Minimally-invasive valve surgery in patients with valvular heart disease with comorbidities: A single centre experience
ORIGINAL RESEARCH ARTICLE
Minimally-invasive valve surgery in patients with valvular heart disease with comorbidities: A single centre experience
Article Summary
- DOI: 10.24969/hvt.2024.494
- CARDIOVASCULAR DISEASES
- Published: 30/06/2024
- Received: 08/02/2024
- Revised: 20/05/2024
- Accepted: 22/05/2024
- Views: 4865
- Downloads: 3144
- Keywords: minimal invasive valve surgery, pulmonary arterial hypertension, chronic obstructive pulmonary disease, right anterolateral mini thoracotomy
Address for Correspondence: Ketav Lakhia, U N Mehta Institute of Cardiology and Research Centre, Ahmedabad, Gujarat, India E-mail: ketavtl@gmail.com
Milan Snehkunj1a, Ketav Lakhia1a, Ronak Khojani1a, Himani Pandya1b, Chirag Doshi1a
1aDepartment of Cardiovascular and Thoracic Surgery and 1bDepartment of Research, U. N. Mehta Institute of Cardiology and Research Centre, (Affiliated to B. J. Medical College), New Civil Hospital Campus, Asarwa, Ahmedabad-380006, India
Abstract
Objective: With advancements in technology, instrumentation and techniques in minimally invasive surgery, several new findings have arisen about patients undergoing minimally invasive cardiac valve surgery (MICVS). This study focuses on assessing the safety and effectiveness of MICVS in a particular population, characterized by advanced age, multiple comorbidities and a high-risk profile for conventional open-heart surgery amid scepticism and resistance over minimally invasive cardiac surgery.
Methods: This is a descriptive retrospective study. The patients with valvular heart disease having multiple co-morbidities (e.g. left ventricular dysfunction (LVD), elderly, severe pulmonary arterial hypertension (PAH), chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), obesity, redo surgery etc.) who underwent MICVS between August 2018 to December 2021 at our tertiary cardiac care Institute (UNMICRC)(n=100) were included. Overall, 77 patients underwent minimally invasive mitral/tricuspid valve interventions through right anterolateral mini thoracotomy and 23 patients underwent minimally invasive aortic valve intervention. Various outcomes in terms of patient demographics, intraoperative findings, perioperative data, hospital length of stay, complications were observed and analyzed.
Results: Out of 100 patients, 47 were male & 53 were female. The mean age was 43.26 (12.80) years; 13 had infective endocarditis, 11 had previous cardiac intervention, 11 had COPD, 4 had previous history of stroke, 64 patients were diabetic having HbA1C > 7%, 22 patients had severe PAH, 16 - LVD. Nine patients had CKD, among them two patients were on hemodialysis. Average mechanical ventilation time was 9.6 (6.67) hours, average hospital stay was 4.85 (1.05) days and average ICU stay was 56.4 (13.37) hours.
Conclusion: In comparison to conventional methods, MICVS appears to have more promising results for this specific patient group, such as fewer postoperative complications, shorter mechanical ventilation time, shorter hospital & ICU stay and a tendency towards quicker recovery. The study highlights the significance of careful patient selection and surgeon experience, as well as the difficulties and complexities of applying MICVS in this specific patient group.
Graphical abstract
Key words: Minimal invasive valve surgery, pulmonary arterial hypertension, chronic obstructive pulmonary disease, right anterolateral mini thoracotomy
Introduction
Over the past ten years, there has been a rise in the use of minimally invasive, or less invasive, techniques for heart valve surgery. Early investigations in patients with lower risk showed the method was associated with improved recovery, higher patient satisfaction, and good operating results due to its less traumatic nature (1).
Over the time, surgeons used this strategy to treat patients with more comorbidities and performed more complex surgeries, despite a steep learning curve. Heart valve surgery that is minimally invasive is a relatively new and noteworthy paradigm shift. Initially, traditionalists opposed these methods, saying that smaller incisions result in less exposure and inferior results.
