Design and implementation of cardiac rehabilitation in pediatric heart re-transplantation: a case report
CASE REPORT
Design and implementation of cardiac rehabilitation in pediatric heart re-transplantation: a case report
Article Summary
- DOI: 10.24969/hvt.2023.438
- Transplantation
- Published: 30/11/2023
- Received: 06/10/2023
- Revised: 26/11/2023
- Accepted: 27/11/2023
- Views: 4958
- Downloads: 3541
- Keywords: cardiac rehabilitation, heart transplantation, physical therapy, rehabilitation, extracorporeal membrane oxygenation
Address for Correspondence: Roberta da Silva Teixeira, Rua das Laranjeiras, 374, Rio de Janeiro, RJ, Brazil,
Email: robertateixeira@outlook.com
Roberta da Silva Teixeira1,2, Fellipe Allevato Martins da Silva1,2
1Physiotherapy Service, National Institute of Cardiology, Rio de Janeiro, RJ, Brazil
2Postgraduate Program in Physiotherapy in Cardiopediatric and Neonatal Intensive Care, National Institute of Cardiology, Rio de Janeiro, RJ, Brazil
Abstract
Objective: There are no guidelines for cardiac rehabilitation in pediatric cardiac re-transplantation. The study describes the design and implementation of the exercise prescription in a cardiac rehabilitation program, which evaluated the indicators of respiratory muscle force, vital capacity, functional capacity, pulmonary function efficacy, manual muscle force, mobility, and generic health status in a 14-year-old male patient who underwent a heart re-transplant requiring extracorporeal membrane oxygenation.
Case presentation: A 14-year old boy with redo heart transplantation was referred for rehabilitation. A heart transplant patient had an unfavorable evolution after pericardiectomy. He underwent re-transplantation and had extracorporeal membrane oxygenation dependence due to significant ventricular dysfunction. Diffuse alveolar hemorrhage and lower airways infectious/inflammatory process occurred during the days of mechanical ventilation. The physiotherapy team conducted the exercise prescription in a cardiac rehabilitation program and intervened during the hospital stay. The program included aerobic and resistance training, respiratory muscle strengthening and inspiratory capacity work, impairment-based interventions, non-invasive ventilatory support, and postural interventions. Quantitative assessments were applied weekly.
Conclusion: Cardiac rehabilitation of the pediatric re-transplant patient was well succeeded.
Graphical abstract

Key words: cardiac rehabilitation, heart transplantation, physical therapy, rehabilitation, extracorporeal membrane oxygenation
Introduction
Heart re-transplantation is probability in all age groups (1), especially in pediatrics; the patients are young at the time of transplantation in this population, and the life expectancy of a transplanted heart to be short (concerning the child's age) (2). Re-transplanted patients may have higher mortality (3). The complexity of this patient category may require a long period of hospitalization, which is highly related to worsening prognosis (4).
Evidence shows the benefits of exercise intervention in receivers of a new heart (5). Cardiac rehabilitation is crucial for hospital recovery. Major health associations recommend cardiac rehabilitation in heart transplantation. In pediatric transplantation, exercise is encouraged without specifying a cardiac rehabilitation program (6).
The present paper describes the design and implementation of exercise prescription in a cardiac rehabilitation program, which evaluated the indicators of respiratory muscle force, vital capacity, functional capacity, pulmonary function efficacy, manual muscle force, mobility, and generic health status in a 14-year-old male patient who underwent a heart re-transplant requiring extracorporeal membrane oxygenation (ECMO).
Case report
A pediatric 14-year-old male patient with a body mass index of 24 kg/m2 and a history of dilated cardiomyopathy with subsequent heart transplantation was admitted to our hospital.
Two years after heart transplantation, surgeons performed a pericardiectomy due to constrictive pericarditis. The postoperative surgical evolution was unfavorable as a consequence of a cardiac arrest in the pediatric intensive care unit (PICU).
After two hours of reanimation protocol, it was necessary to proceed with veno-arterial ECMO implementation.
The new transplantation occurred six days after ECMO implementation. The patient presented with severe ventricular dysfunction after re-transplantation surgery and remained on ECMO for another seven days. At that moment of better hemodynamic and echocardiogram parameters, the surgical team removed extracorporeal support and performed chest closure.
Diffuse alveolar hemorrhage and lower airway infectious/inflammatory process occurred during the 24 days of mechanical ventilation (18 days of intubation after transplant). The extubation succeeded for non-invasive positive pressure ventilation (NIPPV), bilevel modality via full-face mask. Tachypnea, pleural effusion, hypoxemia, cellulite, and a sacral ulcer (grade II) were manifestations detected at the beginning of cardiac rehabilitation. The Ethics and Research Committee approved this case report. The child's father provided informed consent, and the child assented.
