Left ventricular perforation by a chest tube: Case report and review of complications
CASE REPORT
Left ventricular perforation by a chest tube: Case report and review of complications
Article Summary
- DOI: 10.24969/hvt.2024.456
- CARDIOVASCULAR DISEASES
- Published: 25/01/2024
- Received: 07/12/2023
- Revised: 12/01/2024
- Accepted: 13/01/2024
- Views: 5029
- Downloads: 3537
- Keywords: Chest tube, pleural effusion, pneumothorax, thoracotomy
Address for Correspondence: Ulises Rojel-Martínez, Arrhythmias and Pacing Unit, Cardiology Service General Hospital “Dr. Eduardo Vázquez Navarro”, South Medical Center, Puebla, Mexico
Email: ulirm@hotmail.com
Ulises Rojel-Martínez, Pablo Andres Reatiga-Vega, Flor Mayranny Marquez-Maldonado, Alan Cordova-Fierro, Karla Bozada-Nolasco
Arrhythmias and Pacing Unit, Cardiology Service General Hospital “Dr. Eduardo Vázquez Navarro”, South Medical Center Puebla, Mexico
Abstract
Objective: The placement of a chest tube to resolve pleural effusion, pneumothorax or as a diagnostic method is a relatively common invasive procedure in the emergency room and hospitalization area, which is not inherent to presenting complications. We present the case of a patient with perforation of the left ventricle secondary to the placement of a chest tube
Case presentation: A 76-year-old male who was admitted to the emergency department with pneumonia and left pleural effusion. A chest tube was placed in pleural space, however, after procedure hemodynamic deterioration occurred and computed tomography (CT) revealed left ventricular perforation. Thoracotomy was performed to remove the catheter and repair the left ventricular puncture site. Although due to hemodynamic instability patient was admitted to intensive care unit with mechanical ventilation, subsequently developed cardiogenic shock. Vasopressor support was needed. An echocardiogram was performed on day 1 after the surgical intervention and showed no evidence of bleeding according to the report. After three days the patient dies from cardiogenic shock.
Conclusion: In conclusion, whenever available, it is better to use a chest CT prior to placement of the chest tube and during the procedure use lung ultrasound to guide the puncture. Special care must be taken when using small caliber probes. Finally, more publications of these complications are required to have more evidence in the management of these cases.
Take home message: Special care must be taken when using small caliber probes. The efficacy of lung ultrasound in guiding chest tube placement, demonstrating it is utility in improving accuracy and reducing complications.
Key words: Chest tube, pleural effusion, pneumothorax, thoracotomy
Introduction
The placement of a chest tube to resolve pleural effusion, pneumothorax or as a diagnostic method is a relatively common invasive procedure in the emergency room and hospitalization area, which is not inherent to presenting complications. These complications may be due to insertion of the pleural tube in 19% (vascular injury, abdominal organs, lung parenchyma, diaphragm, cardiac), malposition of the tube (53%), removal (16%), infection (14%) and dysfunction (<1%). Among the factors associated with immediate complications is the use of chest tubes < 36 FR, with an increase in the risk of complications due to malposition of up to 3 times (1, 2).
We present the case of a patient with perforation of the left ventricle secondary to the placement of a chest tube.
Case report
A 76-year-old male was admitted to the emergency department due to dyspnea, cough and fever. The physical examination showed a blood pressure of 115/65 mmHg, heart rate of 85 bpm, respiratory rate of 22 rpm, intercostal indrawing and oxygen saturation of 93% with support of supplemental oxygen at 3L/min. A chest x-ray (Rx) showed findings suggestive of pneumonia and left pleural effusion; a simple chest computed tomography (CT) confirmed 80% left pleural effusion.
During his stay at the Hospital, a chest tube with a DRENTECH UNICO TM 12 Fr catheter was placed in the 6th intercostal space in the mid-axillary line.
After placement, completely hematic pleural output was obtained and hemodynamic deterioration was present. A CT was performed that allowed to identify a catheter in the left ventricle (LV) with a tip in the left atrium (LA) (Fig. 1A, 1B). Subsequently, the patient was immediately transferred to a hospital with cardiothoracic surgery service available. Upon his admission, an electrocardiogram was performed, which showed sinus rhythm, heart rate of 81 bpm, with T wave inversion from V1 to V4; transthoracic echocardiogram revealed LV perforation in the lateral wall region with a tip located in the LA, systolic dysfunction (LV ejection fraction of 39%), moderate mitral and aortic insufficiency and pericardial effusion with an approximate volume of 900 ml.