The last ten years have seen tremendous advancement and improvement in procedures, which has led to the understanding that complicated valve surgery may be successfully conducted using a minimally-invasive approach. Minimally invasive cardiac valve surgery (MICVS) is therefore being used more often as a standard procedure in several institutions around the globe, with outstanding short-term and long-term outcomes. Only after becoming skilled in performing the conventional operations, all MIVS are undertaken.
This study’s objective is to evaluate the effects of MICVS in patients with co-morbidities on postoperative complications, respiratory issues, hospital length of stay (LOS), and returning to routine activities.
Methods
Study design and population
This was a descriptive retrospective study conducted for a duration of 3 years from August 2018 to December 2021 at our tertiary cardiac care centre, in Ahmedabad. A total of 100 patient’s data were collected. The study was conducted after Institutional ethical committee clearance (UNMICRC/CVTS/2019/18). Informed consent was taken from all the patients.
In this study, the patients with valvular heart disease having multiple co-morbidities (e.g. left ventricular dysfunction (LVD), elderly, with severe pulmonary arterial hypertension (PAH), chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), obesity, redo surgery etc.) undergoing MICVS (n=100) were included. Patients with COPD (long-term use of bronchodilators or steroids), PAH (pulmonary artery systolic pressure >31mmHg), patients with left ventricular systolic dysfunction(left ventricular ejection fraction <45%), dyspnea with NYHA III/NYHA IV class, patients with history of previous cardiac intervention, patients with prior cerebrovascular events (CVE)/stroke, patients with CKD and patients with body mass index (BMI) >30 kg/m2 were included.
Collected data
We assessed demographic – age, sex, anthropometric - BMI, history of cardiac intervention and stroke, diabetes, infective endocarditis, COPD, NYHA class, LVEF, laboratory - HbA1c and creatinine level.
Perioperative data included types of MICVS – mitral valve (MVR) and aortic valve (AVR) replacement, mitral valve and tricuspid valve repair, cardiopulmonary bypass time (CPB), mechanical ventilation duration, length of intensive care unit (ICU) and hospital stay.
The following complications were recorded: conversion to sternotomy, re-exploration , heart block, arrhythmia (atrial fibrillation, AF), wound infection, septicemia, CVE, and re-intubation.
Surgery procedure
As far as cannulation strategies for cardiopulmonary bypass are concerned, femoral vessels were surgically isolated and cannulated using peripheral arterial and venous cannulas. In most cases, right anterior mini thoracotomy (RAMT) was performed with peripheral cannulation for CPB. Mini J-shaped sternotomy with central cannulation was performed in some aortic valve surgeries. St. Thomas cardioplegia solution was used in all the patients.
Statistical analysis
Data are presented as number (%) and mean SD.
Results
Clinical characteristics
Out of 100 patients included in the study, 47 were male and 53 were female. The mean age in our study was 43.26 (12.80) years, 13 patients were above the age of 60 years. As far as the significant previous history of the patient is concerned, 13 had infective endocarditis, 11 had previous cardiac intervention (balloon mitral valvuloplasty, mitral commissurotomy, balloon aortic valvuloplasty), 11 had COPD and 4 had previous history of stroke. The mean BMI was 25.53 (3.54) kg/m2, 60 patients had NYHA class III and 40 patients had NYHA class II. According to PAH severity, 22 patients had severe PAH, 6 patients had moderate, and 26 had mild PAH (Table 1).
