An overview of critical care management of patients after cardiac arrest: A statement towards individualized, patient-centered care
EDITORIALS
An overview of critical care management of patients after cardiac arrest: A statement towards individualized, patient-centered care
Article Summary
- DOI: 10.24969/hvt.2024.507
- Page(s): 347-349
- CARDIOVASCULAR DISEASES
- Published: 22/08/2024
- Received: 16/08/2024
- Accepted: 17/08/2024
- Views: 4925
- Downloads: 2963
- Keywords: Cardiac arrest, critical care, management, hemodynamic care, ventilation, neurological recovery, guidelines
Address for Correspondence: Gabriele Martelli, Intensive Care Unit U.O.C. Anestesia e Rianimazione, Department of Surgery, Padua University Hospital, Azienda Ospedale, Università di Padova, Via Nicolò Giustiniani, 2, 35128 Padua, Italy
E-mail: gabriele.martelli@aopd.veneto.it Twitter: Gabrielle Martelli - @G_Martelli_ ORCID: Gabriele Martelli – 0000-0001-6729-2982, Alessandra Maggiolo - 0009-0009-2693-0111
Gabriele Martelli 1, Alessandra Maggiolo2, Ivo Tiberio 1.
1Intensive Care Unit U.O.C. Anestesia e Rianimazione, Department of Surgery, Padua University Hospital, Padua, Italy
2Institute of Anesthesia and Intensive Care, Department of Medicine (DIMED), Padua University Hospital, Padua, Italy
Key words: Cardiac arrest, critical care, management, hemodynamic care, ventilation, neurological recovery, guidelines
Post-cardiac arrest care is widely regarded as a key element to improve survivors’ outcomes and quality of life.
Therefore, we greatly appreciate the commitment of Hirsch and colleagues (1) to guide the comprehensive management in the post-cardiac arrest period, from the return to spontaneous circulation to the definitive outcome. Their recent work (1), the result of the joint effort of the American Heart Association and Neurocritical Care Society, delivers statements through the expert consensus method to establish clear guidance on the issue.
The development of consensus-based statements is an innovative element of this document and differentiates it from traditional guidelines. While the guideline takes the body of literature and translates it into recommendations, taking into consideration only those aspects found in the literature (and usually from high-quality publications, e.g. RCTs), the consensus may produce additional guidance in areas that lack robust evidence.
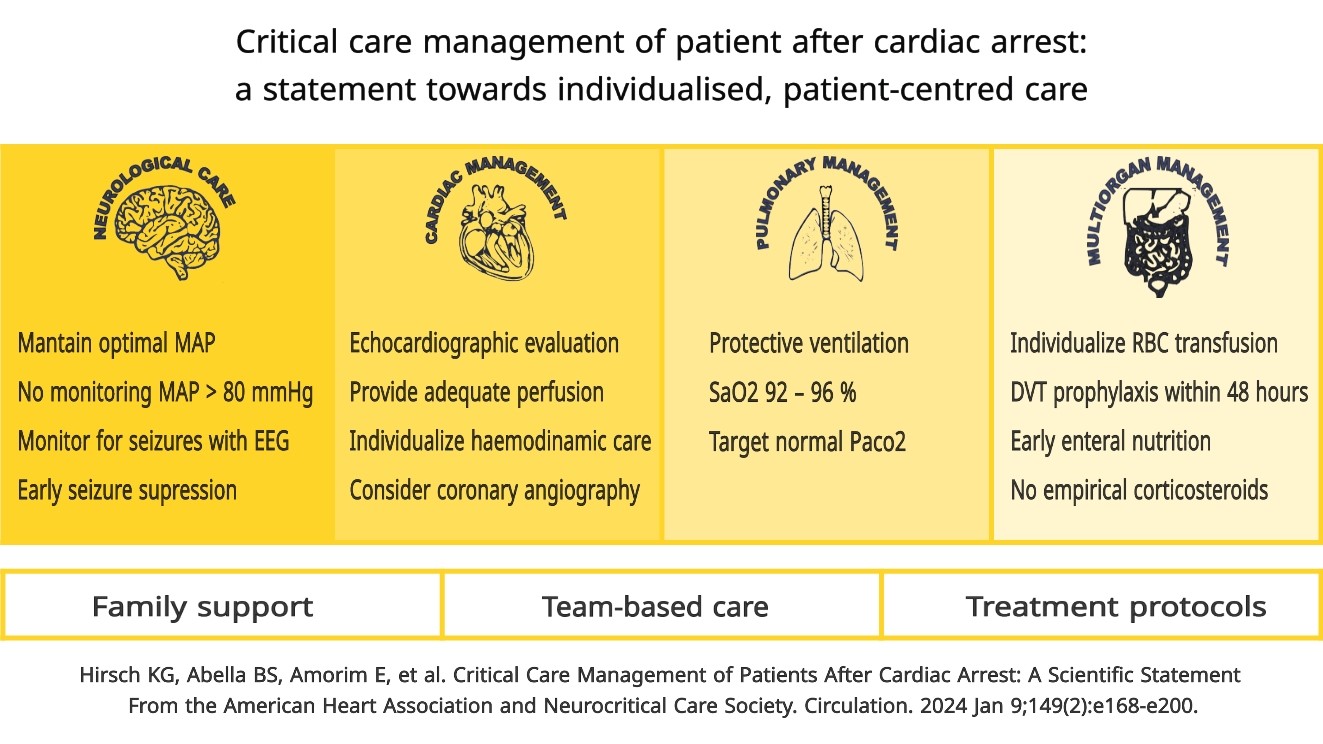
In this paper, the authors lead us to contemplate a more individualized management of the patient, discussing the significance of the usual means of treatment and the consistency of monitoring technique.
