac Surg 1976; 22: 1-7.
- 17. Kliman JW, Ahn C, Andrews NC, Klassen K. Surgery for pulmonary aspergillosis, J Thorac Cardiovasc Surg 1969: 57: 642-7.
- 18.Saab SB, Almind C. Surgical aspects of pulmonary aspergillosis. J Thorac Cardiovasc Surg 1974; 68: 455-60.
- 19. Mohapatra B, Sivakumar P, Bhattacharya S, Dutta S, Surgical treatment of pulmonary aspergillosis. A single-center experience. Lung India 2016; 33: 9-13.
- 20. Pratap H, Dewan RK, Singh L, Gill S, Vaddadi S, Surgical treatment of pulmonary aspergilloma; a series of 72 cases. Indian J Chest Dis Allied Sci 2007; 49: 23-7.
- 21. Babatasi G, Massetti M, Chapeliar A, Fadel E, Macciarani P, Khayat A, et al. Surgical tretamen tof pulmonary aspergilloma: current outcome. J Thorac Cardiovasc Surg 2000; 119: 906-12.
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