According to biochemical parameters, 64 patients were diabetic having HbA1C > 7% and 9 patients had CKD of whom two patients were on maintenance hemodialysis. Left ventricular function wise, 84 atients had preserved LVEF, 14 patients had moderate LVD and two patients had severe LVD.
|
Table 1. Clinical characteristics |
|
|
Variables |
Number or mean (SD) |
|
Male, n Female, n |
47 53 |
|
Mean age, years |
43.26 (12.80) |
|
Infective endocarditis, n |
13 |
|
COPD, n |
11 |
|
History of stroke, n |
4 |
|
Previous cardiac intervention, n |
11 |
|
Mean BMI, kg/m2 |
25.53 (3.54) |
|
NYHA Class, n Class-I Class-II Class-III Class-IV |
0 40 60 0 |
|
HbA1c, n > 7 % < 7 % |
64 36 |
|
Serum creatinine, n <1.2 mg/dL >1.2 mg/dL |
91 09 |
|
LVEF, n <30 % 31-50 % >51 % |
2 14 84 |
Perioperative data
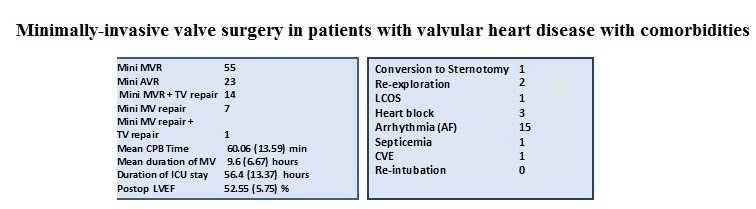
Among 100 patients, 77 patients had undergone minimally invasive mitral/tricuspid valve intervention through right anterolateral thoracotomy in the 4th intercostal space (ICS)/ 3rd ICS and 23 patients had undergone minimally invasive aortic valve surgery through right anterior thoracotomy in the 2nd ICS/ through median upper J shaped hemi sternotomy (Table 2). Intraoperative and postoperative parameters are shown in Table 3.
|
Table 2. Technique of MICVS |
|
|
MICVS |
No of patients |
|
Mini MVR |
55 |
|
Mini AVR |
23 |
|
Mini MVR + TV repair |
14 |
|
Mini MV repair |
7 |
|
Mini MV repair + TV repair |
1 |
|
Total |
100 |
|
AVR - aortic valve replacement, MICVS – minimally invasive cardiac surgery, MV – mitral valve, MVR - mitral valve replacement, TV – tricuspid valve |
|
|
Table 3. Intraoperative and postoperative data |
|
|
Variables |
Mean (SD) |
|
Mean CPB Time, min |
60.06 (13.59) |
|
Mean duration of mechanical ventilation, hours |
9.6 (6.67) |
|
Mean duration of ICU stay, hours |
56.4 (13.37) |
|
Mean duration of hospital stay, days |
4.85 (1.05) |
|
Mean postoperative LVEF, % |
52.55 (5.75) |
|
CPB – cardiopulmonary bypass, ICU – intensive care unit, LVEF – left ventricular ejection fraction |
|
Complications (Table 4)
Among all of the 100 patients, there was no paravalvular leak in the postoperative period. Fifty-four patients had mild right ventricular dysfunction and one patient of mini MVR developed severe right ventricular dysfunction. One patient developed complete atrioventricular block after mini AVR and required permanent pacemaker implantation in the same setting. One patient developed right common femoral artery stenosis after decannulation, so an interposition PTFE graft was placed in common femoral artery. In one patient re-exploration was done for bleeding. There was one death out of total 100 patients (1% mortality). That patient who underwent mini MVR, developed severe right ventricular dysfunction intraoperatively after weaning off CPB, so converted to midline sternotomy and veno-arterial extracorporeal membrane oxygenation (VA ECMO) was instituted, however patient expired on post-operative day 3 due to low cardiac output syndrome and multi organ dysfunction. The rate of conversion to midline (open) sternotomy was 1% (Table 5).
|
Table 4. Complications of MICVS |
|
|
Complication |
Number of patients |
|
Conversion to Sternotomy |
1 |
|
Re-exploration |
2 |
|
LCOS |
1 |
|
Heart block |
3 |
|
Arrhythmia (AF) |
15 |
|
Wound Infection |
0 |
|
Septicemia |
1 |
|
CVE |
1 |
|
Re-intubation |
0 |
|
AF – atrial fibrillation, CVA – cerebrovascular event, LCOS – low cardiac output syndrome, MICVS – minimally invasive cardiac surgery |
|
Discussion
Since ages, midline sternotomy has remained the standard and preferred approach for most cardiac surgery including valve surgeries and surgeries performed using CPB. MICVS has remained under scepticism due to a higher learning curve and limited surgical site exposure. However, with advancements in technology, instrumentation, techniques, and well-trained surgeons in minimally invasive surgery, many canters have proven time and over that MICVS is equally safe quality-wise with better cosmetics and less trauma (2).
