From Editor-in-Chief: Our Hirsch index, current issue, news from ESC 2024, trials and new guidelines, protection and long COVID
EDITORIALS
From Editor-in-Chief: Our Hirsch index, current issue, news from ESC 2024, trials and new guidelines, protection and long COVID
Article Summary
- DOI: 10.24969/hvt.2024.510
- Page(s): 319-322
- CARDIOVASCULAR DISEASES
- Published: 10/09/2024
- Received: 09/09/2024
- Accepted: 09/09/2024
- Views: 4304
- Downloads: 2974
- Keywords: editorial
Address for Correspondence: Gulmira KUdaiberdieva, Heart, Vessels and Transplantation
E-mail: editor@hvt-journal.com

From Editor-in-Chief: Our Hirsch index, current issue, news from ESC 2024, trials and new guidelines, protection and long COVID
Dear readers
We have important news to share – our SCOPUS Hirsch index is increased to 4 and Google scholar h5 index increased from 4 to 5 and h5 median increased from 5 to 7 (Fig. 1). This means we received more citations and we increased number of cited articles of higher quality. Our goal is to substantially improve quality, make visible our published articles and receive more citations, so we can move with inclusion in other major databases, meaning to increase the chances of our prepared evidence-based knowledge contribute to wider internal pool of knowledge and advancement of science and practical skills.
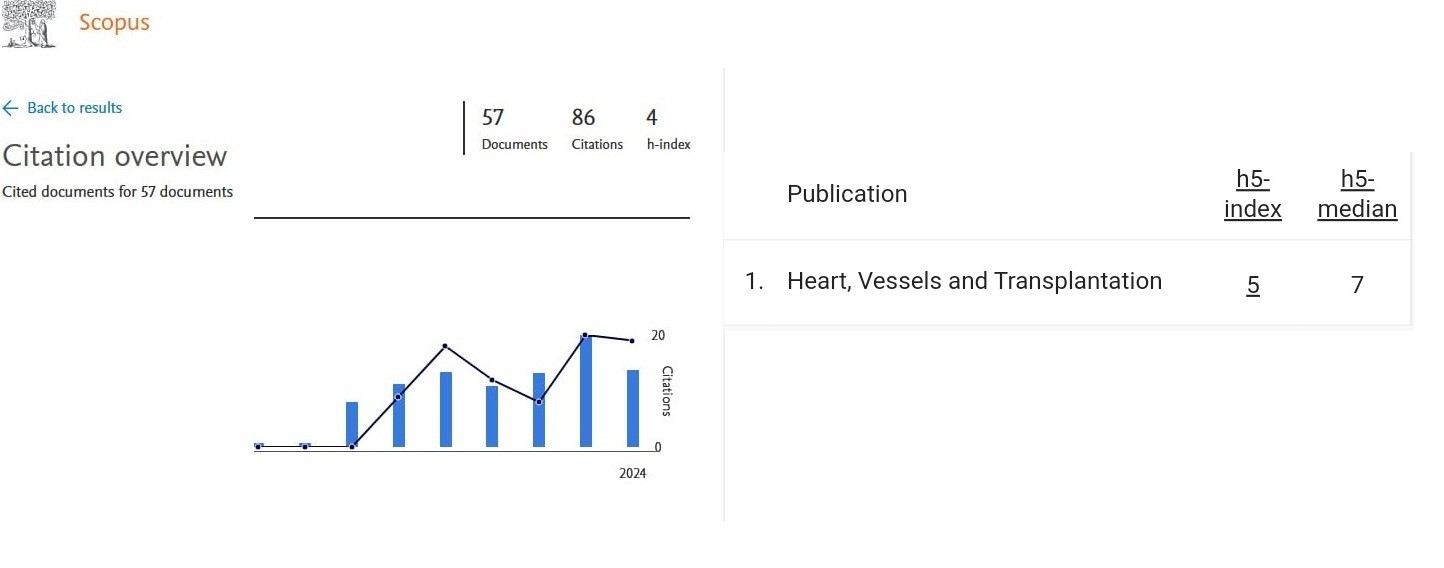
Figure 1. SCOPUS Hirsch index (left panel) and Google scholar metrics (right panel by September 2024 for Heart, Vessels and Transplantation
The novice in our published articles is that you can find now how to cite each article in the 1st page footnote under the title Citation – with authors names`, title of article , our journal abbreviation, year, volume, pages and doi number.