The physiotherapy team conducted the exercise prescription in cardiac rehabilitation, as well as intervened during the entire hospital stay. The decision to proceed with rehabilitation was taken based on the absence of signs of intolerance, such as increased respiratory effort, psychomotor agitation/cognitive alteration, oxygen saturation less < 92%, cardiac arrhythmia, heart rate and blood pressure > 20% of baseline, and increase in pain score.
The physiotherapy team divided the cardiac rehabilitation program into two stages (PICU and ward). The detailed program can be found in Figure 1. Physical therapists (PTs) were trained and approved for standardized conduction of cardiac rehabilitation. A team of healthcare professionals acted simultaneously offering the care inherent in their area to the patient.
Concerning the patient's weakness, the PTs applied the initial daily activities in three periods in the PICU (3 sessions of 1 hour each). The morning routine consisted of stretching and muscle strengthening, postural interventions, incentive spirometer, and inspiratory muscle training, followed by ventilatory support at rest. In the afternoon, the team performed aerobic training, postural interventions, and ventilatory support. At night, incentive spirometer, postural interventions, and ventilatory support were applied.
After three weeks of rehabilitation, the second phase of this intervention began in the ward. PTs continued the program applied in the PICU on one-hour daily sessions, except for ventilatory support. The patient and his parents were instructed about active mobility maintenance, regular incentive spirometer use, and motor exercises.
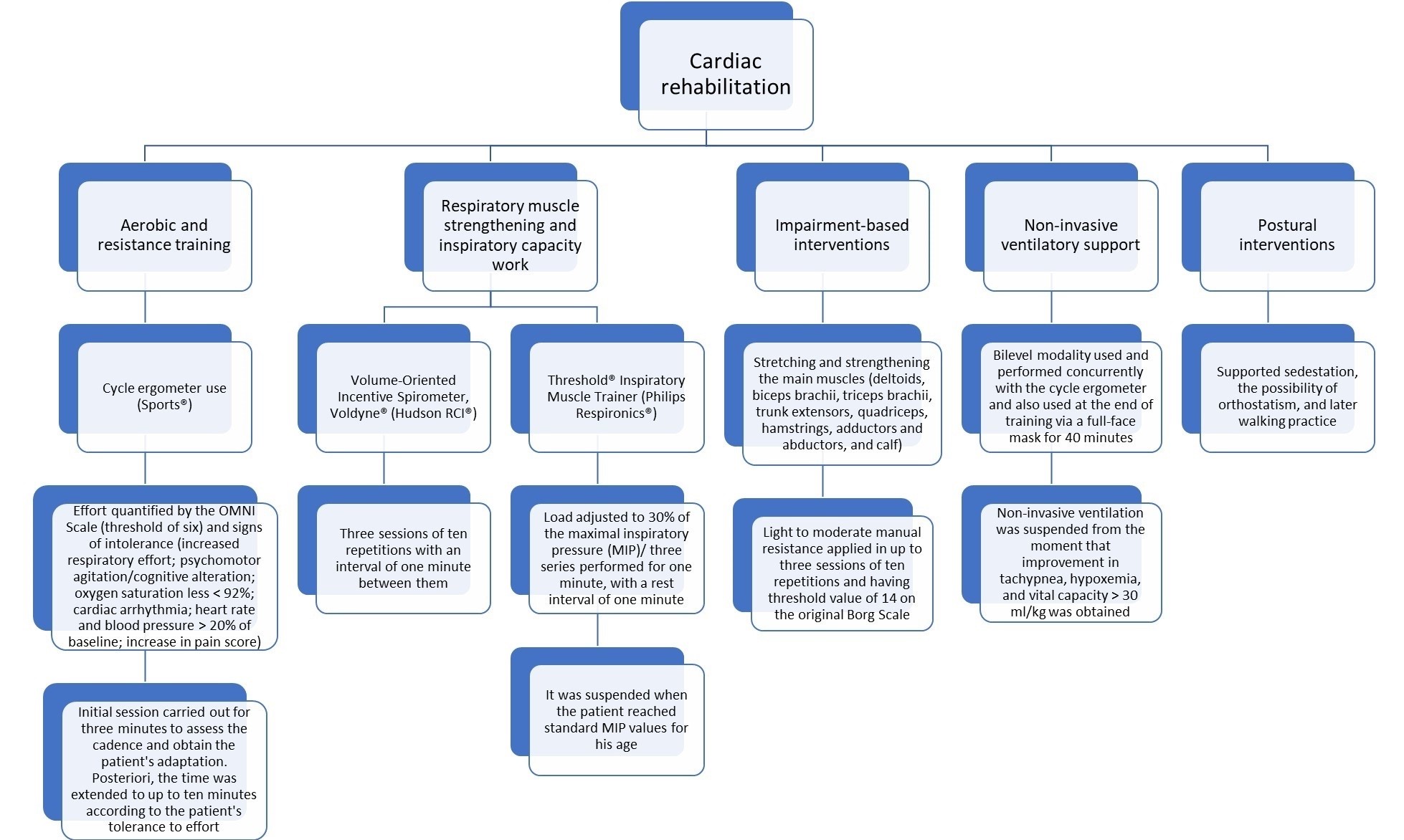
Figure 1. Cardiac rehabilitation program
PT applied quantitative assessments throughout the treatment weekly. PT assessed respiratory muscle force, vital capacity, functional capacity, pulmonary function efficacy, manual muscle force, mobility, and generic health status. The context of the cardiac rehabilitation approach defined these outcome measures. The difficulty in providing a cardiac rehabilitation program for this patient is the absence of specific reference indexes for the pediatric heart transplant population. Due to this limitation, the team considered values based on healthy individuals, and, attaining the adopted reference values, the tests were suspended.
