Influence of time in therapeutic range on postoperative complications in mechanical heart valve replacement patients operated with the indigenous TTK Chitra heart valve
ORIGINAL RESEARCH ARTICLE
Influence of time in therapeutic range on postoperative complications in mechanical heart valve replacement patients operated with the indigenous TTK Chitra heart valve
Article Summary
- DOI: 10.24969/hvt.2024.482
- Page(s): 221-230
- CARDIOVASCULAR DISEASES
- Published: 28/04/2024
- Received: 01/04/2024
- Accepted: 01/04/2024
- Views: 5879
- Downloads: 3384
- Keywords: Valvular heart disease, mechanical heart valve replacement, international normalised ratio, time in therapeutic range, postoperative complications, TTK™ Chitra valve
Address for Correspondence: Tarun Shetty, Department of Cardiothoracic and Vascular Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry- 605006, India
E-mail: tscvtsjipmer@gmail.com Mobile: +91 98200 96114.
Tarun Shetty, Hemachandren M, Ram Sankar P, Durga Prasad R.
Department of Cardiothoracic and Vascular Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry- 605006, India
Abstract
Objective: Valvular heart disease (VHD) patients after mechanical heart valve (MHV) replacement surgery require postoperative prophylactic anticoagulation to preclude the risk of thromboembolic events. The aim of the present study was to understand the impact of international normalised ratio (INR) variability and time in therapeutic range (TTR) in balancing the choice of antithrombotic therapy and its outcomes in patients who underwent the MHV replacement.
Methods: This retrospective cohort study was conducted between January 2018 to December 2019 at a tertiary care hospital in South India.
Results: A total of 159 patients with a mean age of 37.31 (12) years were operated for MHV replacement. Of 159 patients, 50 patients (31.4%) were male and 109 (68.6%) were female. From the cohort, majority of the patients underwent mitral valve replacement (93, 58.5%), followed by double valve replacement (34, 21.4%) and aortic valve replacement (32, 20.1%). Post-surgery, 36 patients had thromboembolic complications, where the majority suffered from peripheral embolism (18, 50%), followed by ischemic stroke (10, 27.7%), and prosthetic valve thrombosis (8, 22.2%). The most common post-operative anti-coagulation drug used was warfarin (124, 79%). The INR range of 2.01 – 2.49 (p - 0.003) was reported to be significant for mitral valve and double valve replacement patients.
Conclusion: Overall, the complication rates in the Indian population who underwent MHV replacement was reported to be low. To conclude, higher the TTR - lesser will be the risk of developing complications and vice versa.
Key words: Valvular heart disease, mechanical heart valve replacement, international normalised ratio, time in therapeutic range, postoperative complications, TTK™ Chitra valve.
Introduction
The prevalence of valvular heart disease (VHD) is rising worldwide, affecting approximately 41 million people (1). In future too, it is expected to rise year-on-year concurrently with increase in life expectancy. Among all the heart valve-related pathologies, rheumatic heart disease (RHD) is more prevalent and reported predominantly in low-income and middle-income countries (2). It is estimated that approximately 300 000 new prostheses are implanted annually worldwide (3). Such heart valve replacement surgeries were performed using either mechanical or bioprosthetic valves depending upon the individual medical and other considerations such as age, desires, lifestyle, values, surgical factors, co-morbidities, and clinical conditions (4).
Both mechanical and bioprosthetic valves have their own advantages and disadvantages. However, limitations such as durability and structural valve deterioration discouraged the use of bioprosthetic valves. Except for the risk of thromboembolism, mechanical valves were considered to be more durable and effective. To avoid any post-operative mechanical heart valve (MHV) replacement-related complications, all the operated patients are now encouraged to use lifelong anticoagulation drugs and vitamin K antagonists such as warfarin.
Graphical abstract
In clinical practice, European therapeutic guidelines or the American College of Cardiology/ American Heart Association/ American College of Chest Physicians (AHA/ACC/ACCP) have provided certain recommendations regarding the use of anticoagulants and target international normalized ratio (INR) range for the timeous adjustment of anticoagulants dosages, to avoid INR out of the safe range related thrombosis and bleeding complications (5). Such anticoagulation effects by anticoagulants were thoroughly measured using either the traditional/or Rosendall method, to determine the target INR and time in the therapeutic range (TTR, anticoagulation effectiveness). The traditional method is the percentage of values in the therapeutic range. For mitral valve replacement (MVR) and double valve replacement (DVR) patients, target INR was considered a 2.5 – 3.5 and for aortic valve replacement (AVR) patients it was considered as 2.0 – 3.0. The Rosendall method, known as the percentage of days in the therapeutic range, considers the amount of time between the visits and estimates the number of days the patient's INR was in the therapeutic range. The Rosendall method uses linear interpolation to assign an INR value to each day between successive observed INR values (6). Establishing such optimum INR was reported to avoid a large number of post-operative complications. The optimal INR range was always a debate and it was also reported to be highly dependent up on race and ethnicity of the patients. Randomised clinical trials conducted in Asian population have always confirmed the greater tendency of bleeding to anticoagulation therapy over Western population (5). From the literature, the overestimation of such TTR values and its outcomes were well documented from different parts of the world. In view of this, balancing INR and TTR was reportedly taken a central role in patient`s post-operative outcomes.
