The 24th organ: the aorta. The main concept of new EACTS/STS Guidelines
EDITORIALS
The 24th organ: the aorta. The main concept of new EACTS/STS Guidelines
Article Summary
- DOI: 10.24969/hvt.2024.481
- Page(s): 175-177
- CARDIOVASCULAR DISEASES
- Published: 21/04/2024
- Received: 02/04/2024
- Accepted: 03/04/2024
- Views: 7399
- Downloads: 3411
- Keywords: aorta, guidelines, aortic diseases, diagnosis, treatment
Address for Correspondence: Fabio Massimo Oddi, Vascular Surgery Unit, University of Rome “Tor Vergata”, Italy
Email: fabio.massimo89@gmail.com ORCID: 0000-0001-8081-807X
Fabio Massimo Oddi1, Grazia Granata 1, Leonardo Oddi2, Giorgio Fedeli3, Vincenzo Brizzi4
1Vascular Surgery Unit, University of Rome “Tor Vergata”, Rome, Italy
2Saint Camillus International University of Health and Medical Sciences (UniCamillus) of Rome, Rome, Italy
3 Cardiology department, Guidonia health district, Asl Roma 5, Rome, Italy
4Department of Vascular Surgery, Tripode-Pellegrin Hospital, University Hospital of Bordeaux, Bordeaux, France
Graphical abstract
Key words: aorta, guidelines, aortic diseases, diagnosis, treatment
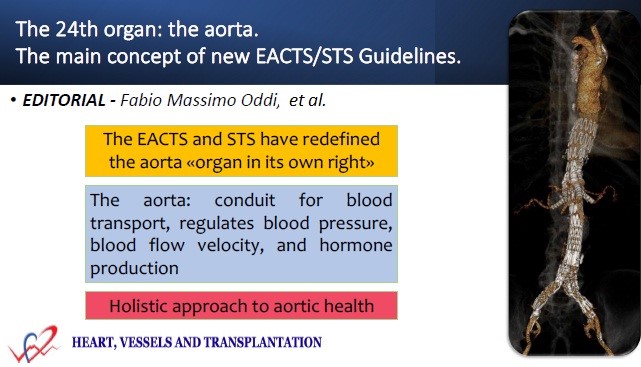
In the intricate landscape of cardiovascular medicine, the management of aortic syndromes stands as a paramount challenge, demanding precision, foresight, and expertise. The recent unveiling of the EACTS/STS Guidelines for Diagnosing and Treating Acute and Chronic Syndromes of the Aortic Organ represents a significant milestone in our journey towards enhanced patient care and outcomes, underscoring the evolving understanding of the aorta's pivotal role within the human body (1).
Aortic syndromes, ranging from acute dissections to chronic aneurysms, present unique complexities, where timely and accurate diagnosis can profoundly impact patient outcomes. Recognizing this imperative, the European Association for Cardio-Thoracic Surgery (EACTS) and the Society of Thoracic Surgeons (STS) have redefined the aorta, acknowledging it as an "organ in its own right" (1).
The aorta, traditionally viewed as a conduit for blood transport, is now understood to possess intrinsic physiological significance. It regulates blood pressure, blood flow velocity, and hormone production, underscoring its status as the 24th organ of the human body. Recognizing the aorta as an organ puts it on a par with the heart, lungs and brain. The guidelines emphasize this paradigm shift, advocating for a holistic approach to aortic health, where diagnosis, treatment, and surveillance are contextualized within the framework of organ-centric care (2).
The comprehensive scope of the guidelines encompasses both thoracic and abdominal aortic regions, offering invaluable recommendations to clinicians across various stages of patient care. From diagnostic and preoperative assessments to the selection of optimal imaging modalities and measurement techniques, these guidelines pave the way for standardized approaches in managing acute and chronic aortic diseases, including heritable thoracic aortic disease (HTAD), concepts also analyzed in the recent guidelines of the American College of Cardiology (ACC) and the American Heart Association (AHA) (3). With nearly 300 meticulously crafted recommendations, the guidelines serve as a beacon of precision and clarity, emphasizing the importance of standardized diagnostic criteria and treatment algorithms. Among these highlights, the endorsement of the TEM classification and GERAADA score for acute aortic dissection stands out, facilitating precise disease characterization and treatment planning. Furthermore, the integration of novel parameters such as aortic length into treatment decisions underscores a commitment to enhancing therapeutic precision and improving patient outcomes. (4).
Imaging modalities assume paramount importance in diagnostics, with a particular emphasis on anatomical structures like the circle of Willis, critical for planning complex surgical interventions (5). Furthermore, the guidelines establish standardized definitions for hypothermic circulatory arrest during aortic surgery, enabling uniformity in treatment strategies and outcomes assessment (6).
Treatment algorithms for acute aortic dissections, regardless of extent, are delineated, emphasizing the importance of primary tear location and malperfusion status (7). Surgical approaches for aortic arch and thoracoabdominal pathologies are detailed, alongside considerations for rare conditions and post-treatment follow-up protocols (8).