However, data on MICVS are limited. Sternotomy has its own complications. Apart from being associated with cosmetically disfiguring scars, there are risks of complications, e.g. sternal instability, dehiscence and deformity, wound infection and postoperative sternal and scar pain, blood loss, and prolonged hospital stay (2).
In the last three decades, MICVS with peripheral cannulation has gained widespread acceptance in adults with good results in a wide range of congenital and acquired cardiac diseases. The minimally invasive nature of this procedure reduceS the incidence of postoperative mediastinitis and wound pain to a minimum. It can provide the promise of expediency, safety, minimal discomfort, less postoperative pain, quick functional recuperation, excellent cosmetic healing, shortened hospital stays, and therefore savings in cost. However, these potential benefits may come with an increased risk of stroke, aortic dissection or aortic injury, phrenic nerve palsy, groin infections/complications, and increased cross-clamp, CPB, and procedure time. During the last two decades, there has been considerable emphasis on sternal sparing and cosmetically superior approaches. Hence, several alternative minimally invasive approaches have been described however; the most commonly utilized include a right anterior or lateral thoracotomy, an upper hemisternotomy, and the use of robotic technology (2).
Left ventricular dysfunction
In our study, 18% of patients undergoing MICVS had LVD. The incidence of operative mortality, re-exploration, acute kideny injury, low cardiac output syndrome (LCOS), and CVE was 0. The average hospital length of stay was 4.15 (1.05) days. Tabata and colleagues conducted a retrospective review of 140 patients with a LVEF ≤40% undergoing AVR, and compared the results of 41 matched pairs who had MICVS via an upper hemisternotomy or full sternotomy (3).
The incidence of operative mortality (2.4% vs. 4.4.9%, p=0.56), acute kidney injury (0 vs. 2.4%, p=0.32), CVE (0 vs. 2.4%, p=0.32), and hospital length of stay (8.5 vs. 10.6 days, p=0.17), was similar between MICVS vs. sternotomy (3). Garbade et al. (4) reported the outcomes of 71 patients with severe LVD and secondary mitral regurgitation undergoing MICVS via a right thoracotomy. There were 31 (44%) patients that had mitral valve repair, and 40 (56%) that had MVR. No patient required conversion to sternotomy. There was 1 (1.4%) CVE, 5 (7%) patients developed acute kideny injury, and there were no re-operations for bleeding. The median hospital length of stay was 6 days (IQR 5–9 days), with in-hospital mortality of 2.8%, which was lower than the STS predicted mortality of 6.6%. These studies demonstrate that in patients with LVD, MICVS can be performed safely with satisfactory perioperative outcomes.
Obesity
High BMI in patients undergoing cardiac surgery is associated with an increased risk of perioperative morbidity, including deep sternal wound infections, respiratory and renal complications, and prolonged ICU and hospital length of stay (5). In our study, 9% of patients were from the obese group (BMI>30kg/m2) and 52% of patients were from the overweight group. This group required longer operative times but no patient required conversion to sternotomy for inadequate field exposure. Two patients developed basal atelectasis in the postoperative period. No incidence of postoperative renal failure, reintubation, deep wound infection, pneumonia, sepsis, bleeding requiring re-exploration, stroke, or death was recorded. The average hospital length of stay in this group was 4.65 (1.05) days. Santana et al. (6) reported the results of 160 consecutive obese patients with a body mass index >30 kg/m2 who underwent isolated mitral and/or aortic valve surgery. The outcomes of 64 patients who underwent MICVS via a right thoracotomy were compared with 96 who had sternotomy. The baseline characteristics were similar between groups. The MICVS group experienced longer operative times; however, no patient required conversion to sternotomy for inadequate surgical field exposure. When compared with sternotomy, the composite of postoperative complications, which were defined as the presence of postoperative renal failure, prolonged ventilation, reintubation, deep wound infection, pneumonia, sepsis, bleeding requiring re-exploration, stroke, or death, occurred significantly less in patients undergoing MICVS (23.5% vs. 51%, p=0.034), with a lower incidence of acute kideny injury (0 vs. 6.3%, p=0.041), prolonged mechanical ventilation (18.7% vs. 34.3%,p=0.049), and need for re-intubation (4.7% vs. 15.6%, p=0.032). Additionally, a MICVS approach was associated with a reduction in the hospital length of stay [7.7 (IQR, 5–9) vs. 11.7 (IQR, 7–16) days, p<0.001] compared with sternotomy.