In the present study, we tried to study and understand the impact of INR variability and TTR in balancing the choice of antithrombotic therapy and its outcomes in patients who have underwent MHV replacement.
Methods
Study design and population
This retrospective cohort study was conducted over a period of two years (January 2018 to December 2019) at a tertiary care hospital in South India. All the patients were operated for MHV replacement (single or double) were rigorously followed up.
Only patients with a minimum of 15 INR reports were included in the final study data.
Whereas, patients with a history of MVR, AVR or DVR with coronary artery bypass graft surgery (CABG) were excluded. Patients with co-morbidities associated with liver/kidney disease
/coagulopathies were also discouraged from participating in the study.
Written informed consent was obtained from the participants for all procedures. Ethics committee approval was received for this study from the Institutional Ethics Committee for Observational Studies, JIPMER, India (JIP/IEC/2021/031).
Baseline variables
All the required final data was collected from electronic medical records and operation theatre registries of the hospital. The demographic (age, sex), history of atrial fibrillation, comorbidities, surgery and their types, transcatheter interventions, valve lesions and anticoagulation therapy were retrieved.
Outcome variables
Post-surgery, all the patients were contacted and enquired through telephone or email regarding any postoperative complications. Major thromboembolic events such as cerebral infarction, peripheral embolism, and valve thrombosis were considered and recorded. Cerebral infarction is defined as a sudden temporary or permanent neurologic defect. Whereas, hemorrhagic episodes include fatal bleeding, intracranial bleeding, or any bleeding requiring a blood transfusion, and hospitalization. Any events that occurred during an episode of endocarditis were excluded. We also documented survival of patients. Whereas, INR values measured at the time of the event or within the last seven days of the event were included and documented.
TTR Calculation
Generally, TTR was calculated either by traditional method or Rosendall method or both. The traditional method is the percentage of values in the therapeutic range. Whereas, the Rosendall method, known as the percentage of days in the therapeutic range by using a linear interpolation approach. In the present study, we have used the traditional method for calculation of TTR.

Statistical analysis
Based on the normality of the data, the continuous variables like age, follow-up period, total INR values, TTR, INR range, and INR at the time of the event were summarized as mean with standard deviation (SD)/or median with interquartile range (IQR). Whereas the categorical variables such as sex, diagnosis, atrial fibrillation, past history, and comorbidities were summarized as frequency/or proportion. The comparison of variables between groups was performed using the Mann-Whitney U test and the Chi-Square test. A p-value < 0.05 was considered significant. Throughout the study, a standard pro forma was used for data collection, tabulation (Microsoft Office 2021, Microsoft Corporation, Albuquerque, NM, USA), and analysis (SPSS Version 22, Chicago, IL, USA).
Results
A total of 159 patients were operated for MHV replacement. The mean age of the patients was 37.31 (12) years (Table 1) with female predominance (109, 68.6%). Of 159 patients, 119 (74.8%) had no history of surgery and predominant of them underwent MVR (93, 58.5%), followed by DVR (34, 21.4%) and AVR (32, 20.1%). The most common post-operative complication was reported to be thromboembolic events (36, 22.6%). Out of 159 patients, 143 were alive, 14 had expired, and 2 were lost to follow-up.
The major post-operative anti-coagulant used was warfarin (124, 79%), followed by warfarin-acetylsalicylic acid (24, 15.3%) and acitrom (9, 5.7%).