We would like also to remind that our authors should acknowledge the use of artificial intelligence (A.I.) in the preparation of their manuscripts, writing or generating images. We mentioned in previous Editorial that ICMJE amended the 2023 guidelines for authors making obligatory statement on use of A.I. In addition, you should submit your ORCID numbers and social media accounts as Facebook and Twitter (X) – all to increase visibility of your work in databases, libraries, internet and social media.
In our current September 2024 issue, you can find original research, review, case reports, editorial and education articles of interest to a wide reader audience. We introduce 2 important research articles on safety of environment and signage systems aimed to ease patients orientation in medical facilities; and 4 research articles related to cardiovascular (CV) surgery and interdisciplinary topics combining them with arrhythmias and rehabilitation: on outcomes of minimally invasive valvular surgery in patients with valvular heart diseases and comorbidities; predictors of postoperative atrial fibrillation (AF) after coronary bypass surgery (CABG); outcomes of diaphragmatic paralysis after pediatric cardiac surgery, and predictors of re-coarctation in patients who underwent surgery for coarctation of aorta. We also published comprehensive state-of-art review on chronic coronary artery disease (CCD) with critical analysis of current evidence and guidelines recommendation and defining directions for further research; 2 case reports on challenging case of successful implantation of pacemaker in a patient with persistent left superior vena cava syndrome and rare case of amyotrophic lateral sclerosis with frontotemporal dementia developed in a patient with obesity.
In frame of continuous medical education we prepared Editorials acquaint with recent consensus and position papers from different professional societies as ESC, AHA, ACC and their associations that might be of your interest to implement in clinical practice – our editorials provide key messages to draw you attention to main documents that may not be known by wide audience. Our published editorials are of interest for all specialties and practicing physicians: management of cardiogenic shock in elderly, critical multidisciplinary care of patients after cardiac arrest, management of infections associated with cardiac implantable electronic devices, management of fetal arrhythmias, update on stress echocardiography and the overview on how to prepare a clinical case report. Finally, you can find an article on recent international interdisciplinary school on how to prepare scientific project.
Just few days ago, the ESC 2024 live congress in London, United Kingdom has finished. After long period of pandemics, colleagues and I have opportunity to attend live event. Four important guidelines were presented (1-4): 2024 ESC guidelines on management of chronic coronary syndromes (CCS), elevated blood pressure (BP) and hypertension, management of atrial fibrillation, and peripheral arterial and aortic diseases.
These four major guidelines (1-4) will be introduced by our editors and invited experts in coming weeks and they will appear first ahead of print online and further published in December 2024 issue. Our Editors will compare also the 2024 CCS ESC and ACC/AHA CCD 2023 guidelines, 2024 ESC AF and 2023 ACC/AHA AF guidelines and 2024 ESC and 2024 AHA/ACC guidelines on aortic disease as well.
I just briefly would like to highligh major changes in elevated BP and hypertension 2024 guidelines of interest for many (4): there are no grades of BP and hypertension, rather following more simplified classification is recommended to use - non-elevated BP level (<120/70 mmHg), elevated BP level (>120/70 <140/90) and hypertension (≥140/90. The complications of hypertension are now called hypertension mediated target organ damage. There are changes in diagnostic procedures and medical treatment. Where applicable not only office but also home and ambulatory BP monitoring is recommended to measure BP. Regarding treatment the renal denervation is now suggested as class IIB for patients with resistant hypertension on combination of 3 drugs treatment. The details you can find in guideline and forthcoming Editorial.
