Comprehensive assessment of the quality of life in patients with breast cancer during neoadjuvant chemotherapy
ORIGINAL RESEARCH ARTICLE
Comprehensive assessment of the quality of life in patients with breast cancer during neoadjuvant chemotherapy
Article Summary
- DOI: 10.24969/hvt.2024.452
- CARDIOVASCULAR DISEASES
- Published: 06/01/2024
- Received: 23/10/2023
- Revised: 06/12/2023
- Accepted: 09/12/2023
- Views: 4602
- Downloads: 3587
- Keywords: cardiotoxicity, neoadjuvant chemotherapy, quality of life, breast cancer, cardiac monitoring, Eastern Cooperative Oncology Group scale
Address for Correspondence: Firdavsdzhon R. Akildzhonov, Clinical diagnostic department of National Medical Research Center for Cardiovascular Surgery named after A.N. Bakulev, Rublevskoe highway, 135, Moscow, 121552, Russian Federation
E-mail: firdavs96_tths@mail.ru; Mobile: +7 999 450 46 42
ORCID : Firdavsdzhon R. Akildzhonov 0000-0002-1675-4216; Yuri I. Buziashvili 0000-001-7016-7541; Ivan S. Stilidi 0000-0002-5229-8203; Elmira U. Asymbekova 0000-0002-5422-2069; Elena V. Artamonova 0000-0001-7728-9533; Simon T. Matskeplishvili 0000-0002-5670-167X; Elvina F. Tugeeva 0000-0003-1751-4924; Nazli K. Akhmedyarova 0000-0001-7157-6312
Yuri I. Buziashvili1, Ivan S. Stilidi2, Elmira U. Asymbekova1, Simon T. Matskeplishvili1, Elvina F. Tugeeva1, Nazli K. Akhmedyarova1, Elena V. Artamonova3, Firdavsdzhon R. Akildzhonov1
1Clinical Diagnostic Department, National Medical Research Center for Cardiovascular Surgery named after A.N. Bakulev (director – academician of the Russian Academy of Sciences Golukhova E.Z.), Ministry of Health of Russia, Moscow, Russian Federation
2National Medical Research Center of Oncology named after N.N. Blokhin, Moscow, Russian Federation
3Chemotherapy Department, National Medical Research Center for Oncology named after N.N. Blokhin, Moscow, Russian Federation
Abstract
Objective: Advances in cancer treatment over the past decades have improved long-term patient survival but increased the incidence of chemotherapy-associated cardiotoxicity (CAC). The study of quality of life (QoL) indicators is becoming a relevant and integral subject for the management of patients receiving high doses of antitumor therapy. In particular, CAC carries a high burden on the healthcare system and the patient's daily lifestyle due to a decrease in the body's functional capacity. Due to the increasing life expectancy of patients with cancer, the issues of maintaining a high QoL are becoming increasingly important. The purpose of the study is to conduct a comprehensive assessment of QoL in patients with breast cancer during neoadjuvant chemotherapy (NAC).
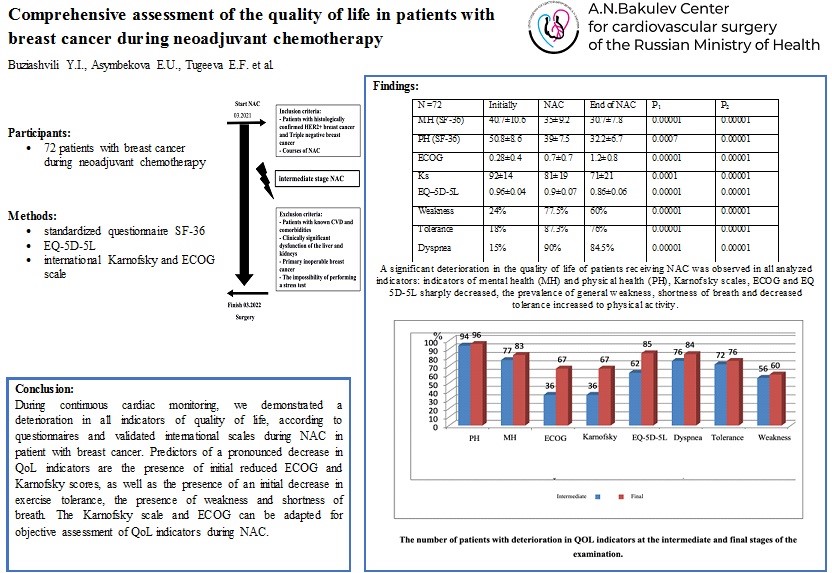
Methods: The study included 72 patients with breast cancer who underwent a comprehensive assessment of the cardiovascular system at the National Medical Research Center for Cardiovascular Surgery. A.N. Bakulev" as continuous cardiac monitoring during NAC. To assess the quality of life, all patients filled out the standardized questionnaire SF-36, EQ-5D-5L, as well as indicators on the international Karnofsky and ECOG (Eastern Cooperative Oncology Group) scales. The possible relationship between various indicators of the questionnaire with internationally validated scales, as well as data from the clinical status of patients, was studied.