A left anterior thoracotomy was performed to remove the chest tube and a polytetrafluoroethylene patch was placed (Fig. 1C, 1D). Due to hemodynamic instability, patient was admitted to intensive care unit with mechanical ventilation, subsequently developed cardiogenic shock. Vasopressor support was needed. An echocardiogram was performed on day 1 after the surgical intervention and showed no evidence of bleeding according to the report. After three days, the patient died from cardiogenic shock.
.
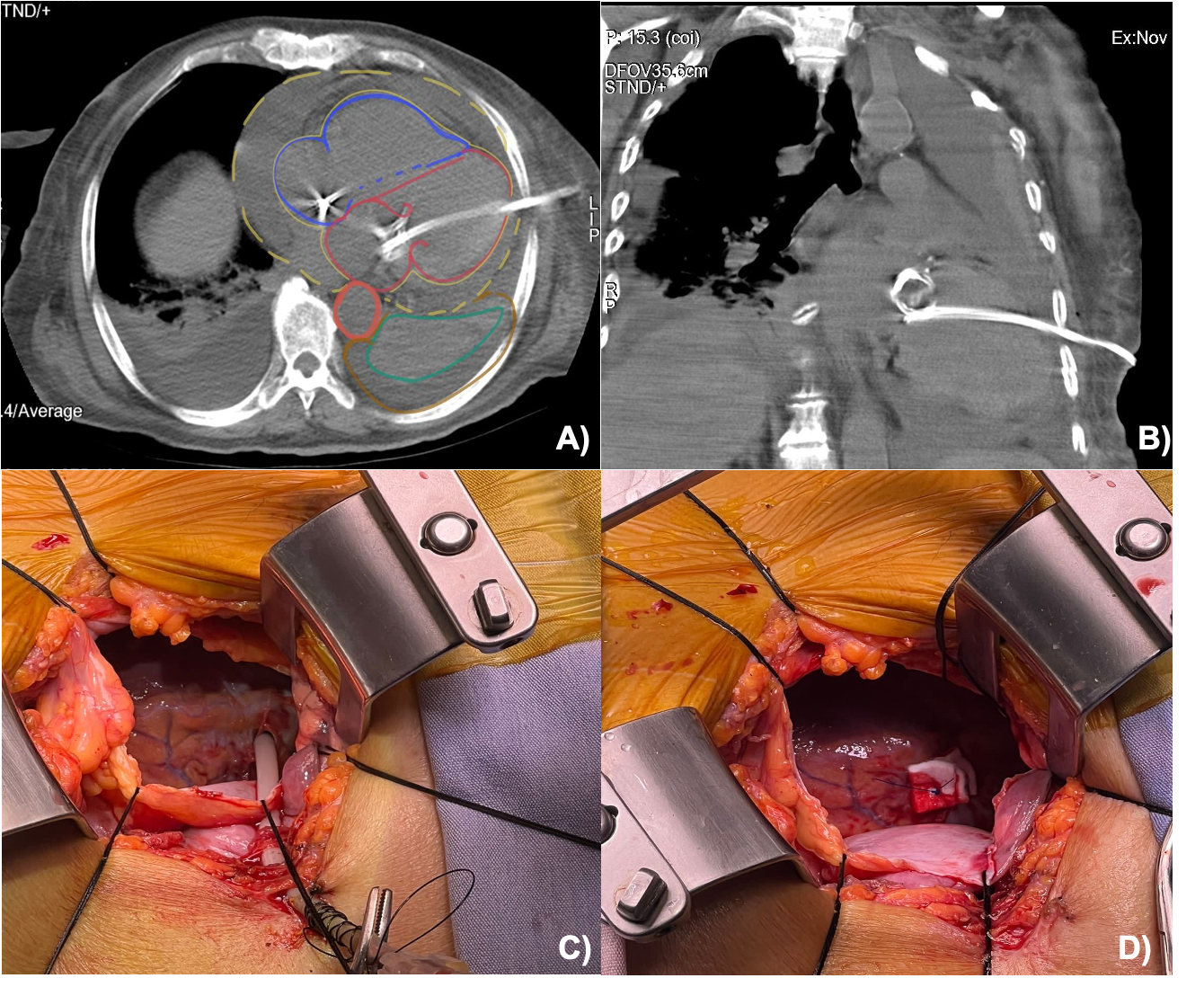
Figure 1. A-B) Computed tomography image of catheter identified in the left ventricle with a tip in the left atrium
C-D) Intraoperative image of left anterior thoracotomy showing removal the chest tube and a placement of polytetrafluoroethylene patch.