This study demonstrated not only that MICVS is feasible in the obese, but also that it is associated with a significant reduction in morbidity and mortality when compared with sternotomy, despite longer operative times. There were no differences in the occurrence of major adverse cardiac and cerebrovascular events; however, the obese patients did have longer ventilation times. The authors concluded that obesity should not deter a surgeon from selecting MICVS.
Chronic obstructive pulmonary disease and pulmonary hypertension
The prevalence of COPD is estimated to be as high as 27% in patients undergoing cardiac surgery (7). After sternotomy, there is the development of diaphragmatic dysfunction, with a reduction in vital capacity of 55% and functional residual capacity of 30% (8). These effects are exacerbated in patients with underlying COPD and contribute to the development of atelectasis, pneumonia, and ventilation/ perfusion mismatching. It is hypothesized that the improved thoracic stability noted with MICVS, as well as less surgical trauma and decreased mechanical ventilation time, leads to earlier mobilization and normalization of pulmonary function.
In our study group, 11% of patients had COPD and 26%, 2% & 22% of patients had mild, moderate and severe PAH respectively undergoing minimally invasive mitral/aortic valve surgery. One patient of moderate PAH developed severe right ventricular dysfunction intraoperatively, because of not being able to wean off CPB, thoracotomy converted to sternotomy, and VA ECMO instituted in view of severe RV dysfunction; due to LCOS, acute kidney injury, multi organ dysfunction and sepsis patient died on postoperative day 3. Two patients with COPD developed right basal atelectasis. The mean duration of mechanical ventilation required in the postoperative period was 8.6 (4.17) hours. The mean duration of ICU stay was 58.4 (13.37) hours. The mean hospital length of stay was 4.96 (1.35) days.
In a study of 165 patients with COPD who had isolated aortic or mitral valve surgery, Santana et al. (6), compared the results of 100 patients who underwent MIVS via a right thoracotomy with 65 who had sternotomy. The baseline characteristics did not differ between the two groups. In patients undergoing MICVS, the COPD severity was mild, moderate, or severe in 15%, 82%, and 3% of the patients, while in the sternotomy group, 19% were mild, 75% were moderate, and 6% were severe (p=0.49). There were no required conversions to sternotomy in patients undergoing MICVS, and the incidence of operative mortality was similar (MICVS 1%, sternotomy 5%, p=0.14). The composite post-operative complications were reduced in the MICVS group (30% vs. 54%, p=0.002), which was driven by less prolonged mechanical ventilation (13% vs. 28%, p=0.02), as compared with sternotomy. Finally, a MICVS approach decreased the ICU and hospital length of stay by 24 hours and 3 days respectively (p<0.001, for both). Perioperative complications occur in approximately 14% of patients with pulmonary hypertension, and this risk increases commensurate with the severity of the disease (9).