Results: A significant deterioration in the QoL of patients receiving NAC was observed in all analyzed indicators: mental and physical health indicators, Karnofsky scores, ECOG and EQ 5D-5L sharply decreased, the prevalence of general weakness, shortness of breath and decreased exercise tolerance increased. According to scale SF-36, initially low indicators were observed in a large number of patients (80 and 82%, respectively); at the intermediate and final stages, almost all patients showed a deterioration in their condition compared to the outcome (p = 0.0002–0.0001). Predictors of a pronounced negative deviation in QoL indicators are the presence of initial reduced ECOG and Karnofsky scores, as well as the presence of an initial decrease in exercise tolerance, the presence of weakness and shortness of breath.
Conclusion: During continuous cardiac monitoring, we demonstrated a deterioration in all indicators of QoL, according to questionnaires and validated international scales during NAC in patient with breast cancer. Predictors of a pronounced decrease in QoL indicators are the presence of initial reduced ECOG and Karnofsky scores, as well as the presence of an initial decrease in exercise tolerance, the presence of weakness and shortness of breath. The Karnofsky scale and ECOG can be adapted for objective assessment of QoL indicators during NAC.
Key words: cardiotoxicity, neoadjuvant chemotherapy, quality of life, breast cancer, cardiac monitoring, Eastern Cooperative Oncology Group scale
Graphical abstract
Introduction
Cardio-oncology is an emerging field of cardiology that specializes in cardiovascular disease in cancer patients. The classical paradigm of cardio-oncology is the prevention, diagnosis and treatment of cardiotoxicity resulting from chemotherapy and/or radiation therapy. Diagnosis and treatment of primary and metastatic cardiac tumors, as well as cardiac amyloidosis, can be considered “less classical” tasks of cardio-oncology. Overall, the management of patients with cancer is complex and requires a multidisciplinary team approach involving oncologists, surgeons, radiologists and cardiologists.
Progress in the treatment of cancer over the past decades has improved long-term patient survival, but has increased the incidence of chemotherapy-associated cardiotoxicity (CAC) (1). Standard chemotherapy regimens have traditionally included anthracyclines such as doxorubicin and epirubicin, and more recently targeted therapies, such as the HER2-targeted monoclonal antibodies trastuzumab and pertuzumab. As targeted therapy develops, there is a steady increase in survival rate in patients with cancer, but the incidence of adverse cardiovascular complications also progresses (2). Signs of cardiotoxicity, such as a significant decrease in left ventricular ejection fraction (LVEF) with the development of progressive heart failure (HF), are the main adverse events associated with neoadjuvant chemotherapy (NAC), especially in combination with anthracyclines. In particular, HF imposes a high burden on the health care system and the patient's lifestyle due to a decrease in the functional capacity of the body. In addition to the significant clinical manifestations associated with NAC, rates of cardiovascular complications and in-hospital mortality in patients are high.
Accordingly, there is increasing practical and scientific interest in the early identification of CAC to improve the prognosis and maintain optimal quality of life (QoL) in patients during NAC. The study of QoL indicators is becoming a relevant and integral subject for the management of patients receiving high doses of antitumor therapy.
QoL is a patient’s assessment of the impact of the disease itself and the treatment on his physical, psychological, emotional and social functioning, and is associated with clinical endpoints, which makes this indicator highly significant in ongoing clinical trials. According to international clinical guidelines, the most validated and widespread questionnaires for a comprehensive assessment of the QoL of patients during NAC are SF-36, as well as the 5L questionnaire for assessing quality of life EQ-5D (3 – 4).
To improve a personalized approach to treatment in patients receiving NAC, the purpose of our study is to evaluate their quality of life indicators in continuous cardiac monitoring during NAC.