The recognition of the aorta as an organ marks a paradigm shift in medical perception, with roots tracing back to work by Raimund Erbel in 2014 (9). This transformative perspective, epitomized in the EACTS/STS Guidelines, heralds a new era of patient-centric care and collaborative innovation, underscoring the relentless pursuit of excellence in cardiovascular medicine (1).
The emergence of the new guidelines brings to the forefront a pressing question within the medical community: should the treatment of aortic diseases evolve into a separate specialized discipline? The guidelines unmistakably advocate for this transition, emphasizing the necessity of bundling aortic treatment into its own specialty, albeit in close collaboration with other medical fields. Currently, the aorta lacks a dedicated medical discipline, despite a global increase in the incidence and prevalence of aortic disease. While interest in creating specialized aortic teams has burgeoned over the past two decades, the clinical impact remains uncertain. Aortic diseases predominantly fall under the purview of cardiac or vascular surgery, yet the high mortality and morbidity rates associated with aortic surgery highlight the need for specialized expertise in this complex domain. These guidelines signal a pivotal moment for medicine and healthcare, advocating for transformative changes in medical education and specialist training to cultivate knowledgeable specialists capable of navigating the intricacies of aortic pathology and delivering optimal patient care.
Early in this century, a strong force contributing to the fragmentation of medicine was the belief that one physician could not amass all the information necessary to provide complete patient care, yet it should not be forgotten that excessive compartmentalization of medical specialties may not be ideal as it could lead to a loss of holistic understanding of the human body (10, 11).
Peer-review: Internal
Conflict of interest: None to declare
Authorship: F.M.O., G.G., L.O., G.F., and V. B. equally contributed to preparation of manuscript and fulfilled authorship criteria
Acknowledgement and funding: None to declare
References
| 1.Czerny M, Grabenwöger M, Berger T, Aboyans V, Della Corte A, et al. EACTS/STS Guidelines for diagnosing and treating acute and chronic syndromes of the aortic organ. Ann Thorac Surg 2024: S0003-4975(24)00077-8. doi: 10.1016/j.athoracsur.2024.01.021 https://doi.org/10.1016/j.athoracsur.2024.01.021 PMid:38416090 |
||||
| 2. Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J 2018; 39: 739-49 doi: 10.1093/eurheartj/ehx319. https://doi.org/10.1093/eurheartj/ehx319 PMid:29106452 |
||||
| 3.Oddi FM, Franceschini G, Oddi L, Fedeli G. 2022 American Heart Association/American College of Cardiology guidelines for the diagnosis and management of aortic disease: lessons to be drawn. Heart Vessels Transplant 2023; 7: 14-6 doi: 10.24969/hvt.2023.374 https://doi.org/10.24969/hvt.2023.374 |
||||
| 4.Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, et al; IRAD Investigators. Insights From the International Registry of Acute Aortic Dissection: A 20-Year Experience of Collaborative Clinical Research. Circulation 2018; 137: 1846-60. doi: 10.1161/CIRCULATIONAHA.117.031264 https://doi.org/10.1161/CIRCULATIONAHA.117.031264 PMid:29685932 |
||||
| 5.Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation 2003; 108: 628-35. doi: 10.1161/01 https://doi.org/10.1161/01.CIR.0000087009.16755.E4 PMid:12900496 |
||||
| 6.Preventza O, Bakaeen FG, Stephens EH, Trocciola SM, de la Cruz KI, Coselli JS. Innominate artery cannulation: an alternative to femoral or axillary cannulation for arterial inflow in proximal aortic surgery. J Thorac Cardiovasc Surg 2013; 145(3 Suppl): S191-6. doi: 10.1016/j.jtcvs.2012.11.061 https://doi.org/10.1016/j.jtcvs.2012.11.061 PMid:23260457 |
||||
| 7. Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, et al; IRAD Investigators. Role and results of surgery in acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation 2006; 114(1 Suppl): I357-64. https://doi.org/10.1161/CIRCULATIONAHA.105.000620 |
||||
| 8. Etz CD, Weigang E, Hartert M, Lonn L, Mestres CA, et al. Contemporary spinal cord protection during thoracic and thoracoabdominal aortic surgery and endovascular aortic repair: a position paper of the vascular domain of the European Association for Cardio-Thoracic Surgery. Eur J Cardiothorac Surg 2015; 47: 943-57. doi: 10.1093/ejcts/ezv142 https://doi.org/10.1093/ejcts/ezv142 PMid:25991554 |
||||
| 9. Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, et al; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014; 35: 2873-926. doi: 10.1093/eurheartj/ehu281 https://doi.org/10.1093/eurheartj/ehu281 PMid:25173340 |
||||
| 10.Grilli R, Minozzi S, Tinazzi A, Labianca R, Sheldon TA, Liberati A. Do specialists do it better? The impact of specialization on the processes and outcomes of care for cancer patients. Ann Oncol 1998; 9: 365-74. https://doi.org/10.1023/A:1008201331167 PMid:9636826 |
||||
| 11. Kavic MS. The compartmentalization of Surgery. JSLS 1997; 1: 11-2. | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