Generic health status
EuroQol 5-Dimension questionnaire (EQ-5D) was applied to obtain health status and to construct the metric QALYs (Quality Adjusted Life Years), a health outcome that weighs the quantity and quality of life in a single value. The mobility, self-care, habitual activities, pain/discomfort, and anxiety/depression were items evaluated using a three-level scale.
Respiratory muscle force
The monovacuometer (Wika®) estimated the maximum inspiratory pressure and expiratory pressure (MEP). PT provided a detailed explanation of the tests and vigorously stimulated the patient in the executions. The measurements were repeated three times within one-minute with the highest recorded value (7). The maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) reference indices were -124 (42) cmH2O and 169 (57) cmH2O, respectively (7).
Vital capacity
The measurement was performed by the ventilometer device (Nspire TM®) in the sitting position, with the calculation of the vital capacity (ml) by the weight predicted in kilograms (Kg). The procedure followed the guidelines. Reference values were divided into three grades: normal (> 60 ml/Kg), noninvasive ventilation indication (<30 ml/Kg), and orotracheal intubation indication (<15 ml/kg) (8).
Functional capacity
It was assessed by the six-minute walk test (6MWT), performed by the American Thoracic Society guidelines. Heart rate, blood pressure, oxygen saturation, and the original Borg effort perception scale were measured before and immediately after the walk test ended. Total distance and any rest were recorded. For a predicted value of 719.05 meters, we use the equation proposed by Geiger et al. (9).
Pulmonary function efficacy
Through the peak flow tool (Philips Respironics®), the airflow or expiratory flow rate was estimated in three interval attempts with the patient seated and previously oriented and encouraged in the test. A better valuation was considered. A reference of 516 liters per minute was considered standard (10).
Manual muscle force
Using the manual muscle force score established by the Medical Research Council (MRC), the measurement was performed via isometric contraction or resistive movement or not for a set of 12 muscle groups (shoulder abductors, elbow flexors, wrist extensors, hip flexors, knee extensors, and dorsiflexors, assessed bilaterally). The patient remained in the supine position during the procedure.
Mobility
The capacity description to perform various activities with different levels of physical capacity was made using the Functional Status Score-Intensive Care Unit (FSS-ICU) mobility scale. This scale comprises five functional tasks: rolling; transfer from supine to sitting; transfer from sitting to standing; sitting at the bedside; and walking.
Outcomes
The same PT, who has extensive experience in conducting the adopted tests, evaluated the values. The outcomes are organized by functions: respiratory, motor, endurance, and general health status.
Respiratory function
Cardiac rehabilitation obtained significant gains in aspects evaluated. Respiratory muscle force and vital capacity increased successively (Fig. 2). Inspiratory and expiratory muscles were compromised. The MEP had the most deficit. The increase in vital capacity with rehabilitation was 3.8 times. The initial quantification was very close to the tracheal intubation indication, which determined the NIPPV (noninvasive positive pressure ventilation) used for a prolonged period (two weeks). At the rehabilitation end, the patient fully recovered his capacity.
In lung function efficacy, three measurements were necessary to reach the standard value. The expiratory flow rate progression is undeniable. The first measurement corresponded to 71% of the ideal (370 l/min). The subsequent measures were 320 l/min and 550 l/min.