Methods
Study design and population
The observational prospective cohort study included 72 patients with a confirmed diagnosis of breast cancer (BC) during NAC, who underwent a comprehensive assessment of the cardiovascular system (CVS) at National Medical Research Center for Cardiovascular Surgery A.N. Bakulev, as continuous cardiac monitoring from March 2021 to February 2022, the average age of all patients was 47.9 (11.9) years, the stages of the tumor process varied between I and IV. The inclusion and exclusion criteria are presented in Figure 1.
All patients included in the study signed informed consent for voluntary participation in the survey. The study was approved by the local ethics committee of the National Medical Research Center for Cardiovascular Surgery A.N. Bakulev.
Baseline clinical characteristics
Demographic (age), anamnestic, complaints, physical examination and exhocardiographic and clinical data (symptoms such as fatigue, nausea/vomiting, weakness, decreased exercise tolerance, and shortness of breath; smoking, hypertension, were assessed.
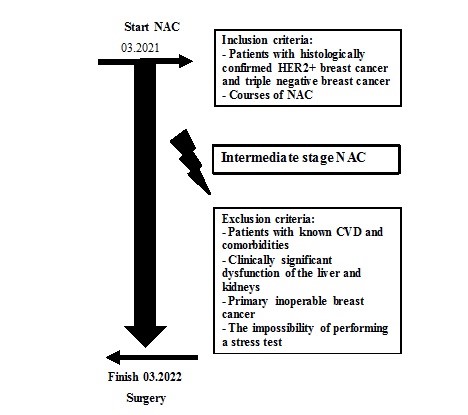
Figure 1. Study design
Protocol of the study
Clinical research methods included the collection of clinical and anamnestic data by patient interview method: symptoms such as fatigue, nausea/vomiting, weakness, decreased exercise tolerance, and shortness of breath.
To assess QOL, questionnaires SF-36, EQ-5D-5L (modified version for Russia) were used, and assessments were also carried out according to the international Karnofsky and ECOG scales. During the scheduled appointment, patients were given questionnaires and scales, which they filled out. The survey was carried out before the start of NAC, after the 4th course, and also after completion of the NAC courses (Fig.1).
Chemotherapy
All patients received combined NAC in the PH-FECH regimen: 12 courses of paclitaxel (80 mg/m2) plus trastuzumab, followed by four 21-day courses of 5-fluorouracil (500 mg/m2), epirubicin (75 mg/m2), and cyclophosphamide (500 mg/m2) plus trastuzumab. Chemotherapy courses were carried out once every 2 weeks. These control points were optimal for assessing functional and symptomatic variables. The primary end-point in our prospective study was change in QoL after treatment. The correlation between parameters of subclinical cardiotoxicity and quality of life will be presented in the next article as “markers of cardiotoxicity”.
Quality of life questionnaires
To assess QOL, questionnaires SF-36, EQ-5D-5L (modified version for Russia) were used, and assessments were also carried out according to the international Karnofsky and ECOG scales.
The EQ-5D-5L questionnaire assesses the state of health studied in five areas: the ability to move in space; personal care; usual daily activities; pain or discomfort; anxiety and depression. The multidimensionality of this questionnaire implies an assessment of all main areas of human life. EQ-5D identifies five such areas, which makes it possible to differentiate the impact of the disease and the treatment on the patient’s condition.
Easier and also frequently used methods for assessing the level of daily activity are the Karnofsky scale and its modification, which allows assessment of the general somatic ECOG status. ECOG scale 0 - the patient is fully active, able to perform everything as before the disease (90-100 points on the Karnofsky scale); 4 - disabled person, completely incapable of self-care, confined to a chair or bed (10-20 points on the Karnofsky scale).
The SF-36 questionnaire (Medical Outcomes Study Short-Form 36) is the most common standardized questionnaire for studying QOL in the population, allowing to assess various components of a patient’s life. If you have perfect physical and mental health, your scores are on a 50 mean/10 standard deviation scale.
Statistical analysis
Statistical analysis was carried out using the Statistica 10.0 application package and Excel Microsoft. The results are presented as mean (standard deviation), median values. After determining the normality of distribution according to the Kolmogorov-Smirnov, Lilliefors and Shapiro-Wilk indices, statistical processing was carried out using the Mann-Whitney test, Fisher test for non-parametric variables, Student's test, calculation of the correspondence coefficient χ2, odds ratio and relative risk. The indicators were considered statistically significant at a significance level of p<0.05.
Results
Clinical characteristics (Table 1)
The average age of all patients was 47.9 (11.9) years, the stages of the tumor process varied between I and IV, with most often grate T2, comprising 45%, majority of patients had no metastases, and lymph node involvement (N1) was detected in 47% of patients. Family history of CVD was present in 15% of patients. Patients had preserved ejection fraction.