The surgical baseline characteristics, INR, and TTR grouping of all the patients are reported in Tables 2-5. ![]()
|
Table 1. Clinical characteristics |
|
|
Variables |
N=159 |
|
Age distribution, years |
37.3 (12.0) |
|
Sex distribution, n(%) |
|
|
Male |
50 (31.4) |
|
Female |
109 (68.6) |
|
Atrial fibrillation, n(%) |
|
|
Yes |
63 (39.6) |
|
No |
96 (60.4) |
|
History of past surgery, n(%) |
|
|
No surgery |
119 (74.8) |
|
Yes |
3* (1.9) |
|
Balloon mitral valvotomy |
24 (15.1) |
|
Trans-ventricular mitral commissurotomy |
11 (6.9) |
|
Balloon aortic valvotomy |
2 (1.3) |
|
Surgery done, n(%) |
|
|
Aortic valve replacement |
32 (20.1) |
|
Double valve replacement |
34 (21.4) |
|
Mitral valve replacement |
93 (58.5) |
|
Complications, n(%) |
|
|
No complication |
116 (73) |
|
Bleeding complication |
7 (4.4) |
|
Thrombotic complications, n(%) |
36 (22.6) |
|
Peripheral embolism |
18 (50) |
|
Ischaemic stroke |
10 (28) |
|
Prosthetic valve thrombosis |
8 (22) |
|
Anticoagulation used, n(%) |
|
|
Warfarin |
124 (79) |
|
Warfarin- acetylsalicylic acid |
24 (15.3) |
|
Acitrom |
9 (5.7) |
|
Survival, n(%) |
|
|
Alive |
143 (91) |
|
Expired |
14 (9) |
|
Not known |
2 |
|
*exact detail of the surgical procedure not known Data are presented as mean (SD) and number (percentage) |
|
As can be seen from Table 2, patients who underwent AVR were older than patients in MVR and DVR groups, and female sex dominated in MVR and DVR groups. Atrial fibrillation was present only in MVR and DVR groups, due to mitral valve disease. History of balloon valvotomy and transventricular mitral comissurotomy was higher in MVR group. MVR group tended to have less complications, while AVR group has higher thrombotic complications and DVR – bleeding complications. Groups did not differ by type of anticoagulation therapy. Survival did not differ between groups.
As to valve lesions (Table 3), in AVR group severe calcific aortic stenosis and aortic regurgitation prevailed, while in MVR group severe mitral stenosis due to rheumatic heart disease was the most encountered lesion and in DVR group – severe aortic stenosis and severe mitral stenosis and severe mitral stenosis and severe aortic regurgitation bot due to rheumatic heart disease were documented in 1/5 of patients each.
|
Table 2. Surgical group- wise baseline characteristics |
|||
|
Baseline characteristics N=159 |
AVR |
DVR |
MVR |
|
(n=32) |
(n=34) |
(n=93) |
|
|
Age, years |
41.1 (12.4) |
35.5 (12.6) |
36.6 (11.4) |
|
Sex, n(%) |
|
|
|
|
Male |
20 (62.5) |
14 (41.2) |
16 (17.2) |
|
Female |
12 (37.5) |
20 (58.8) |
77 (82.8) |
|
Atrial fibrillation n(%) |
|
|
|
|
Yes |
0 |
17 (50) |
46 (49.5) |
|
No |
32 (100) |
17 (50) |
47 (50.5) |
|
Past surgery, n(%) |
|
|
|
|
No surgery |
32 (100) |
29 (85.3) |
58 (62.4) |
|
Yes |
- |
0 |
3 (3.2) |
|
BMV |
- |
3 (8.8) |
21 (22.6) |
|
TVMC |
- |
0 |
11 (11.8) |
|
BAV |
- |
2 (5.9) |
0 |
|
Complications, n(%) |
|
|
|
|
No Complication |
22(68.8) |
23(67.7) |
71(76.3) |
|
Bleeding Complication |
1(3.1) |
3(8.8 ) |
3(3.2) |
|
Thrombotic Complication |
9(28.1) |
8(23.5) |
19(20.4) |
|
Anticoagulation used, n(%) |
|
|
|
|
Warfarin |
24(75) |
28(82.3) |
72(79.1) |
|
Warfarin-ASA |
7(21.9) |
3(8.8) |
14(15.4) |
|
Acitrom |
1(3.1) |
3(8.8) |
5(5.5) |
|
Survival, n(%) |
|
|
|
|
Alive |
28(93.3) |
31(91.2) |
84(90.3) |
|
Expired |
2(6.7) |
3(8.0) |
9(9.7) |
|
Data are presented as mean (SD) and number (percentage) ASA - acetylsalicylic acid, BAV - balloon aortic valvotomy, BMV - balloon mitral valvotomy, TVMC - trans-ventricular mitral commissurotomy |
|||
The time spent according to INR range are displayed in Table 4. The time in suboptimal INR less 2.0 for AVR, MVR and DVR was found as 22.5 and 7.6 median, while in 2-2.5 and 3.5-4.5 – 20.5 and 11.5 respectively. Mean TTR was 30.8%
The TTR and INR ranges for each groups of surgery – AVR, MVR and DVR are presented in Table 5.