Neurological treatment recommendations are the result of this process. In recent years, the implementation of invasive and non-invasive methods of cerebral autoregulation monitoring has led to a critical review of previous treatment.
The authors recommend to identify and achieve the optimal mean arterial pressure to preserve adequate cerebral perfusion pressure when advanced monitoring is available.
In those cases where advanced monitoring is absent, the recommendation has been directed toward high-normal blood pressure values (mean arterial pressure > 80 mmHg) if no adverse consequences are suspected. This aspect was influenced by relatively recent literature, which demonstrated that actively achieving higher blood pressure is a safe treatment in most patients and can led to improved specific outcome.
However, no consensus has been reached on the initiation and duration of invasive monitoring, as there is no solid scientific evidence to guide the decision.
One area of care that lacks indications from large RCT studies but where consensus method has proved decisive is the diagnosis and treatment of post-arrest seizures.
The indication on this issue is based mainly on observational studies and case series. The statements underline the central role of EEG monitoring, particularly in patients who fail to regain consciousness and also provide an interesting perspective on treatment. They include seizure (or burst) suppression on the acute phase and, in refractory cases, even aggressive treatment if compatible with the standard of care, since neurological recovery may occur in certain subsets of patients when intensive seizure control is pursued .
The main purpose of cardiac management is to maintain organ perfusion. The statements cover the topics of monitoring, hemodynamic optimization, mechanical circulatory support and coronary reperfusion.
The document provides guidance on patient monitoring, recommending echocardiography, a useful method for assessing ventricular function, cardiac output, fluid status and to guide appropriate treatment.
Optimization of hemodynamics, based on inotropes, vasoconstrictors or fluids, must be individualized. The clinician could consider the use of mechanical circulatory support in cases where hemodynamic optimization fails to provide sufficient support to the circulation.
Early coronary angiography in out-of-hospital cardiac arrest (OHCA) patients without ST segment elevation is safe and reasonable (2), as some patients could benefit from potential reduction in myocardial damage and a decrease in the incidence of systolic heart failure.
Pulmonary statements focus on protective lung ventilation, based on target tidal volume and PEEP. The aim is to avoid acute respiratory distress syndrome (ARDS), which leads to worse outcomes in patients after cardiac arrest (3).
Another important issue is the harm caused by hypoxemia and hyperoxia, which are well known for the risk of developing either hypoxic-ischemic brain lesions or post-ischemic oxidative lesions. Oxygen titration, which is only possible when arterial saturation is available, should be set to a target between 92 and 96% (4).
Carbon dioxide regulates blood vessel tone and cerebral blood flow and has long been the subject of research to find its appropriate threshold. The CCC study (5) found that mild hypercapnia compared to normocapnia resulted in lower values of neuron-specific enolase. However, the TAME trial (6) found that mild hypercapnia did not improve neurological outcomes at six months compared to normocapnia, in coma patients resuscitated after OHCA. These results suggest that our knowledge of the physiological interaction between oxygen, carbon dioxide and critical organs is incomplete and led to the statement to aim for a normal PaCO2 after cardiac arrest.
A characteristic of the document is that it covers all areas of patient care. Thus, there are recommendations for issues not usually addressed.
Hematological statements include the recommendation to maintain hemoglobin target over 7 g/dL in general patients and 9 g/dL in patients with coronary artery disease. Antithrombotic prophylaxis should be started within 48 hours if there are no contraindications.
Various statements are made about the systems that regulate the metabolic, digestive and endocrine systems. Enteral nutrition should be started as soon as possible, even at reduced dosage in patients with intolerance. Parenteral nutrition should be reserved for patients with enteral nutrition contraindications that persist for 5-7 days.
.
Corticosteroids should not be administered routinely, but only in the presence of suspected or diagnosed adrenal suppression. It is also recommended to consider regulating blood glucose in the range of 80-180 mg/dL.
The document also emphasizes organizational and ethical aspects. Healthcare organizations are advised to implement protocols to provide appropriate treatment in specialized centers, to encourage a multidisciplinary approach (team-based) and to provide patient and family centered care. Family members or, in a broader perspective, decision-makers are particularly important in this context where the subject often cannot make autonomous decisions. They must play an active role in patient care and be involved in the clinician's discussion of goals of care. This motivates clinicians to improve their practice and to consider additional case-specific training to develop key competencies and address individual biases.
The paper deals extensively with all areas of post-cardiac arrest management but we noted two topics that were purposely left out of the statements: target temperature management and cerebral edema.