Changes in the QOL in patients with BC during treatment with NAC
The QoL was analyzed in 72 patients with BC during NAC. It was shown that during NAC, there was a significant decrease in the physical and mental health of patients, and symptoms such as fatigue, weakness, decreased exercise tolerance and shortness of breath were pronounced. There was a significant increase in dyspnea and a decrease in exercise tolerance after NAC (p=0.0001). During the observation period, the patients showed signs of irritability and nervousness, which certainly affected the change in psycho-emotional state. A significant deterioration in the quality of life of patients receiving NAC was observed in all analyzed indicators: indicators of mental health (MH) and physical health (PH), Karnofsky scales, ECOG and EQ 5D-5L sharply decreased, the prevalence of general weakness, shortness of breath and reduced exercise tolerance increased (all p=0.0001) (Table 2).
|
Table 1. Clinical and demographic characteristics of patients |
||
|
Variables |
Absolute number |
% |
|
Number of patients |
72 |
100 |
|
Age, years |
47.9 (11.9) |
|
|
T1 |
15 |
20.8 |
|
T2 |
33 |
45.8 |
|
T3 |
13 |
18.1 |
|
T4 |
11 |
15.3 |
|
M0 |
70 |
97.2 |
|
M1-2 |
2 |
2.8 |
|
N0 |
29 |
40.3 |
|
N1 |
34 |
47.2 |
|
N2 |
4 |
5.5 |
|
N3 |
5 |
7.0 |
|
Impaired glucose tolerance, |
1 |
1.4 |
|
Smoking |
14 |
19.4 |
|
Dyslipidemia |
8 |
11.1 |
|
Obesity |
6 |
8.3 |
|
Family history of CVD |
11 |
15.3 |
|
EDVi, ml/m2 |
86.2 (17.0) |
|
|
ESVi, ml/m2 |
34.2 (8.2) |
|
|
LVEF, % |
60.4 (3.7) |
|
|
Data are presented as mean (SD) and n(%) CVD – cardiovascular diseases, EDVi – indexed end-diastolic volume, ESVi indexed end-systolic volume, LVEF – left ventricular ejection fraction, M – distant metastases, N – regional lymph nodes, T – primary tumor |
||
|
Table 2. Quality of life indicators initially, during and after NAC (n =72) |
|||||
|
VAriables |
Initially |
NAC |
End of NAC |
P1 |
P2 |
|
MH (SF-36) |
40.7 (10.6) |
35 (9.2) |
30.7 (7.8) |
0.00001 |
0.00001 |
|
PH (SF-36) |
50.8 (8.6) |
39 (7.5) |
32.2 (6.7) |
0.0007 |
0.00001 |
|
ECOG |
0.28 (0.4) |
0.7 (0.7) |
1.2 (0.8) |
0.00001 |
0.00001 |
|
Ks |
92 (14) |
81 (19) |
71 (21) |
0.0001 |
0.00001 |
|
EQ–5D-5L |
0.96 (0.04) |
0.9 (0.07) |
0.86 (0.06) |
0.00001 |
0.00001 |
|
Weakness |
24% |
77.5% |
60% |
0.00001 |
0.00001 |
|
Tolerance |
18% |
87.3% |
76% |
0.00001 |
0.00001 |
|
Dyspnea |
15% |
90% |
84.5% |
0.00001 |
0.00001 |
|
Ks – Karnofsky scale, MH – mental health, NAC – neoadjuvant chemotherapy, PH – physical health, P1 – between start and intermediate courses, P2 – between intermediate and final courses
|
|||||
Initially, a certain number of patients had disturbances in QOL indicators that were not associated with the planned NAC: these were 20 patients with low Karnofsky and ECOG scale scores (28%), 22 – EQ-5D-5L (31%), 11 patients had shortness of breath (15.5%), 17 – weakness (23.9%), and 13 had reduced exercise tolerance (13.3%) (Table 3).