Among HOTLINE sessions, transcatheter interventions for patients with functional mitral regurgitation and heart failure (HF) caught my interest. Patients with HF and moderate-severe mitral regurgitation have option to undergo transcatheter mitral valve repair. RESHAPE HF2 trial presented by Dr Anker (5), tested the effect of transcatheter edge-to-edge mitral valve repair (TEER) using MItra Clip device in patients with HF, ejection fraction 20%-50% and functional moderate –severe mitral regurgitation on hospitalizations, CV death and health status vs guideline recommended medical therapy. At 2 years after intervention TEER reduced composite of hospitalizations and CV death by 36% (HR - 0.64; 95% CI 0.48 to 0.85; p = 0.002) and increased health status. At the same session, MATTERHORN trial was introduced. It demonstrated noninferiority of TEER in patients with functional moderate-severe mitral regurgitation and HF to surgical mitral valve repair or left ventricular assisted device (LVAD) in terms of re-hospitalization, death, stroke, re-intervention on mitral valve or LVAD implantation (6).
It worth mentioning, that in patients undergoing transcatheter aortic valve replacement (TAVR), percutaneous coronary intervention (PCI) (7) for at least 1 lesion with FFR 0.80 resulted in reduction of MACE (death, revascularization and myocardial infarction) at 2 years by 29% (HR 0.71; 95% CI 0.51 to 0.99, p=0.04), acute kidney failure was lower by 55% (HR 0.45 (95% CI0.23–0.89), however bleeding rate was not negligible (HR 1.51; 95% CI 1.03 to 2.22) as compared with only TAVR plus conservative management group. The population median age was 82 years. PCI was recommended before TAVR, but was performed simultaneously of shortly after TAVR in 26% of patients. More studies are needed and risk of bleeding should be taken in account before procedures in urgent situations.
Again in elderly population (>75 years old, majority 70% were >80 years old) with myocardial infarction, SENIOR-RITA trial did not demonstrate benefit of invasive strategy (90% - coronary angiography, 49.9% - PCI and 3% - CABG) over conservative medical therapy in terms of composite of death and recurrent myocardial infarction (8).
Interesting study was also on role of inflammation in development of atherosclerotic disease. Large population study involved more than 27000 healthy women at age of 54 years who were followed-up for 30 years. The risk of composite outcome of myocardial infarction, revascularization, death and stroke was predicted by increased levels of C-reactive protein, LDL cholesterol and lipoprotein (a). This means, more aggressive preventive measures should target inflammation and abnormal lipid levels (9).
For HF patients with mildly reduced and preserved ejection fraction (with EF>40%) the effect of nonsteroidal mineral- corticoid receptor antagonist finerenone (10) demonstrated significant benefit in reduction of worsening of HF events and CV deaths as compared to placebo (RR 0.84; 95% CI 0.74 to 0.95; p=0.007) during 36 months of follow up as compared to placebo. It should be noted that over 85% of patients were on beta-blockers, 60% -received angiotensin converting enzyme inhibitors or angiotensin receptor blockers, angiotensin receptor and neprisylin inhibitor -8.5%, 14% sodium glucose co-transporter 2 inhibitors, loop diuretics - 87%,, thiazides -14% and glucagon-like peptide-1 receptor agonist 3%, potassium supplements – 11%.
Another trial deserving attention is SHAM-PVI study (11) that demonstrated efficacy of pulmonary vein isolation (PVI) in patients with persistent or paroxysmal AF over sham procedure (phrenic nerve denervation) in improvement of health status and reduction of AF burden. There were no crossovers between groups. This is a first trial showing efficacy of PVI over sham procedure in AF patients. Previous ones demonstrated efficacy of ablation vs placebo and antiarrhythmic therapy.