The outcomes of a right thoracotomy MICVS for aortic and/or mitral valve surgery were analyzed in 569 patients with PAH, with a mean pre-operative pulmonary artery pressure of 33 (8) mmHg (10). The PAH severity was mild in 48% of the patients, moderate in 35%, and severe in 17%. There were 76 (13%) combined mitral and aortic valve operations, and no patient required conversion to sternotomy. Operative mortality occurred in 20 (3.5%) patients, 8 (1.4%) had a CVE, and the mean ICU and hospital length of stay were 50 (14) hours and 7 (1) days, respectively. Despite a longer mechanical ventilation time and ICU length of stay, patients with severe PAH (mean pulmonary artery pressure ≥40 mmHg) had similar outcomes to those with mild or moderate disease, highlighting the safety and feasibility of MICVS in this population.
Infective endocarditis
The incidence of infective endocarditis is cited at 1.4 to 6.2 cases per 100,000 person-years, with the mitral valve affected in approximately two-thirds of patients with left-sided valvular endocarditis (11). Despite advancements in medical and surgical therapy, morbidity remains high, with 10-year overall and event-free survival reported to be 50% and 17%, respectively. When considering surgical intervention, mitral valve repair is favoured over replacement given its association with superior short- and long-term outcomes (12).
In our study group, 12% had infective endocarditis of the mitral valve and one patient had of aortic valve. Twelve patients underwent valve replacement surgery and 1 patient (age 22, male) underwent valve repair surgery through mini thoracotomy. There were no incidences of conversion to sternotomy, re-exploration, LCOS, wound infection, sepsis, CVE, acute kidney injury, or death.
Mihos et al. (13), reported their outcomes of 50 patients with native mitral valve endocarditis undergoing surgical intervention. The results of 22 patients who had MICVS via a right thoracotomy were compared with 28 patients who had sternotomy. There were no baseline differences noted between groups, no patient undergoing MICVS required a conversion to sternotomy. Disease burden, as measured by the presence of chordal rupture, annular abscess, cusp perforation, and vegetation size, was similar between the groups. A MICVS approach was associated with a decreased incidence of sepsis (0 vs. 21%, p=0.02), less use of intraoperative blood products (59% vs. 93%, p=0.004), higher rates of mitral valve repair (56% vs. 21%, p=0.02), and shorter ICU length of stay (56 vs. 114 hours, p=0.009), as compared with sternotomy. There was no difference in in-hospital mortality (5% vs. 14%, p=0.25), or 2.5-year actuarial survival (80% vs. 68%, p=0.33), between a MICVS vs. sternotomy approach. This study, though limited by its small size and retrospective nature, did demonstrate a significant reduction in post-operative complications with MICVS.
Study limitations
The available evidence concerning the outcomes of MICVS in higher-risk patients is limited, due to the fact that the results were mainly derived from single- centre, retrospective studies, and thus are subject to significant selection bias. In addition, the cohorts tended to be small in size and provided only short-term outcomes.
Conclusion
The study highlights the significance of careful patient selection and surgeon experience, as well as the difficulties and complexities of applying MICVS in this specific patient group. In comparison to conventional methods, MICVS appears to have more promising results for this specific patient group with multiple co-morbidities, such as fewer postoperative complications, shorter mechanical ventilation time, shorter hospital and ICU stay, and a tendency towards quicker recovery. This study's finding showed that skilled surgical teams could achieve appropriate exposure of the operative field with similar quality operation with better cosmetics, less trauma, and better outcomes. Therefore, MICVS should be promoted in suitable cases in well-experienced hands and will become widely adopted especially in patients with multiple co-morbidities as patients will ask for less invasive approaches.
Ethics: A written informed consent was obtained from the patients.
This study was approved by the institutional ethics committee (UNMICRC/CVTS/2019/20).