|
Table 3. Number of patients with QOL indicators below normal at baseline, at the intermediate and final stages of examinations (N=72) |
||||||||
|
Variables |
Initially |
IC |
FC |
Ps-i |
Pi-f |
|||
|
n |
% |
n |
% |
n |
% |
|||
|
SF-36 (MH) |
57 |
79.2 |
70 |
97.2 |
71 |
98.6 |
0.0002 |
0.39 |
|
SF-36 (PH) |
58 |
80.5 |
71 |
98.6 |
71 |
98.6 |
0.0002 |
1.0 |
|
ECOG |
20 |
27.7 |
37 |
51.3 |
52 |
72.2 |
0.003 |
0.009 |
|
Ks |
20 |
27.7 |
37 |
51.3 |
52 |
72.2 |
0.005 |
0.009 |
|
EQ-5D-5L |
22 |
30.5 |
56 |
77.7 |
68 |
94.4 |
0.00001 |
0.002 |
|
Dyspnea |
11 |
22.2 |
64 |
88.8 |
60 |
83.3 |
0.00001 |
0.31 |
|
Tolerance |
13 |
25 |
62 |
86.1 |
54 |
75 |
0.00001 |
0.08 |
|
Weakness |
17 |
23.6 |
55 |
76.3 |
43 |
59.7 |
0.00001 |
0.02 |
|
FC – final courses, IC – intermediate courses, Ks – Karnofsky scale, MH – mental health, PH – physical health, QoL – quality of life Ps-i – between start and intermediate courses, Ps-f – between start and final courses, Pi-f – between intermediate and final courses |
||||||||
When comparing the intermediate and final courses with the initial state, a deterioration in all indicators of QoL was revealed. According to PH and MH of SF-36, initially low indicators were observed in a large number of patients (80 and 82%, respectively); at the intermediate and final stages, almost all patients showed a deterioration in their condition compared to the outcome (p = 0.0002 – 0.0001). Patients with low ECOG scores and at the intermediate stage increased by 1.85 times, at the final stage – by 2.6 times compared to the outcome (p = 0.003, p = 0.0001); according to the Karnofsky scale, respectively, by 1.85 and 2.6 times (p = 0.005 and 0.00001); according to EQ-5D-5L – 2.54 and 3.1 times (p = 0.00001). Complaints of weakness, decreased exercise tolerance and shortness of breath were also noted, respectively, 3.23, 5.1 and 5.6 times more often at the intermediate stage, and 2.5, 4.2 and 5.2 times after the end of NAC. When comparing the number of patients with low QoL scores between mid- and final stages, statistical significance was obtained only for ECOG, Karnofsky scale, EQ-5D-5L and frailty.
Taking into account the presence of a decrease in QoL indicators already at the first initial stage of the survey, an analysis of the negative dynamics of indicators from stage to stage was carried out (Fig. 2).
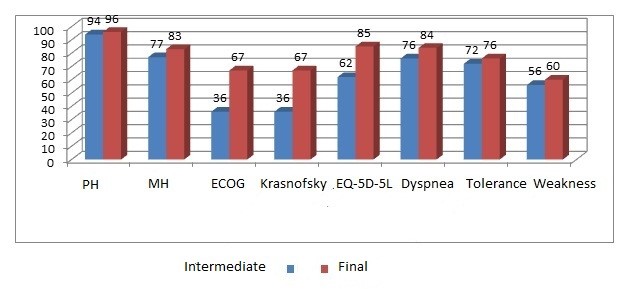
Figure 2. The number of patients with deterioration in QoL indicators at the intermediate and final stages of the examination
QoL – quality of life
As can be seen from the Figure 2, a deterioration of QoL in all indicators is noted already at the intermediate stage; in the future, subjective indicators do not change significantly, while according to ECOG, the Karnofsky scale and EQ-5D-5L, further deterioration in quality of life is observed during NAC (p = 0.0002).
Determination of the influence of the initial state of quality-of-life indicators on predicting the negative impact of NAC
The Karnofsky scale and ECOG showed themselves to be more objective markers of QOL indicators and, accordingly, they were accepted for further analysis. Among all the examined individuals, according to the Karnofsky and ECOG scales, 20 women did not show a deterioration in QOL indicators at all stages of the examination, and 52 had a significant deterioration in their condition. To determine predictors of decreased QoL during NAC, these groups of patients were considered separately, groups 1 and 2, respectively.