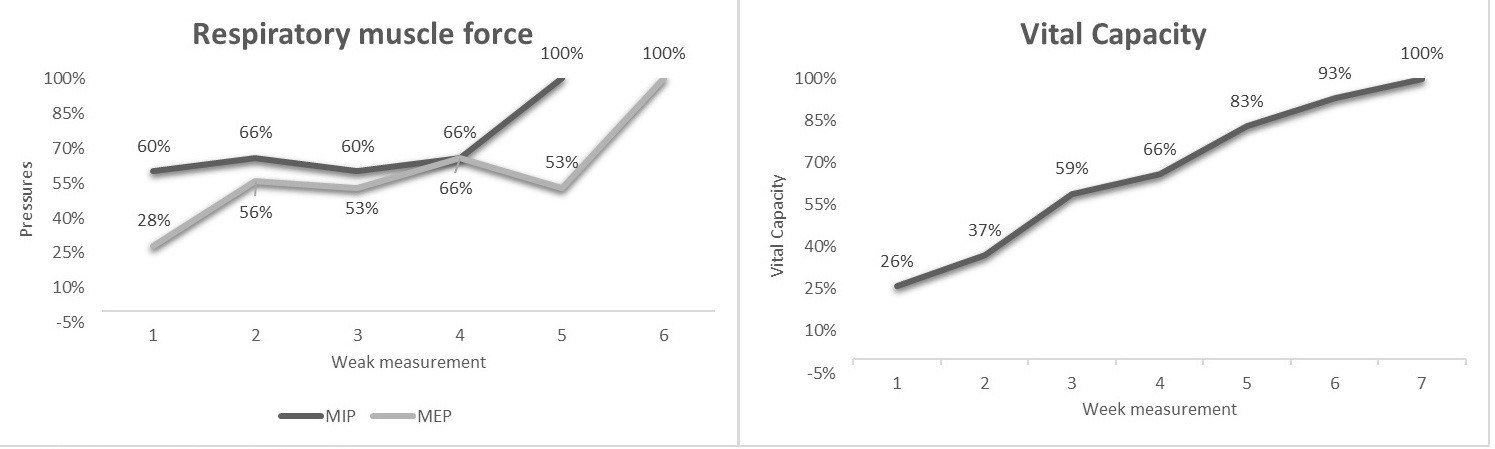
Figure 2. Respiratory muscle force and vital capacity assessment
MEP – maximal expiratory pressure, MIP – maximal inspiratory pressure
Endurance function
The functional capacity measurements (Fig. 3) only started when the patient walked without any support, which occurred four weeks after the start of cardiac rehabilitation. The 6MWT quantification totaled four measures, with significant gains, mainly in the three initial estimates. The patient did not reach the standard distance during the hospital admission.
Motor function
By assessing the mobility and muscle force scales (Fig. 4), it is possible to observe the accentuated degree of patient fragility. Manual muscle force and mobility represented 14% and 56% of their maximum scores, respectively. In the second week of rehabilitation, mobility increased by 4 times. The manual muscle force increased by 1.7 times in the third measure.
Generic health status function
We obtained utility at the beginning and end of hospital cardiac rehabilitation to measure the generic health status. The item related to mental state did not change with the patient reporting remaining moderately anxious or depressed. The variation of utility was broad, with the first sequence related to negative utility (-0.0275) and the last positive (0.408). When associated with the estimated survival rate for adolescents, mean of 11 years (11), we obtained a QALY of 4.488. With re-transplantation, rehabilitation provided the patient out of 11 years of survival approximately 4.5 years of life in good health. Addendum that the neurological status at hospital discharge showed no changes and was correlated with the general outcome.