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: M.S., K.L., R.K., H.P., and C.D. equally contributed to the study and preparation for manuscript, and fulfilled authorship criteria.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
References
| 1.Claessens J, Rottiers R, Vandenbrande J, Gruyters I, Yilmaz A, Kaya A, et al. Quality of life in patients undergoing minimally invasive cardiac surgery: a systematic review. Indian J Thorac Cardiovasc Surg 2023; 39: 367-80. doi: 10.1007/s12055-023-01501-y https://doi.org/10.1007/s12055-023-01501-y PMid:37346428 PMCid:PMC10279589 |
||||
| 2.Langer NB, Argenziano M. Minimally invasive cardiovascular surgery: incisions and approaches. Methodist Debakey Cardiovasc J 2016; 12: 4-9. doi: 10.14797/mdcj-12-1-4 https://doi.org/10.14797/mdcj-12-1-4 PMid:27127555 PMCid:PMC4847968 |
||||
| 3.Tabata M, Aranki SF, Fox JA, Couper GS, Cohn LH, Shekar PS. Minimally invasive aortic valve replacement in left ventricular dysfunction. Asian Cardiovasc Thorac Ann 2007; 15: 225-8. https://doi.org/10.1177/021849230701500310 PMid:17540992 |
||||
| 4.Garbade J, Seeburger J, Merk DR, Pfannmüller B, Vollroth M, Barten MJ, et al. Mitral valve pathology in severely impaired left ventricles can be successfully managed using a right-sided minimally invasive surgical approach. Eur J Cardiothorac Surg 2013; 44: e1-7. https://doi.org/10.1093/ejcts/ezt144 PMid:23520235 |
||||
| 5.Virani SS, Nambi V, Lee VV, Elayda MA, Pan W, Petersen LA, et al. Obesity: an independent predictor of in-hospital postoperative renal insufficiency among patients undergoing cardiac surgery?. Texas Heart Inst J 2009; 36: 540. | ||||
| 6.Santana O, Reyna J, Benjo AM, Lamas GA, Lamelas J. Outcomes of minimally invasive valve surgery in patients with chronic obstructive pulmonary disease. Eur J Cardiothorac Surg 2012; 42: 648-52. https://doi.org/10.1093/ejcts/ezs098 PMid:22555309 |
||||
| 7.Leavitt BJ, Ross CS, Spence B, Surgenor SD, Olmstead EM, Clough RA, et al. Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation 2006; 114(1 suppl): I-430. https://doi.org/10.1161/CIRCULATIONAHA.105.000943 |
||||
| 8.Weissman C. Pulmonary function after cardiac and thoracic surgery. Anesth Analg 1999; 88: 1272-9. https://doi.org/10.1213/00000539-199906000-00014 https://doi.org/10.1097/00000539-199906000-00014 PMid:10357329 |
||||
| 9.Kennedy JL, LaPar DJ, Kern JA, Kron IL, Bergin JD, Kamath S, et al. Does the Society of Thoracic Surgeons risk score accurately predict operative mortality for patients with pulmonary hypertension? J Thorac Cardiovasc Surg 2013; 146: 631-7. https://doi.org/10.1016/j.jtcvs.2012.07.055 PMid:22982034 |
||||
| 10.Gosain P, Larrauri-Reyes M, Mihos CG, Escolar E, Santana O. Aortic and/or mitral valve surgery in patients with pulmonary hypertension performed via a minimally invasive approach. Interact Cardiovasc Thorac Surg 2016; 22: 668-70. https://doi.org/10.1093/icvts/ivw019 PMid:26892195 PMCid:PMC4892159 |
||||
| 11.Tleyjeh IM, Abdel-Latif A, Rahbi H, Scott CG, Bailey KR, Steckelberg JM, et al. A systematic review of population-based studies of infective endocarditis. Chest 2007; 132: 1025-35. https://doi.org/10.1378/chest.06-2048 PMid:17873196 |
||||
| 12.Feringa HH, Shaw LJ, Poldermans D, Hoeks S, van der Wall EE, Dion RA, et al. Mitral valve repair and replacement in endocarditis: a systematic review of literature. Ann Thoracic Surg 2007; 83: 564-70. https://doi.org/10.1016/j.athoracsur.2006.09.023 PMid:17257988 |
||||
| 13.Mihos CG, Santana O, Pineda AM, Lamas GA, Lamelas J. Right anterior minithoracotomy versus median sternotomy surgery for native mitral valve infective endocarditis. J Heart Valve Dis 2014; 23: 343-9. | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