The TTR for AVR group was 39%, DVR – 31.5% and MVR – 27%.
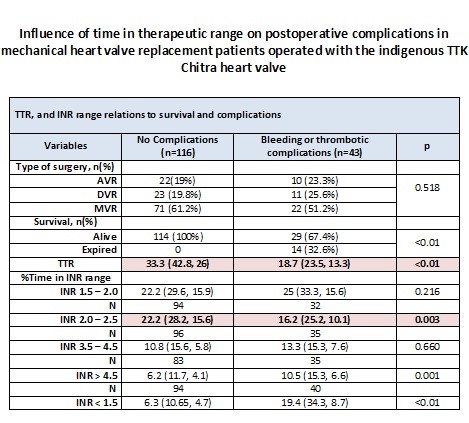
Comparison between groups with and without complications are presented in Table 6.
There were no differences between groups with and without complications regarding age, sex, history of atrial fibrillation, history of surgery and type of surgery (p>0.05).
There were significant differences in survival status with mortality of 32% in complications group vs no mortality in group without complications (p<0.01). Among those 43 patients reported with complications, 29 (67.4%) were alive and 14 (32.6%) were succumbed to death. Of the 14 patients dead, 6 patients died following thromboembolic events, 5 of bleeding complications, 2 were unrelated to surgery, and 1 patient’s cause of death could not be identified.
The INR values at the time of the complications of all the patients were assessed and it was reported that they all had a low TTR (< 25%) (p<0.01).
Among the INR ranges, the overall complication rates were reportedly low in the INR range of 2.01 – 2.49 (p=0.003). Whereas, increase in complication rates were reported in INR values >4.5 (p=0.001) and <1.5 (p<0.01).
Overall, 422 patient-years were retrospectively studied and 3919 INR values were reviewed with a mean follow-up period of 2.65±1.5 years, and mean INR values of 24.65±6.9 for each patient.
|
Table 3. Surgical groups-wise valve lesions (n=159) |
|||||
|
AVR |
DVR |
MVR |
|||
|
(n=32) |
(n=34) |
(n=93) |
|||
|
Diagnosis |
Number (%) |
Diagnosis |
Number (%) |
Diagnosis |
Number (%) |
|
BAV Sev CalcificAS |
1 (3.1) |
IE MV AV |
2 (5.9) |
RHD SevMR |
7 (7.5) |
|
BAV SevAR |
2 (6.3) |
RHD ModMS SevAR |
1 (2.9) |
RHD SevMR SevAR |
4 (4.3) |
|
RHD SevAR |
2 (6.3) |
RHD ModMS SevAS |
2 (5.9) |
RHD SevMS |
76 (81.7) |
|
Sev CalcificAS |
11 (34.4) |
RHD SevAS ModMS |
1 (2.9) |
RHD SevMS ModAR |
2 (2.2) |
|
Sev CalcificAS BAV |
1 (3.1) |
RHD SevMR ModAR |
3 (8.8) |
RHD SevMS SevMR |
3 (3.2) |
|
SevAR |
8 (25) |
RHD SevMR ModAS |
1 (2.9) |
SevMR |
1 (1.1) |
|
SevAR IE |
1 (3.1) |
RHD SevMR SevAR |
3 (8.8) |
- |
- |
|
SevAR Takayasu arteritis |
1 (3.1) |
RHD SevMR SevAS |
1 (2.9) |
- |
- |
|
SevAS |
5 (15.6) |
RHD SevMS ModAR |
5 (14.7) |
- |
- |
|
SevAR IE |
1 (3.1) |
RHD SevMR SevAR |
3 (8.8) |
- |
- |
|
- |
- |
RHD SevMS SevAR |
7 (20.6) |
- |
- |
|
- |
- |
RHD SevMS SevAS |
7 (20.6) |
- |
- |
|
AR - aortic regurgitation, AS - aortic stenosis, AV - aortic valvotomy, AVR - aortic valve replacement, BAV - bicuspid aortic valve, DVR - double valve replacement, IE - Infective endocarditis, MR - mitral regurgitation, MS - mitral stenosis, MV - mitral valvotomy, MVR - mitral valve replacement, Mod – moderate, RHD - rheumatic heart disease, Sev – severe |
|||||
|
Table 4. Time spent in different INR ranges by AVR, MVR, and DVR patients |
||||
|
INR Group |
N=159 |
Mean (Standard Deviation) |
Median |
Inter quartile Range |
|
Time Therapeutic Range |
159 |
30.8 (13.4) |
29.1 |
(39.3, 22.2) |
|
INR 1.5 - 2.0 |
159 |
23.2 (10.2) |
22.5 |
(29.4, 15.7) |
|
INR 2.0 – 2.5 |
126 |
20.9 ( 8.3) |
20.5 |
(27.7, 14) |
|
INR 3.5 – 4.5 |
159 |
12.4 (6.6) |
11.5 |
(15.6, 5.04) |
|
INR > 4.5 |
159 |
8.9 (5.7) |
7.2 |
(12.58, 4.5) |
|
INR < 1.5 |
159 |
13.8 (13.9) |
7.6 |
(15.9, 5.0) |
|
AVR - aortic valve replacement, DVR - double valve replacement, INR - international normalized ratio, MVR - mitral valve replacement, TTR - time therapeutic range
|
||||
|
Table 5. TTR and different INR ranges for the three surgical groups (AVR, MVR, and DVR) |
