Management of cardiogenic shock in older adults: A commentary on the 2024 American Heart Association Scientific Statement
EDITORIALS
Management of cardiogenic shock in older adults: A commentary on the 2024 American Heart Association Scientific Statement
Article Summary
- DOI: 10.24969/hvt.2024.496
- Page(s): 323-326
- CARDIOVASCULAR DISEASES
- Published: 06/07/2024
- Received: 27/06/2024
- Accepted: 28/07/2024
- Views: 5683
- Downloads: 3072
- Keywords: Mechanical ventilation, renal replacement therapy, coronary revascularization, mechanical circulatory support, palliative care
Address for Correspondence: Stefano Cacciatore, Department of Geriatrics, Orthopedics and Rheumatology, Università Cattolica del Sacro Cuore, L.go F. Vito 1, 00168 Rome, Italy. Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, L.go A. Gemelli 8, 00168 Rome, Italy.
E-mail: stefano.cacciatore01@icatt.it ORCID ID: 0000-0001-7504-3775 X/Twitter: @stecacMD
Chieh-en Hsu1, Alberto Emanuele Fratta1, Stefano Cacciatore1,2
1Università Cattolica del Sacro Cuore, L.go F. Vito 1, 00168 Rome, Italy
2Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, L.go A. Gemelli 8, 00168 Rome, Italy
Abstract
Cardiogenic shock occurring in older adults is associated with higher short-term mortality rates and poorer outcomes. However, current evidence and dedicated approaches in clinical practice to assess and manage this condition in older adults are limited. The American Heart Association (AHA) has issued a scientific statement to tackle the primary issues related to the risk of cardiogenic shock in older persons, as well as to provide potential solutions for its optimal management. This editorial delves into the primary principles examined by the AHA concerning decision-making process, clinical management practices, and forthcoming strategies for the treatment of older patients with cardiogenic shock.
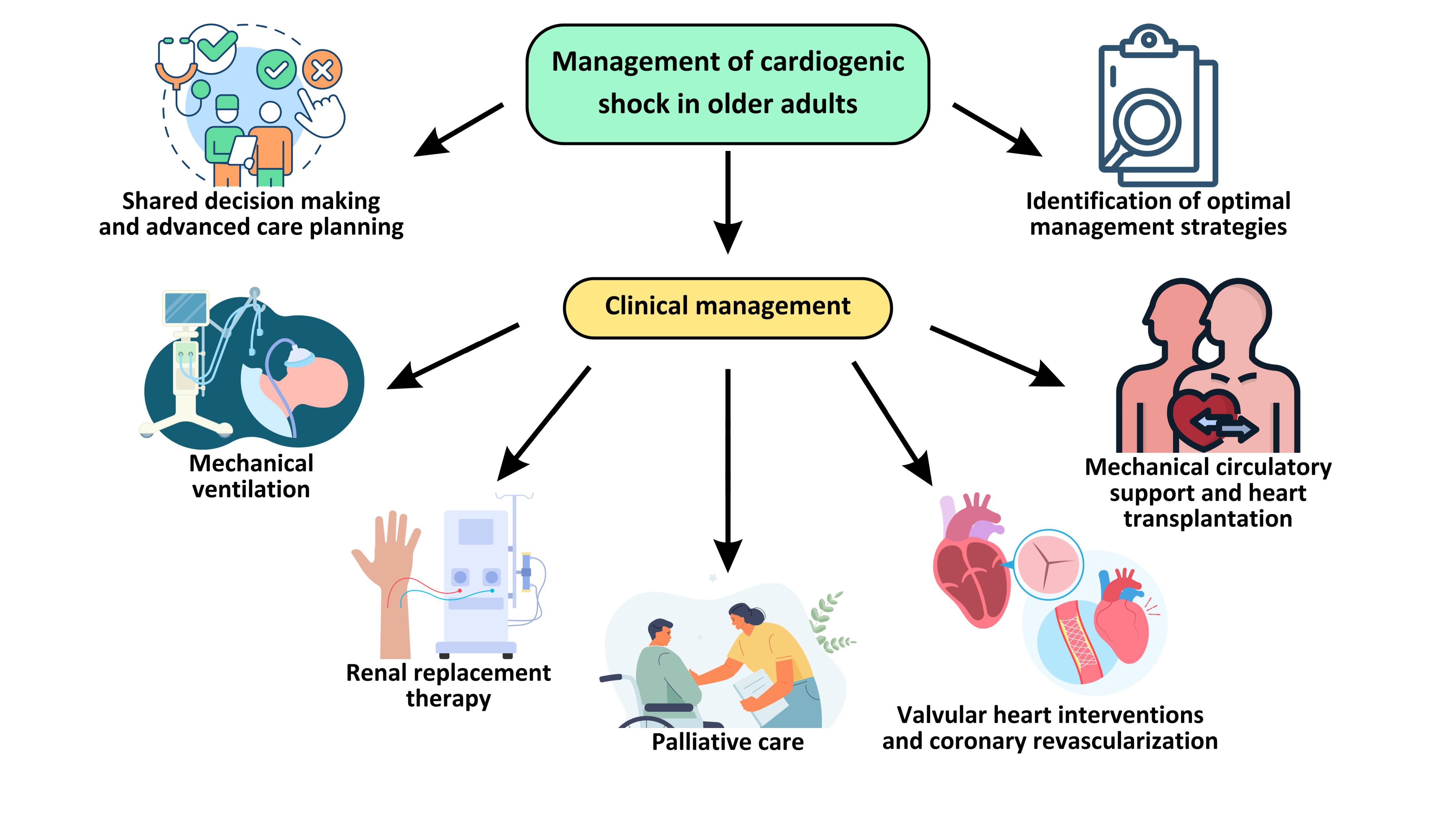
Graphical abstract
Key words: Mechanical ventilation, renal replacement therapy, coronary revascularization, mechanical circulatory support, palliative care
Introduction
Cardiogenic shock (CS) occurring in older adults poses significant challenges due to higher short-term mortality and worse outcomes. However, available evidence and dedicated approaches in clinical practice to assess and manage this condition in older adults are limited. The American Heart Association (AHA) has issued a scientific statement that focuses on the primary problems related to CS in older adults and provides valuable insights for its optimal management (1).