|
Table 4. Comparative characteristics of indicators in patients with and without deterioration in QOL |
||||||
|
Variables |
Groups |
Start |
IC |
FC |
Ps-i |
Pi-f |
|
ECOG |
1 group |
1.0 (0) |
1.3 (0.5) |
1.54 (0.64) |
0.0000 |
0.16 |
|
2 group |
0 (0) |
0 (0) |
0 (0) |
- |
- |
|
|
P1-2 |
|
0.0004 |
0.0000 |
0.0000 |
|
|
|
Ks |
1group |
88(15) |
74(18) |
59.2 (12.8) |
0.0000 |
0.0000 |
|
2 group |
100(0) |
100(0) |
100(0) |
- |
- |
|
|
P1-2 |
|
0.0009 |
0.0000 |
0.0000 |
|
|
|
EQ–5D-5L |
1group |
0.96 (0.04) |
0.9(0.06) |
0.86(0.06) |
0.0000 |
0.001 |
|
2 group |
0.98 (0.04) |
0.91(0.04) |
0.87(0.08) |
0.0000 |
0.05 |
|
|
P1-2 |
|
0.06 |
0.5 |
0.5 |
|
|
|
SF-36 (PH) |
1group |
49.1(22.9) |
39(18) |
31(14) |
0.01 |
0.01 |
|
2 group |
54.4(27.2) |
40(20) |
35.5(16.2) |
0.07 |
0.45 |
|
|
P1-2 |
|
0.4 |
0.84 |
0.25 |
|
|
|
SF-36 (MH) |
1group |
40 (12.6) |
35(9.1) |
30.7 (8.3) |
0.02 |
0.01 |
|
2 group |
42.1 (8.6) |
37 (9.6) |
30.5 (6.5) |
0.09 |
0.01 |
|
|
P1-2 |
|
0.52 |
0.42 |
0.92 |
|
|
|
Weakness
|
1group |
31% |
73.1% |
69.2% |
0.0000 |
0.6 |
|
2 group |
5.3% |
89.5% |
36.8% |
0.0000 |
0.0007 |
|
|
P1-2 |
|
0.02 |
0.14 |
0.01 |
|
|
|
Decreased tolerance |
1group |
25% |
86.5% |
90.4% |
0.0000 |
0.53 |
|
2 group |
0% |
89.5% |
36.8% |
0.0000 |
0.0008 |
|
|
P1-2 |
|
0.01 |
0.73 |
0.0000 |
|
|
|
Dyspnea
|
1group |
21% |
90% |
92% |
0.0000 |
0.72 |
|
2 group |
0% |
89.5% |
63.2% |
0.0000 |
0.05 |
|
|
P1-2 |
|
0.02 |
0.95 |
0.003 |
|
|
|
FC – final courses, IC – intermediate courses, Ks – Karnofsky scale, MH – mental health, PH – physical health, QoL – quality of life Ps-i – between start and intermediate courses, Ps-f – between start and final courses, Pi-f – between intermediate and final courses |
||||||
Table 4 shows QOL indicators by stage in two groups of patients. All indicators (p<0.05), except the Karnofsky and ECOG scales, decreased significantly in both groups of patients. Differences between the groups were noted only in weakness, shortness of breath and exercise tolerance at baseline and at the final stage.
To determine prognostic markers of QoL deterioration, an analysis was carried out to determine the correspondence index χ 2 and the relative risk of the indicators under consideration as shown in Table 5.
|
Table 5. The significance of the initial state of QOL on the development of negative changes during NAC (n=72) |
||||||||
|
Test |
|
MH |
PH |
ECOG and Ks |
EQ–5 D-5L |
Weakness |
Dyspnea |
Tolerance |
|
χ2 test |
|
1.54 |
0.01 |
10.1 |
2.8 |
4.6 |
4.7 |
5.8 |
|
R |
0.21 |
0.99 |
0.002 |
0.09 |
0.03 |
0.03 |
0.01 |
|
|
Fisher criterion |
|
0.28 |
1.00 |
0.0007 |
0.14 |
0.05 |
0.029 |
0.014 |
|
P |
>0.05 |
>0.05 |
<0.05 |
>0.05 |
>0.05 |
<0.05 |
<0.05 |
|
|
Relative risk (RR) |
|
1.19 |
0.99 |
1.59 |
1.28 |
1.4 |
1.46 |
1.48 |
|
95%CI |
0.91-1.6 |
0.71-1.4 |
1.29 -2.0 |
0.99 -1. 7 |
1.1-1.7 |
1.23-1.7 |
1.24-1.8 |
|
|
Sensitivity |
0.48 |
0.78 |
0.38 |
0.36 |
0.30 |
0.21 |
0.25 |
|
|
Specificity |
0.68 |
0.21 |
1.00 |
0.84 |
0.95 |
1.00 |
1.00 |
|
|
Ks – Karnofsky scale, MH – mental health, NAC – neoadjuvant chemotherapy, PH – physical health, QoL – quality of life |
||||||||
As can be seen from Table 5, significant predictors of QoL deterioration were ECOG and Ks scores (RR1.59 (95CI 1.29-2.0)), followed by the presence of low exercise tolerance (RR 1.48), shortness of breath (RR 1.46) and weakness (1.4) in descending order. That is, before the start of NAC, a decrease in these particular QOL indicators turned out to be unfavorable prognostic markers. It should be noted that the sensitivity is quite low with high specificity.