|||
|
Variables |
AVR |
DVR |
MVR |
|
Time Therapeutic Range* |
39.3 (54.13, 22.98) |
31.5 (36.83, 19) |
27 (35.2, 21.8) |
|
N |
32 |
34 |
93 |
|
INR 1.5 – 2.0 |
23.4 (33.3, 17.7) |
23 (26.9, 15.7) |
22.2 (29.7, 15.35) |
|
N |
|
33 |
93 |
|
INR 2.0 – 2.5 |
- |
21 (29.4, 14.5) |
20.5 (27.35, 13.8) |
|
N |
25 |
23 |
83 |
|
INR 3.5 – 4.5 |
20 (23.95, 13.6) |
9.5 (13.3, 5.8) |
9.6 (14.2, 5.8) |
|
N |
20 |
28 |
70 |
|
INR < 4.5 |
6.6 (7.4, 4.7) |
9.75 (13.83, 4.3) |
7.95 (12.93, 4.55) |
|
N |
25 |
27 |
82 |
|
INR > 1.5 |
10 (33.95, 5.4) |
6.6 (21, 4.7) |
7.5 (13, 5) |
|
Data are presented as median (IQR) INR - International Normalized Ratio; TTR - Time Therapeutic Range; MVR - Mitral valve replacement; DVR - Double valve replacement; AVR - Aortic valve replacement. *The INR values collected in the follow up period have been systematically arranged separately for AVR, MVR, and DVR patients. These values have been further segregated into different INR ranges, where TTR represents the established INR range i.e. 2.0 – 3.0 for AVR patients and 2.5 – 3.5 for MVR and DVR patients. The range 2.01 – 2.49 will be available only for MVR and DVR patients, as in the AVR patients the TTR is taken as INR 2.0 – 3.0. Therefore, in AVR patients, there will be no entry in the 2.01 – 2.49 range column. Remaining all ranges are common for all the three groups.
|
|||
Discussion
In resource-limited settings like India, MHV replacement is associated with high costs which results in lower reach to the people. In view of such limitations, in the early 1900s an indigenous prosthetic heart valve (The TTK Chitra™) was developed by the Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum. Since then, it was largely tested and curated as per international protocols applicable for the development and use of critical bio-medical devices.
In the present study cohort, TTK Chitra™ was used in all the patients and majority were females with mitral valve disease. Review studies conducted by Youssef et al. (7) and Desjardin JT et al.(8) also confirmed the higher prevalence rate of mitral valve (especially rheumatic heart disease) lesions in women across all age groups over men with a predominance rate of 3:1. On the other hand, men were reported to have higher incidences of aortic valve diseases (aortic regurgitation) (9). Major post-operative complications in these MHV replacement patients include bleeding and thromboembolic events such as valve thrombosis, cerebral infarction, and peripheral embolism.
As reported by multiple studies, the Asian population has a higher propensity for bleeding during anticoagulation therapy than the Western population (5). Therefore, before mechanically applying the ‘one-size-fits-all’ strategy as per current Western-oriented US and European guidelines, focusing on optimal treatment strategy depending on the patient’s race and medical condition can be highly beneficial in terms of decreasing complication rate and increasing survival rate (10,11).
In view of this, in the present study, an optimal, lower INR range was explored for efficacious anticoagulation without increasing the risk of thrombosis. Where an efficient therapeutic INR range was reported to be 2 - 3 in AVR patients and 2.5 - 3.5 for MVR and DVR patients (12). Among all the anti-coagulants used post-operatively, warfarin (a vitamin K antagonist) was reported to have significant effect in reducing the thromboembolic side effects and bleeding. From the earlier studies, labile INR was defined as TTR < 60% (6,13).