This editorial explores the key concepts explored by the AHA about the decision-making process, clinical management techniques, and future initiatives for treating older patients with CS.
Decision-making and advanced care planning
The management of older adults necessitates addressing a greater level of care complexity as compared to younger patients. Frailty is common in older patients, especially in those with significant cardiovascular impairment, along with deficits in several domains including physical, cognitive, social, and functional areas (2). As a result, the main outcomes in geriatric medicine are seldom univocal and go beyond mortality alone, including prolonged hospitalization, repeated hospital admissions, deterioration in physical and cognitive abilities, disability, and reduced quality of life (3). Considering the significant tradeoffs associated with different treatment approaches, especially for major adverse events such as CS, shared decision-making is a fundamental principle in the management of older adults (4). For the above reasons, the AHA recommends focusing on enhancing the communication abilities, and implementing interdisciplinary management and advanced care planning (ACP) as crucial areas for improvements (1). ACP holds particular significance for older adults with CS, since it can be defined as the process of giving value to the patients’ preferences and long-term life ambitions, so that surrogate decision-makers can transform these values into tailored medical care strategies (5).
Clinical managements
Mechanical ventilation
Due to the complexities associated with CS, a significant number of older patients experiencing CS may eventually require mechanical ventilation (MV) to sustain their respiratory function (1). The statement highlights the preference for invasive MV over non-invasive methods, as invasive MV typically results in more significant improvements in hemodynamic parameters and better clinical outcomes. However, the decision to use invasive positive pressure ventilation in cases of CS must be made carefully, considering potential adverse effects in specific clinical contexts. Additionally, it is crucial to respect patient preferences, assess their attitudes towards cardiopulmonary resuscitation and prolonged MV, and incorporate these factors into the treatment decision-making process (6).