The debate about hypothermic treatment is still unresolved. For years, this treatment was regarded as an effective method to improve neurological outcomes after cardiac arrest, but since the results of the TTM study (7) were published, this belief has been questioned.
This topic has become so relevant that some scientific societies have decided to issue specific guidelines to include the evidence present to date (8) and the scientific updates emerging from the literature. The authors decided to refer to other guidelines rather than covering the topic partially, an approach we support.
The issue of cerebral edema, on the other hand, was kept open for future guidance. The authors address the topic of intracranial pressure management, which can be considered a surrogate argument, but there are no statements on the management of cerebral edema. Unlike temperature management, there are no other works that address this argument properly. The recent “Guidelines for the Acute Treatment of Cerebral Edema in Neurocritical Care Patients” discuss the general management of this condition extensively, but do not consider the specific subset of patients after cardiac arrest (9).
This document is undoubtedly an important guide for and a basis for future developments.
Hirsch and colleagues (1) emphasized the concept of individualized care based on the differences between individual patients; physiology and balance should ultimately guide the clinicians' practice.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: G.M., A.M., and I.T..equally contributed to the manuscript preparation and fulfilled authorship criteria
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: Authors declare that they did not use AI-assisted technologies in preparation of this manuscript
References
| 1. Hirsch KG, Abella BS, Amorim E, Bader MK, Barletta JF, Berg K et al. for American Heart Association and Neurocritical Care Society. Critical care management of patients after cardiac arrest: A scientific statement from the American Heart Association and Neurocritical Care Society. Circulation 2024; 149: e168-e200. https://doi.org/10.1161/CIR.0000000000001163 PMid:38014539 PMCid:PMC10775969 |
||||
| doi: 10.1161/CIR.0000000000001163 https://doi.org/10.1161/CIR.0000000000001163 PMid:38014539 PMCid:PMC10775969 |
||||
| 2.Wyckoff MH, Singletary EM, Soar J, Olasveengen TM, Greif R, Liley HG et al. International consensus on cardiopulmonary resuscitation and emergency cardio- vascular care science with treatment recommendations: summary from the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the COVID-19 Working Group. Circulation 2022; 145: e645-e721. https://doi.org/10.1161/CIR.0000000000001050 |
||||
| doi: 10.1161/CIR.0000000000001017 https://doi.org/10.1161/CIR.0000000000001017 PMid:34813356 |
||||
| 3. Johnson NJ, Caldwell E, Carlbom DJ, Gaieski DF, Prekker ME, Rea TD et al The acute respiratory distress syndrome after out-of-hospital cardiac arrest: Incidence, risk factors, and outcomes. Resuscitation 2019; 135: 37-44. https://doi.org/10.1016/j.resuscitation.2019.01.009 PMid:30654012 |
||||
| doi: 10.1016/j.resuscitation.2019.01.009 https://doi.org/10.1016/j.resuscitation.2019.01.009 PMid:30654012 |
||||
| 4. Holmberg MJ, Nicholson T, Nolan JP, Schexnayder S, Reynolds J, Nation K et al Oxygenation and ventilation targets after cardiac arrest: a systematic review and meta-analysis. Resuscitation 2020; 152: 107-15. https://doi.org/10.1016/j.resuscitation.2020.04.031 PMid:32389599 |
||||
| Doi: 10.1016/j.resuscitation.2020.04.031 https://doi.org/10.1016/j.resuscitation.2020.04.031 PMid:32389599 |
||||
| 5. Eastwood GM, Schneider AG, Suzuki S, Peck L, Young H, Tanaka A, et al. Targeted therapeutic mild hypercapnia after cardiac arrest: a phase II multi-centre randomised controlled trial (the CCC trial). Resuscitation 2016; 104: 83-90. Doi: 10.1016/j.resuscitation.2016.03.023 https://doi.org/10.1016/j.resuscitation.2016.03.023 PMid:27060535 |
||||
| 6. Eastwood G, Nichol AD, Hodgson C, Parke RL, McGuinness S, Nielsen N, et al. Mild Hypercapnia or Normocapnia after out-of-hospital Cardiac Arrest. N Engl J Med 2023; 389: 45-57. Doi: 10.1056/nejmoa2214552 https://doi.org/10.1056/NEJMoa2214552 PMid:37318140 |
||||
| 7. Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med 2013; 369: 2197-206. doi: 10.1056/nejmoa1310519 https://doi.org/10.1056/NEJMoa1310519 PMid:24237006 |
||||
| 8. Nolan JP, Sandroni C, Andersen LW, Böttiger BW, Cariou A, Cronberg T, et al. ERC-ESICM guidelines on temperature control after cardiac arrest in adults. Resuscitation 2022; 172: 229-36. doi :10.1016/j.resuscitation.2022.01.009 https://doi.org/10.1016/j.resuscitation.2022.01.009 PMid:35131119 |
||||
| 9. Cook AM, Morgan Jones G, Hawryluk GWJ, Mailloux P, McLaughlin D, Papangelou A, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care 2020; 32: 647-66. doi: 10.1007/s12028-020-00959- https://doi.org/10.1007/s12028-020-00959-7 PMid:32227294 PMCid:PMC7272487 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