![]()
|
Table 6. Comparison between gender, age, atrial fibrillation, surgical history, type of surgery, survival status, TTR, INR range, and complications
|
|||
|
Variables |
No Complications (N=116) |
Bleeding or thrombotic complications (N=43) |
p |
|
Gender, n(%) |
|
|
|
|
Male |
40 (34.5%) |
10 (23.3%) |
0.176
|
|
Female |
76 (65.5%) |
33 (76.7%) |
|
|
Age, years |
37 (42, 30) |
39 (45, 32) |
0.455 |
|
Atrial fibrillation |
|
|
|
|
Yes |
41 (35.3%) |
22 (51.2%) |
0.070
|
|
No |
75 (64.7%) |
21 (48.8%) |
|
|
Surgical history, n(%) |
|
|
|
|
No surgery |
83 (71.6%) |
36 (83.7%) |
0.339
|
|
Yes |
3 (2.6%) |
0 |
|
|
BMV |
19 (16.4%) |
5 (11.6%) |
|
|
TVMC |
10 (8.6%) |
1 (2.3%) |
|
|
BAV |
1 (0.9%) |
1 (2.3%) |
|
|
Type of surgery, n(%) |
|
|
|
|
AVR |
22(19%) |
10 (23.3%) |
0.518
|
|
DVR |
23 (19.8%) |
11 (25.6%) |
|
|
MVR |
71 (61.2%) |
22 (51.2%) |
|
|
Survival, n(%) |
|
|
|
|
Alive |
114 (100%) |
29 (67.4%) |
<0.01 |
|
Expired |
0 |
14 (32.6%) |
|
|
TTR |
33.3 (42.8, 26) |
18.7 (23.5, 13.3) |
<0.01 |
|
%Time in INR range |
|
|
|
|
INR 1.5 – 2.0 |
22.2 (29.6, 15.9) |
25 (33.3, 15.6) |
0.216 |
|
N |
94 |
32 |
|
|
INR 2.0 – 2.5 |
22.2 (28.2, 15.6) |
16.2 (25.2, 10.1) |
0.003 |
|
N |
96 |
35 |
|
|
INR 3.5 – 4.5 |
10.8 (15.6, 5.8) |
13.3 (15.3, 7.6) |
0.660 |
|
N |
83 |
35 |
|
|
INR > 4.5 |
6.2 (11.7, 4.1) |
10.5 (15.3, 6.6) |
0.001 |
|
N |
94 |
40 |
|
|
INR < 1.5 |
6.3 (10.65, 4.7) |
19.4 (34.3, 8.7) |
<0.01 |
|
AVR - aortic valve replacement, BAV - balloon aortic valvotomy, BMV - balloon mitral valvotomy, DVR - double valve replacement, INR - international normalized ratio, , MVR - mitral valve replacement, TTR - time in therapeutic range, TVMC - trans-ventricular mitral commissurotomy
|
|||
However, multiple studies have reported a wide TTR range varying from ∽25% to 65%, depending upon the patients’ geographical region, and physician specialty (14–16). The studies are in favour of higher TTR for better outcomes. The mean TTR in the present study was reportedly very low (29.1%, IQR: 22.2 – 39.3) with higher complication rate of 22.6%, thus validating the fact of low TTR and its association with higher complication rates.
In MVR and DVR patients, complications have occurred mainly outside the INR range of 2.0-3.5. Whereas, fewer complications were noted in the INR range group of 2.0 – 2.5 and 2.5 – 3.5, which were statistically significant.
Studies have also reported less vulnerability of Asian patients to thromboembolic events with a greater tendency to bleed during anticoagulation therapy than Western patients. In view of this, patients from Asian countries are always recommended a lower therapeutic INR range. However, in contrast to this, our study has shown a higher thromboembolic complication rate occurrence outside the INR range of 2.0-3.5.
In Asian countries, especially in populous countries like India, rheumatic heart disease is considered as a neglected disease of poverty and it is also seen very high globally in disadvantaged population (17, 18). As the majority of our patients are from the lower socioeconomic strata of society, the literacy rate, awareness level, and limited access to INR testing have formed natural confining barriers. This in turn reflected in the patient’s non-compliance with medication, suggested dietary modifications, and regular follow-ups leading to poorer INR control and low TTR. As per the RE-LY AF registry maintained worldwide, the TTR for patients from India, China, and Africa were reported to be <40% (19,20). Therefore, to improve the clinical outcomes using oral anticoagulants in patients from lower-middle-income countries (i.e. India) - recruitment of educated and motivated individuals from the local communities as surrogate healthcare providers to perform home monitoring can be a novel and practical approach.