Renal replacement therapy
Older patients with underlying renal conditions and CS often require renal replacement therapy (RRT). The American Heart Association (AHA) recommends continuous RRT (CRRT) over intermittent methods due to concerns about hemodynamic instability and the potential adverse effects of significant intravascular volume shifts (1). A study by Conroy et al. (7) found that among intensive care unit (ICU) patients needing CRRT, older adults did not show significantly higher mortality rates in the ICU or dependency on dialysis compared to younger counterparts. However, they experienced higher in-hospital mortality rates and poorer long-term outcomes (7). Recent research has underscored the importance of frailty in determining outcomes for patients with CS. Beyond age, factors such as baseline renal function, comorbidities, quality of life considerations, and individual patient goals and priorities should be considered when making treatment decisions (8).
Coronary revascularization
CS further increases the risks associated with ischemic heart disease in older adults (2,9). AHA statement emphasized the clinical management of acute myocardial infarction complicated by cardiogenic shock (AMI-CS) in older adults, focusing primarily on percutaneous coronary intervention (PCI) and surgical revascularization (1).
PCI, being less invasive, is the preferred method for early revascularization in older patients, showing significant improvement in in-hospital mortality rates among those with AMI-CS (10). Alternatively, surgical revascularization, notably coronary artery bypass grafting (CABG), aims for comprehensive revascularization and addresses concomitant valvular or mechanical complications of AMI. CABG becomes an option when PCI is not feasible or highly indicated. However, as a more invasive procedure, CABG carries a higher in-hospital mortality rate of up to 50%. Therefore, the decision to proceed with CABG surgery must carefully weigh the preoperative burden of geriatric syndromes and postoperative risks. Therefore, the decision to proceed with CABG surgery must carefully weigh the preoperative burden of geriatric syndromes and postoperative risks (2, 9).
Valvular intervention
Acute valvular heart disease (VHD) can lead to significant hemodynamic compromise and CS) Therefore, various treatment options are suggested for managing acute VHD in older individuals. These include transcatheter aortic valve replacement, urgent cardiac surgery, and chordal-sparing mitral valve replacement (1). Given that surgical valve repair or replacement often comes with higher mortality rates, a higher risk of multiple comorbidities, and prolonged recovery periods, transcatheter therapies present a viable alternative for clinical management (11).
Temporary and durable mechanical circulatory support and heart transplantation
In recent years, the availability of temporary mechanical circulatory support (t-MCS) devices has seen a significant increase in managing CS. However, as noted, deciding to employ t-MCS in older adults necessitates careful deliberation and is typically undertaken with a clear exit strategy in mind. Given its aggressive nature, it is vital to avoid futile t-MCS interventions, with patient preference being paramount; individuals with explicit do-not-resuscitate preferences should not be considered candidates (1). T-MCS serves as a potential bridge to durable MCS or to stabilize patients while on a heart transplantation (HT) waiting list (12). It effectively postpones the decision-making process regarding durable solutions, proving invaluable for navigating the sensitive terrain of HT decisions in the context of CS. Nevertheless, early evaluation for durable MCS or HT is crucial for patients who cannot be weaned off t-MCS (1). Concerning the implantation of durable MCS, particularly durable left ventricular assist devices (LVADs), studies have indicated that age independently predicts mortality post-implantation, suggesting potential suboptimal outcomes with this strategy (13). Furthermore, evaluating older adults considered for durable LVAD should prioritize assessing comorbidities associated with advanced heart failure, such as frailty, end-organ dysfunction, malnutrition, and available caregiver support (1). Additionally, as urgent HT from a CS state gradually becomes a common strategy among older adults, studies show that carefully selected older adult HT recipients have similar survival, rehospitalization, and graft failure rates compared to younger patients, making individual transplant programs begin to view the upper age limit for candidate consideration (13). However, the ethical concern regarding the allocation of organs due to scarcity is still controversial, and whether it is the optimal treatment option for multi-comorbid older adults is an issue that requires discussion (13, 14).
Palliative and end-of-life care
When facing CS, it is important to note that the expected outcomes for elderly patients may differ from those of younger patients, as many prioritize quality of life over increased longevity in treatment decisions. According to the statement, palliative therapy is particularly important for patients unlikely to benefit from advanced therapies (1). It also plays an essential role for patients undergoing advanced therapy, aiding in decision-making and offering crucial support in case of adverse outcomes (1). With the increasing demand for palliative care for cardiogenic shock (PCCS), there should be a corresponding increase in trained physicians specialized in palliative care. Moreover, the integration of PCCS should be considered early in the management of all elderly patients with cardiogenic shock, irrespective of their projected trajectory and eligibility for advanced therapies (15, 16).