Discussion
The placement of a chest tube as a therapeutic or diagnostic measure is not a harmless procedure, the closed technique used initially and is now practically out of use because it is related to a greater number of complications. It consisted of the introduction of a troacar directly into the chest prior to the chest tube without prior digital pleural exploration (3). The open technique consists of making a small incision in the skin, followed by digital exploration identifying the pleura and then introducing the chest tube. To reduce the risks of complications, Advance Trauma Life Support (ATLS) and the British Thoracic Society (BTS) have described a non-standardized anatomical region to orient operator during the procedure, called the “safety triangle”, which is delimited by the anterior edge of the m. latissimus dorsi, the lateral edge of the m.pectoralis major and the horizontal line above the nipple and an apex below the armpit (4). The Bulau lateral approach consists of puncture between the 4th and 6t h intercostal space, anterior to the mid-axillary line and, if possible, guided by a prior imaging study, preferably chest CT, to identify structures or anatomical alterations adjacent to the placement site (5).
The use of lung ultrasound at the time of placement is an excellent alternative since, compared to simple chest X-ray, it increased the probability of successful placement of the chest tube without complications by 26% (6). Few cases of cardiac injury have been described in the literature; during our review we identified 11 cases (Table1); 1 case with LA injury, right atrial and right ventricular injuries in 2 cases each and 6 cases with LV involvement (7-17). It was observed that in the majority of cases where cardiac injury occurred, a closed technique and small catheters (< 16 Fr) were used with a favorable final result for the patient. The ATLS in its 2018 guidelines recommended using 28-32 Fr catheters or a smaller caliber if the effusion is not classified as complex (hemothorax, empyema, post-procedure, etc.). For its part, the BTS in its 2023 pleural disease guidelines only mentions as a recommendation the use of a 14 Fr or smaller catheter in infected pleural effusion (18, 19). In our case, a 22 cm long and 12 Fr diameter catheter with a distal pigtail was used, which was placed through a lateral approach. Despite removal of the catheter and repair of the cardiac lesion, the patient died.
|
Table 1. Reported cases with cardiac injury during chest tuve placement (7-17) |
||||
|
Case |
Age, years |
Perforation site |
Type tube |
Death |
|
1 |
72 |
LA injury |
Matthys catheter (6 F) |
No |
|
2 |
65 |
RA injury |
Unknown |
Yes |
|
3 |
68 |
RA injury |
Unknown |
No |
|
4 |
64 |
RV injury |
32 F |
Yes |
|
5 |
76 |
RV injury |
Unknown |
Yes |
|
6 |
82 |
LV perforation |
Bonanno 14-gauge catheter |
No |
|
7 |
53 |
LV perforation |
Unknown |
No |
|
8 |
72 |
LV perforation |
Braun Pleuracan B 6 F |
No |
|
9 |
27 |
LV perforation |
8 fr catheter |
No |
|
10 |
67 |
LV perforation |
Pleurocathplastimed Laboratoire |
Yes |
|
11 |
76 |
LV perforation |
Unknown |
Yes |
|
12 |
76 |
LV perforation |
DRENTECH UNICO TM 12 Fr |
Yes |
Conclusion
In conclusion, whenever available, it is better to use a chest CT prior to placement of the chest tube and during the procedure use lung ultrasound to guide the puncture. Special care must be taken when using small caliber probes. Finally, greater publication of these complications is required to have more evidence in the management of these cases.
Message to take home
Special care must be taken when using small caliber probes.
The efficacy of lung ultrasound in guiding chest tube placement, demonstrating it is utility in improving accuracy and reducing complications.