Study limitations
The present study findings might have been influenced by several limitations. Such limitations include its single-centre, retrospective, and non-randomized nature with a limited-sized cohort. Non-validation of concomitant medications and their interference with anti-coagulant drugs. The use of the traditional method over the Rosendall method in TTR calculation. Data gaps in the long-term follow-up due to the pandemic are prone to bias due to telephonic follow-ups too. Despite these limitations, the current study provides some valuable insights.
Conclusion
From our study, we conclude TTR as a highly dependent factor in developing MHV post-operative complications. TTR usage cannot be generalised, as it is largely varied and highly dependent on the patient’s geographical location. Therefore, the guidelines advised by the AHA/ACC/ACCP may not be relevant and may not be suitable to extrapolate data from Western patients to the Asian population. Overall, the complications rate in the Indian population who underwent MHV (Mitral and Double valve Replacement) replacement was reported to be low in between the therapeutic INR range of 2.01 – 2.50 with efficacious anticoagulation without any increased risk of thrombosis.
Ethics: Ethics committee approval was received for this study from the Institutional Ethics Committee for Observational Studies, JIPMER, India (JIP/IEC/2021/031). Informed consent of the procedure was obtained from all patients.
Written informed consent was obtained from the participants.
Peer-review: External and internal
Conflict of interest: All other authors declare no competing interests.
Authorship: Concept - T.S., D.P.R., H.M., R.S.N.; Design - T.S., D.P.R., H.M., R.S.N.; Supervision - T.S., D.P.R., H.M., R.S.N.; Materials - T.S., D.P.R., H.M., R.S.N.; Data Collection and/or Processing - T.S., D.P.R., H.M., R.S.N.; Analysis and/or Interpretation - T.S., D.P.R., H.M., R.S.N.; Literature Search - T.S.; Writing Manuscript – T.S.; Critical Review – D.P.R., H.M., R.S.N.
Acknowledgements: The authors would like to thank Phoenix Publishing House Group, India, for their medical writing assistance.
Funding: None to declare
Availability of data and materials: The data analyzed during the current study are not publicly available. They are available from the corresponding author on reasonable request.
References
| 1. Coffey S, Roberts-Thomson R, Brown A, Carapetis J, Chen M, Enriquez-Sarano M, et al. Global epidemiology of valvular heart disease. Nat Rev Cardiol 2021 1812 2021; 18: 853-64. https://doi.org/10.1038/s41569-021-00570-z PMid:34172950 |
||||
| 2. Aluru JS, Barsouk AA, Saginala K, Rawia P, Basouk A, et al. Valvular heart disease epidemiology. 2022; 10: 32. https://doi.org/10.3390/medsci10020032 PMid:35736352 PMCid:PMC9228968 |
||||
| 3. Havers-Borgersen E, Butt JH, Vinding NE, Top-Pedersen Ch, Gislason G, Kober L, et al. Time in therapeutic range and risk of thromboembolism and bleeding in patients with a mechanical heart valve prosthesis. J Thorac Cardiovasc Surg 2019; 159: 74-83.e4. https://doi.org/10.1016/j.jtcvs.2019.02.061 PMid:30961980 |
||||
| 4. Tillquist MN, Maddox TM. Cardiac crossroads: deciding between mechanical or bioprosthetic heart valve replacement. Patient Prefer Adherence 2011; 5: 91. https://doi.org/10.2147/PPA.S16420 PMid:21448466 PMCid:PMC3063655 |
||||
| 5. Ntlokotsi S, Moshesh M, Mntla P, Towobola OA, Mogale MA. Optimum INR intensity and therapeutic INR control in patients with mechanical heart valve prosthesis on warfarin oral anticoagulation at Dr George Mukhari academic hospital: a three-year retrospective study. South African Fam Pract 2019; 60: 192-6. https://doi.org/10.1080/20786190.2018.1467182 |
||||