Future directions
Older adults constitute a distinct age subgroup with unique care needs and objectives. Particularly when addressing crucial diseases like CS, the considerations extend beyond mere mortality rates, encompassing factors such as quality of life and patient preferences regarding treatment outcomes. Despite the significant proportion of older adults affected by CS, current clinical trials and registries fall short in generating robust recommendations tailored to this demographic.
Additionally, the criteria used in clinical settings to determine the escalation of care for older adults often lack sufficient empirical support (1).
Consequently, there is a pressing need for additional research focusing on older CS patients and the development of more effective risk assessment tools tailored to this population. Furthermore, the prediction and optimal management of out-of-hospital cardiac arrest in older adults require special attention (17). Effective strategies and personalized approaches are essential to improve outcomes and quality of life for older patients experiencing such critical events.
Conclusion
In this statement, the AHA offers practical recommendations for managing CS in older adults. It is crucial to understand that age is not the sole factor in decision-making; rather, patient needs and preferences play a significant role. Therefore, a comprehensive, multidisciplinary approach is essential, emphasizing shared decision-making between physicians and patients. Additionally, further research is needed to develop clinical practice guidelines specifically tailored to managing CS in older adults.
Peer-review: internal
Conflict of interest: None to declare
Authorship: Ch-E.H., A.E.F., and S. C. have participated in manuscript design and drafting. All authors read and approved the final version, and fulfilled authorship criteria.
Acknowledgements and funding: The authors have not declared a specific grant for this work from any funding agency in the public, commercial or not-for-profit sectors.
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
References
| 1.Blumer V, Kanwar MK, Barnett CF, Cowger JA, Damluji AA, Farr M, et al. Cardiogenic shock in older adults: a focus on age-associated risks and approach to management: A Scientific Statement From the American Heart Association. Circulation 2024; 149: e1051-e65. https://doi.org/10.1161/CIR.0000000000001214 https://doi.org/10.1161/CIR.0000000000001214 PMid:38406869 PMCid:PMC11067718 |
||||
| 2.Cacciatore S, Spadafora L, Bernardi M, Galli M, Betti M, Perone F, et al. Management of coronary artery disease in older adults: recent advances and gaps in evidence. J Clin Med 2023;12. https://doi.org/10.3390/jcm12165233 https://doi.org/10.3390/jcm12165233 PMid:37629275 PMCid:PMC10455820 |
||||
| 3.Cunha AIL, Veronese N, de Melo Borges S, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Res Rev 2019; 56: 100960 doi:10.1016/j.arr.2019.100960 https://doi.org/10.1016/j.arr.2019.100960 PMid:31518686 |
||||
| 4. Backman WD, Levine SA, Wenger NK, Harold JG. Shared decision-making for older adults with cardiovascular disease. Clin Cardiol 2020;43:196-204. doi: 10.1002/clc.23267 https://doi.org/10.1002/clc.23267 PMid:31580493 PMCid:PMC7021653 |
||||
| 5.Lum HD, Sudore RL. Advance care planning and goals of care communication in older adults with cardiovascular disease and multi-morbidity. Clin Geriatr Med 2016; 32: 247-60. Doi: 10.1016/j.cger.2016.01.011 https://doi.org/10.1016/j.cger.2016.01.011 PMid:27113144 PMCid:PMC5711730 |
||||