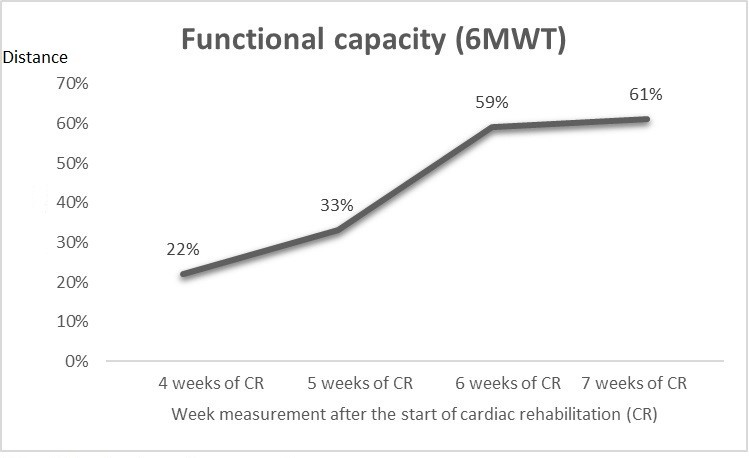
Figure 3. Functional capacity assessment
6MWT – six-minute walk test
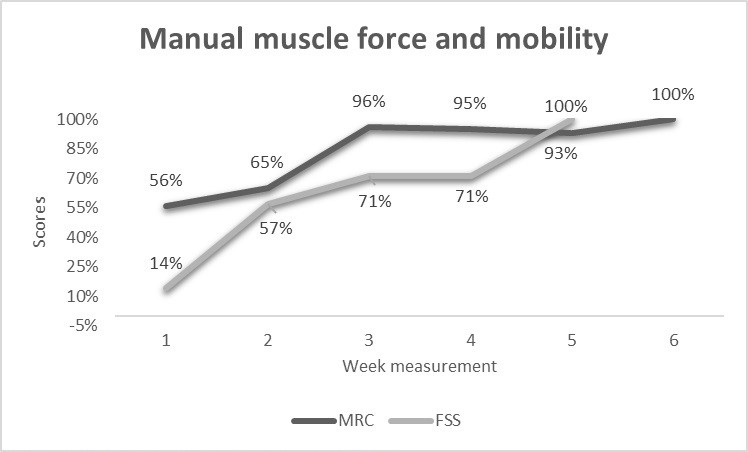
Figure 4. Mobility and manual force assessment
FSS – functional status score, MRC – Medical Research Council
Discussion
The case report showed improvements obtained with exercise prescription in cardiac rehabilitation. The program recovered most predicted normality values for the patient's age and weight. The QALY was 4.5. Respiratory muscle force, vital capacity, and lung function efficacy were optimized. There was an increase in the distance covered in the 6MWT. The patient reached the maximum scores on mobility and manual muscle force. It was not possible to compare measurements before and after heart transplantation because the patient was on hemodynamic circulatory assistance. It was very complicated case and rehabilitation was successful.
Patients on ECMO are subject to adverse effects. Overuse of ECMO should be avoided (12). There are few reports on early cardiac rehabilitation in pediatric patients with ECMO (12). To the best of the author's knowledge, nothing has been described on the board of unexpected myocardial recovery.
Although the guidelines for care of heart transplantation do not specify a pediatric cardiac rehabilitation program (6), extrapolations from the recommendations to the adult population are feasible. Aerobic exercise training and resistance exercise (6) were part of the intervention.
A systematic review summarized disabilities in pediatric post-heart transplantation (14). Data collected after the procedure showed improvements in short and long-term exercise capacity, force, and flexibility (14). Hospital cardiac rehabilitation increases functional capacity, improves physical body composition, and generates quality-of-life gains (5, 15).
Exercise prescription in a cardiac rehabilitation program for transplant patients initiated before and/or immediately after transplantation, the average gain in the distance covered by the 6MWT at the end of treatment was 175.70 (170.31) meters (15). In the present paper, there was an increase of 280 meters, corroborating with the distance gain described in the literature. The patient did not reach the value predicted by the age group in the 6MWT. The significant pain complaints from a sacral ulcer were a restrictive factor in the patient's rehabilitation.
The current concept of rehabilitation is broad, including the respiratory part. Common changes in the postoperative period of cardiac surgery include decreased oxygenation, respiratory muscle force, lung function, and atelectasis (16). These factors are frequently present in the case described. The patient's initial vital capacity was close to mechanical ventilation indication value. Physiotherapeutic performance in the pulmonary field was important, as the patient recovered maximum inspiratory and expiratory pressures, vital capacity, and lung function efficacy. Complications were lower by using non-invasive ventilation.
The relevance of a physical therapy intervention after cardiac surgery is unquestionable. A specific population, such as pediatric re-transplantation, requires all multidisciplinary team attention. Exercise prescription in cardiac rehabilitation conducted by a physiotherapist team can prevent potential morbidity and mortality. It highlights the importance of future studies in this population with larger sample sizes, comparability before and after re-transplantation, and longer follow-up times (hospital, outpatient, and home rehabilitation).
The program implemented evidenced gains in all markers, preventing potential morbidities and reflecting on the patient's clinical improvement. The positive results corroborate the scarce literature on this subject in the pediatric population. The case report supports an effective recovery treatment of a pediatric cardiac re-transplantation, presenting the step by-step of the proposed exercise prescription in a cardiac rehabilitation program.
Ethics: The Ethics and Research Committee approved this case report. The child's father provided informed consent, and the child assented.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: R.S.T. and F.A.M.S. equally contributed case management and to preparation of case report
Acknowledgment: We thank the team of physiotherapists from the National Institute of Cardiology for their support
Funding: None to declare
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