| 6. Tan CSY, Fong AYY, Jong YH, Ong TK. INR control of patients with mechanical heart valve on long-term warfarin therapy. Glob Heart 2018; 13: 241-4. https://doi.org/10.1016/j.gheart.2018.08.003 PMid:30213574 |
||||
| 7. Youssef G. Valvular heart diseases in women. Egypt Hear J 2021; 73: 58. DOI: 10.1186/S43044-021-00184-3. https://doi.org/10.1186/s43044-021-00184-3 PMid:34176027 PMCid:PMC8236007 |
||||
| 8. DesJardin JT, Chikwe J, Hahn RT, Hung JW, Delling FN. Sex differences and similarities in valvular heart disease. Circ Res 2022; 130: 455-73. https://doi.org/10.1161/CIRCRESAHA.121.319914 PMid:35175844 PMCid:PMC8869851 |
||||
| 9.Kong WKF, Regeer MV, Ng ACT, McCormack LM, Poh KK, Yeo TC, et al. Sex differences in phenotypes of bicuspid aortic valve and aortopathy: insights from a large multicenter, international registry. Circ Cardiovasc Imaging 2017; 10: e005155. DOI: 10.1161/CIRCIMAGING.116.005155. https://doi.org/10.1161/CIRCIMAGING.116.005155 PMid:28251911 |
||||
| 10. Cho H, Kang J, Kim HS, Park KW. Ethnic differences in oral antithrombotic therapy. Korean Circ J 2020; 50: 645-7. https://doi.org/10.4070/kcj.2020.0098 PMid:32725974 PMCid:PMC7390713 |
||||
| 11. Guo YT, Zhang Y, Shi XM, Shan ZL, Wang CJ, Wang YT, et al. Assessing bleeding risk in 4824 Asian patients with atrial fibrillation: The Beijing PLA Hospital Atrial Fibrillation Project. Sci Rep 2016; 6: 31755 DOI: 10.1038/SREP31755. https://doi.org/10.1038/srep31755 PMid:27557876 PMCid:PMC4997334 |
||||
| 12. Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021; 77: 450-500. https://doi.org/10.1016/j.jacc.2020.11.035 PMid:33342587 |
||||
| 13. Grzymala-Lubanski B, Labaf A, Englund E, Swenson PJ, Sjalander A. Mechanical heart valve prosthesis and warfarin - Treatment quality and prognosis. Thromb Res 2014; 133: 795-8. https://doi.org/10.1016/j.thromres.2014.02.031 PMid:24642005 |
||||
| 14.Reiffel JA. Time in the Therapeutic Range (TTR): An overly simplified conundrum. J Innov Card Rhythm Manag 2017; 8: 2643. https://doi.org/10.19102/icrm.2017.080302 PMid:32494441 PMCid:PMC7252837 |
||||
| 15. Pokorney SD, Simon DN, Thomas L, Fonarow GC, Kowey PR, Chang P, et al. Patients' time in therapeutic range on warfarin among US patients with atrial fibrillation: Results from ORBIT-AF registry. Am Heart J 2015; 170: 141-8. https://doi.org/10.1016/j.ahj.2015.03.017 PMid:26093875 |
||||
| 16. Baker WL, Cios DA, Sander SD, Coleman CI. Meta-analysis to assess the quality of warfarin control in atrial fibrillation patients in the United States. J Manag Care Pharm 2009; 15: 244-52. https://doi.org/10.18553/jmcp.2009.15.3.244 PMid:19326955 PMCid:PMC10437339 |
||||
| 17. Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: A systematic review. PLoS Negl Trop Dis 2018. DOI: 10.1371/JOURNAL.PNTD.0006577. https://doi.org/10.1371/journal.pntd.0006577 PMid:29897915 PMCid:PMC6016946 |
||||
| 18. Shawar YR, Shiffman J. Generating global priority for addressing rheumatic heart disease: A qualitative policy analysis. J Am Heart Assoc; 2020. DOI: 10.1161/JAHA.119.014800. https://doi.org/10.1161/JAHA.119.014800 PMid:32308101 PMCid:PMC7428514 |
||||
| 19. Zühlke L, Karthikeyan G, Engel ME, Rangarajan S, Mackie P, Mauff BCK, et al. Clinical outcomes in 3343 children and adults with rheumatic heart disease from 14 low-and middle-income countries: two-year follow-up of the global rheumatic heart disease registry (the remedy study). Circulation 2016; 134: 1456-66. https://doi.org/10.1161/CIRCULATIONAHA.116.024769 PMid:27702773 |
||||
| 20.Oldgren J, Healey JS, Ezekowitz M, Commerford P, Avezum A, Pais P, et al. Variations in cause and management of atrial fibrillation in a prospective registry of 15 400 emergency department patients in 46 countries. Circulation 2014; 129: 1568-76. https://doi.org/10.1161/CIRCULATIONAHA.113.005451 PMid:24463370 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