Thus, the use of NAC in patients with breast cancer was accompanied by a significant deterioration in quality of life. The use of various questionnaires and scales, as well as subjective complaints of patients, as a tool for assessing QoL is legitimate; for all assessment methods, a significant decrease in these indicators is noted. Predictors of a pronounced negative deviation in QoL indicators are the presence of initial reduced ECOG and Karnofsky scale, as well as the presence of an initial decrease in exercise tolerance, the presence of weakness and shortness of breath.
Discussion
With significant increases in cancer survival rates treated with high-dose anticancer drugs, the long-term consequences of systemic chemotherapy are an important consideration in a public health context. In addition, it is important to recognize that the QoL of cancer patients mainly depends on the state of the cardiovascular system, the management of which is an important part of personalized patient management, which improves survival in this category of patients. According to the World Health Organization definition, “Human health is a state of complete physical, mental and social well-being and not merely the absence of disease” and has six dimensions: bodily functions, mental functions and perceptions, spiritual dimensions, QoL, social participation and daily functioning (5). Previous QoL studies have focused on the specific cancer burden associated with nausea, pain, somnolence, and anxiety disorders (6). According to the world literature, data on a comprehensive assessment of QoL in patients during NAC are limited. A randomized, single-center study showed that patients with early-stage breast cancer disproportionately experience a decline in QoL and functional status due to progression of heart failure (7). It is important to note that the severe course of the disease and the steady progression of symptoms have a negative impact on the daily life of patients, on relationships with family, the ability to work and ensure their financial well-being, which significantly reduces the QoL in this category of patients. In modern clinical practice, assessing QoL in patients with various diseases is a pressing issue, since for the patients themselves, the effectiveness of the therapy is important not only in slowing down the progression of the disease, but also in maintaining their adaptation in society and the ability to lead everyday life.
Modern scales for assessing the condition of patients allow for a deep multifaceted analysis of physiological, psychological, emotional and social disorders. A large number of standardized and approved questionnaires have been developed to assess the functional, role, emotional, and social state of patients, including cancer patients. Among them are the EQ-5D-5L scales and the SF-36 questionnaire, but none are adapted for assessing the condition of patients during NAC. Also, to assess general somatic health, the dynamics of the general condition of patients was studied using the Karnofsky and ECOG Performance Status scale.
A small number of studies have been published in the literature that would evaluate QoL in patients during NAC. Thus, in a study by Gersak et al. (8), in order to improve personalized treatment of patients with chemotherapy, the degree of connection between selected QoL indicators and both clinical and instrumental data indicators were assessed. In a randomized study, 59 patients aged 18 to 80 years were assessed before chemotherapy and at several follow-up visits using the EQ-5D-5L and SF-36 questionnaires. The results of this study revealed reduced indicators of QoL, which require continuous monitoring. It has also been shown that regular assessment of QoL can significantly improve physical and cognitive outcomes, reducing the burden on the healthcare system (8). In the world literature, data on the use of these scales in patients during NAC are limited.
The Russian-language version of the EQ-5D-5L questionnaire (EuroQOL) was registered in 2009. It has been validated and is currently used in clinical trials in cancer patients (9). According to our study, the questionnaire is sensitive to changes; accordingly, it allows for constant monitoring of the dynamics of QOL parameters over time and, if necessary, correction of therapy. The patient’s participation in assessing his own condition is especially important when studying QOL, since it allows for a complete and objective picture of the disease and corresponds to the concept of patient-centered medicine.
QoL may, in addition to its original purpose for early detection and prediction of cardiotoxicity, provide additional screening, either when used with or without questionnaire-based tools. In this context, the dynamics of QoL indicators can serve as an early marker of the effect of NAC on the cardiovascular system, which forms an integral part of the patient’s health. This would provide the clinician with valuable objective information about an important component of the patient's overall QoL score, which, with timely cardioprotective therapy, would lead to improved survival rates and less burden on the healthcare system.
The associations identified in our study with decreased exercise tolerance, shortness of breath, and general weakness are comparable to existing global data. To monitor the state of QoL during NAC, you can use the SF-36, EQ-5D-5L questionnaire as one of the additional methods for assessing disease progression and the effectiveness of therapy. Assessment of QoL using the Karnofsky and ECOG scales was more informative and objective. They were significant in predicting a significant deterioration in QoL during NAC. Further study of the use of SF-36, EQ-5D-5L in a large cohort of patients over a long period of time is required. Our results are consistent with the world literature on the study of QoL in patients with breast cancer after NAC (10).