| 6.Wiesen J, Ornstein M, Tonelli AR, Menon V, Ashton RW. State of the evidence: mechanical ventilation with PEEP in patients with cardiogenic shock. Heart 2013; 99: 1812-7. Doi: 10.1136/heartjnl-2013-303642 https://doi.org/10.1136/heartjnl-2013-303642 PMid:23539555 PMCid:PMC4096289 |
||||
| 7.Conroy M, O'Flynn J, Marsh B. Mortality and long-term dialysis requirement among elderly continuous renal replacement therapy patients in a tertiary referral intensive care unit. J Intensive Care Soc 2019; 20: 138-43. Doi: 10.1177/1751143718784868 https://doi.org/10.1177/1751143718784868 PMid:31037106 PMCid:PMC6475982 |
||||
| 8.Jamil Y, Park DY, Rao SV, Ahmad Y, Sikand NV, Bosworth HB, et al. Association between frailty and management and outcomes of acute myocardial infarction complicated by cardiogenic shock. J Am Coll Cardiol Advances 2024; 3. Doi: 10.1016/j.jacadv.2024.100949 https://doi.org/10.1016/j.jacadv.2024.100949 PMid:38938859 PMCid:PMC11198471 |
||||
| 9. Cacciatore S, Martone AM, Landi F, Tosato M. Acute coronary syndrome in older adults: an Update from the 2022 Scientific Statement by the American Heart Association. Heart, Vessels and Transplantation 2023; 7. Doi: 10.24969/hvt.2023.367 https://doi.org/10.24969/hvt.2023.367 |
||||
| 10.Damluji AA, Bandeen-Roche K, Berkower C, Boyd CM, Al-Damluji MS, Cohen MG, et al. Percutaneous Coronary Intervention in Older Patients With ST-Segment Elevation Myocardial Infarction and Cardiogenic Shock. J Am Coll Cardiol 2019; 73: 1890-900. Doi: 10.1016/j.jacc.2019.01.055 https://doi.org/10.1016/j.jacc.2019.01.055 PMid:30999991 PMCid:PMC7185801 |
||||
| 11.Kodali SK, Velagapudi P, Hahn RT, Abbott D, Leon MB. Valvular heart disease in patients ≥80 years of age. J Am Coll Cardiol 2018; 71: 2058-72. Doi: 10.1016/j.jacc.2018.03.459 https://doi.org/10.1016/j.jacc.2018.03.459 PMid:29724358 |
||||
| 12.Abiragi M, Singer-Englar T, Cole RM, Emerson D, Esmailian F, Megna D, et al. Temporary mechanical circulatory support in patients with cardiogenic shock: clinical characteristics and outcomes. J Clin Med 2023; 12. Doi: 10.3390/jcm12041622 https://doi.org/10.3390/jcm12041622 PMid:36836157 PMCid:PMC9965226 |
||||
| 13.Rushakoff JA, Kransdorf EP. Heart transplant in older adults. Curr Transplant Rep 2022 ;9: 48-54. Doi: 10.1007/s40472-022-00358-1 https://doi.org/10.1007/s40472-022-00358-1 PMid:35039790 PMCid:PMC8755401 |
||||
| 14.Bunnik EM. Ethics of allocation of donor organs. Curr Opin Organ Transplant 2023; 28: 192-6. Doi: 10.1097/MOT.0000000000001058 https://doi.org/10.1097/MOT.0000000000001058 PMid:36787240 PMCid:PMC10155689 |
||||
| 15. Vallabhajosyula S, Prasad A, Dunlay SM, Murphree DH, Jr., Ingram C, Mueller PS, et al. Utilization of palliative care for cardiogenic shock complicating acute myocardial infarction: A 15-year national perspective on trends, disparities, predictors, and outcomes. J Am Heart Assoc 2019; 8: e011954. Doi: 10.1161/JAHA.119.011954 https://doi.org/10.1161/JAHA.119.011954 PMid:31315497 PMCid:PMC6761657 |
||||
| 16.Feng Z, Fonarow GC, Ziaeian B. Palliative care services in patients admitted with cardiogenic shock in the United States: Frequency and predictors of 30-day readmission. J Card Fail 2021; 27: 560-7. DOI: 10.1016/j.cardfail.2021.01.020 https://doi.org/10.1016/j.cardfail.2021.01.020 PMid:33962743 PMCid:PMC8310778 |
||||
| 17.Spadafora L, Biondi-Zoccai G, Bernardi M. Out-of-hospital cardiac arrest: predict and then protect! EBioMedicine 2023; 90: 104517. Doi: 10.1016/j.ebiom.2023.104517 https://doi.org/10.1016/j.ebiom.2023.104517 PMid:36893589 PMCid:PMC10011734 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