Ethics: Informed consent was obtained from patient for all procedures
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: U. R-M., P. A . R-V., F. M. M-M., A. C-F., K. B.-N. equally contributed to case management and preparation of case report
Acknowledgment and Funding: None to declare
References
| 1.Sethuraman KN, Duong D, Mehta S. Complication of tube thoracostomy placement in the emergency department. J Emerg Med 2011; 40: 14-20. https://doi.org/10.1016/j.jemermed.2008.06.033 PMid:19097724 |
||||
| 2. Hernandez M, El Khatib M, Prokop L, Zielinski M, Aho, J. Complications in tube thoracostomy: Systematic review and meta-analysis. J Trauma Acute Care Surg 2018; 85: 410-6. https://doi.org/10.1097/TA.0000000000001840 PMid:29443856 PMCid:PMC6081248 |
||||
| 3. Laws D, Neville E, Duffy J. British Thoracic Society Guidelines for insertion of a chest drain. Thorax 2003; 53: 53-9. https://doi.org/10.1136/thx.58.suppl_2.ii53 |
||||
| 4. Haverlock T, Teoh R, Laws D, Gleeson F. Pleural procedures and thoraci ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65: 61-76. https://doi.org/10.1136/thx.2010.137026 PMid:20696688 |
||||
| 5. Tomlinson M, Treasure T. Insertion of a chest drain: how to do it. Br J Hosp Med 1997; 58: 248-52. | ||||
| 6. Doelken P, Strange C. Chest ultrasound for "Dummies". Chest 2003; 123: 332-3. https://doi.org/10.1378/chest.123.2.332 PMid:12576345 |
||||
| 7. Rajs J, Rotmil, P. Post-mortem finding of a non-fatal left heart ventricular perforation by a pleural drain. A case report. Forens Sci Intern 1981; XX: 37-40. https://doi.org/10.1016/0379-0738(81)90186-9 PMid:7216080 |
||||
| 8. Meisel S, Ram Z, Priel I, Nass D, Lieberman P. Another complication of thoracostomy--perforation of the right atrium. Chest 1990; 98: 772-3. https://doi.org/10.1378/chest.98.3.772 PMid:2132739 |
||||
| 9. Shih C, Chang Y, Lai S. Successful management of perforating injury of right atrium by chest tube. Chin Med J 1992; 50: 338-40. | ||||
| 10. De La Fuente AE. Left ventricular perforation by a pleural drainage tube. Texas Heart Instit J 1994; 21: 175-6. | ||||
| 11. Dominguez Fernandez EE. Perforation of the heart wall--a rare complication after thoracic drainage treatment. Der Chirurg 1995; 66: 920-2. | ||||
| 12. Kopec S, Conlan A, Irwin R. Perforation of the right ventricle: a complication of blind placement of a chest tube into the postpneumonectomy space. Chest 1998; 114: 1213-5. https://doi.org/10.1378/chest.114.4.1213 PMid:9792599 |
||||
| 13. Abad C, Padron A. Accidental perforation of the left ventricle with a chest drain tube. Texas Heart Instit J 2022; XX: 143. | ||||
| 14. Kerger HE. Perforation of the left atrium by a chest tube in a patient with cardiomegaly: management of a rare, but life-threatening complication. Resuscitation 2007; 74: 178-82. https://doi.org/10.1016/j.resuscitation.2006.11.008 PMid:17303305 |
||||
| 15. Asopa SE. Accidental perforation of the left ventricle with a Bonanno catheter. J Thorac Cardiovasc Surg 2009; 137: 1023-4. https://doi.org/10.1016/j.jtcvs.2008.03.029 PMid:19327535 |
||||
| 16. Haron HE. Chest tube injury to left ventricle: complication or negligence? Ann Thorac Surg 2010; 90: 308-9. https://doi.org/10.1016/j.athoracsur.2010.01.075 PMid:20609810 |
||||
| 17. Shin-Kim JE. Left ventricular perforation with catheter decompression. Am J Emerg Med 2019; 37: 377.e5-e6. https://doi.org/10.1016/j.ajem.2018.10.055 PMid:30413368 |
||||
| 18. Roberts ME, Rahman NM, Maskell NA. British Thoracic Society. British Thoracic Society Guideline for pleural disease. Thorax 2023; 0: 1-34. https://doi.org/10.1136/thorax-2022-219784 PMid:37433578 |
||||
| 19. American College of Surgeons, Committee on Trauma. ATLS Advance Trauma Life Support, 10° Edition. 2018. | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