Study limitations
Limitations in our study include the short follow-up period, the lack of availability of echocardiographic and clinical laboratory research methods and their correlation.
Conclusion
1.During continuous cardiac monitoring, we demonstrated a deterioration in all indicators of QoL, according to questionnaires and validated international scales during NAC in patients with BC.
2.Initially low parameters according to ECOG and Karnofsky scales, as well as the presence of initially low tolerance to physical activity, the presence of weakness and shortness of breath in patients with breast cancer are early markers of worse tolerability of NAC.
3.The Karnofsky scale and ECOG can be adapted for objective assessment of QOL indicators during NAC in patients with BC.
Ethics: All patients included in the study signed informed consent for voluntary participation in the survey. The study was approved by the local ethics committee of the National Medical Research Center for Cardiovascular Surgery A.N. Bakulev
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: Y.I.B., I.S. S., E.U.A., S.T. M., E.F.T., N.K.A., E.V.A., and F.R. A. equally contributed to the study and fulfilled authorship criteria
Acknowledgement and Funding: None to declare
References
| 1. Piper S, McDonagh T. Chemotherapy-related cardiomyopathy. Eur Cardiol 2015; 10: 19-24. doi:10.15420/ecr.2015.10.01.19 https://doi.org/10.15420/ecr.2015.10.01.19 PMid:30310418 PMCid:PMC6159418 |
||||
| 2. Kreutzfeldt J, Rozeboom B, Dey N, De P. The trastuzumab era: current and upcoming targeted HER2+ breast cancer therapies. Am J Cancer Res 2020; 10: 1045-67. | ||||
| 3.Akulova AI, Gaidukova IZ, Rebrov AP. Validation of version 5L of the EQ-5D questionnaire in Russia. Sci Pract Rheumatol 2018; 56: 351-5. doi: 10.14412/1995-4484-2018-351-355 https://doi.org/10.14412/1995-4484-2018-351-355 |
||||
| 4. Chatzinikolaou A, Tzikas S, Lavdaniti M. Assessment of quality of life in patients with cardiovascular disease using the SF-36, MacNew, and EQ-5D-5L questionnaires. Cureus 2021; 13: e17982 doi:10.7759/cureus.17982 https://doi.org/10.7759/cureus.17982 PMid:34667665 PMCid:PMC8517455 |
||||
| 5. Leonardi F. The definition of health: towards new perspectives. Int J Health Serv 2018; 48: 735-48. doi:10.1177/0020731418782653 https://doi.org/10.1177/0020731418782653 PMid:29902944 |
||||
| 6. Hurria A, Soto-Perez-de-Celis E, Allred J. Functional decline and resilience in older women receiving adjuvant chemotherapy for breast cancer. J Am Geriatr Soc 2019; 67: 920-7. doi:10.1111/jgs.15493 https://doi.org/10.1111/jgs.15493 PMid:30146695 PMCid:PMC6391210 |
||||
| 7. Venturini E, Iannuzzo G, D'Andrea A. Oncology and cardiac rehabilitation: an underrated relationship. J Clin Med 2020; 9: 1810 doi:10.3390/jcm9061810 https://doi.org/10.3390/jcm9061810 PMid:32532011 PMCid:PMC7356735 |
||||
| 8. Gersak B, Kukec A., Steen H. Relationship between quality-of-life indicators and cardiac status indicators in chemotherapy patients. Zdr Varst 2021; 60: 199-209. doi:10.2478/sjph-2021-0028 https://doi.org/10.2478/sjph-2021-0028 PMid:34917188 PMCid:PMC8643110 |
||||
| 9. Borchert K, Jacob C, Wetzel N. Application study of the EQ-5D-5L in oncology: linking self-reported quality of life of patients with advanced or metastatic colorectal cancer to clinical data from a German tumor registry. Health Econ Rev 2020; 10: 40. doi:10.1186/s13561-020-00297-6. https://doi.org/10.1186/s13561-020-00297-6 PMid:33313984 PMCid:PMC7733616 |
||||
| 10. Lewandowska A, Rudzki G, Lewandowski T. Quality of life of cancer patients treated with chemotherapy. Int J Environ Res Public Health 2020;17: 6938. doi:10.3390/ijerph17196938 https://doi.org/10.3390/ijerph17196938 PMid:32977386 PMCid:PMC7579212 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