In addition, I would like to briefly mention the recently released 2024 ACC/AHA hypertrophic cardiomyopathy (HCM) guidelines (12). The major changes in management of HCM are:
-there is no age restriction for ICD therapy; for patients with more than 1 risk factor for sudden cardiac death, discussion of 5-year risk of mortality is useful in shared decision making for ICD placement;
-for patients with left ventricular outflow tract (LVOT) obstruction and persistent symptoms despite beta-blocker and dihydropiridine calcium channel blocker therapy, addition of cardiac myosin inhibitor Mavacamten (in adult patients), or dysopiramide (with atrioventricular nodal blocker) or septal reduction therapy performed at experienced centers is recommended. For patients with non-obstructive HCM and older than 45 years with likely cardiac sarcomere genetic variant and mild phenotype adding valsartan is recommended. Additionally for patients at risk for AF and on anticoagulation therapy, ambulatory monitoring is recommended for AF screening. Exercise testing is recommended in pediatric patients to define functional capacity and prognosis. This guideline will also be introduced by our invited experts.
Lastly, new updated RSV and COVID vaccines are available and approved for use in 2024-2025 season. Promote vaccination to protect your patients especially in high -risk groups with comorbidities (13). Recent studies demonstrated that COVID vaccines reduce risk of long COVID (14).
Gulmira Kudaiberdieva
Editor-in-Chief
Heart, Vessels and Transplantation
Peer-review: Internal
Conflict of interest: None to declare
Authorship: G.K.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
References
| 1.Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Developed by the task force for the management of chronic coronary syndromes of the European Society of Cardiology (ESC). Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2024; 00: 1-123. Doi: 10.1093/eurheartj/ ehae177 | ||||
| 2. McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension Developed by the task force on the management of elevated blood pressure and hypertension of the European Society of Cardiology (ESC) and endorsed by the European Society of Endocrinology (ESE) and the European Stroke Organisation (ESO). Eur Heart J 2024; 00: 1-107. Doi: 10.1093/eurheartj/ehae178 https://doi.org/10.1093/eurheartj/ehae178 PMid:39210715 |
||||
| 3. Van Gelder IC, Michiel Rienstra M, Bunting KV, Casado-Arroyo R, Caso V, Crijns HJGM, et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2024; 00: 1-101. Doi: 10.1093/eurheartj/ehae176 https://doi.org/10.1093/eurheartj/ehae176 PMid:39210723 |
||||
| 4. Mazzolai L,Teixido-Tura G, Lanzi S, Boc V, Bossone E, Brodmann M, et al.2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Developed by the task force on the management of peripheral arterial and aortic diseases of the European Society of Cardiology (ESC). Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS), the European Reference Network on Rare Multisystemic Vascular Diseases (VASCERN), and the European Society of Vascular Medicine (ESVM). Eur Heart J 2024; 00: 1-163. Doi: 10.1093/eurheartj/ehae179 https://doi.org/10.1093/eurheartj/ehae179 PMid:39210722 |
||||
| 5. Anker SD, Friede T, von Bardeleben RS, Butler J, Khan MS, Diek M, et al. for the RESHAPE-HF2 Investigators. Transcatheter valve repair in heart failure with moderate to severe mitral regurgitation. New Engl J Med 2024; DOI: 10.1056/NEJMoa2314328 https://doi.org/10.1056/NEJMoa2314328 PMid:39216092 |
||||
| 6. Baldus S, Doenst T, Pfister R, Gummert J, Kessler M, Boekstegers P, et al. for the MATTERHORN Investigators. Transcatheter repair versus mitral-valve surgery for secondary mitral regurgitation. New Engl J Med 2024; DOI: 10.1056/NEJMoa2408739 https://doi.org/10.1056/NEJMoa2408739 PMid:39216093 |
||||
| 7. Lonborg J, Jabbari R, Sabbah M, Veien KT, Niemela M, Freeman P, et al. for the NOTION-3 Study Group. PCI in patients undergoing transcatheter aortic valve implantation. New Engl J Med 2024; DOI: 10.1056/NEJMoa2401513 https://doi.org/10.1056/NEJMoa2401513 PMid:39216095 |
||||
| 8. Kunadian V, Mossop H, Shields C, Bardgett M, Watts P, Teare MD, et al. for the British Heart Foundation SENIOR-RITA Trial Team and Investigators. Invasive treatment strategy for older patients with myocardial infarction. New Engl J Med 2024; DOI: 10.1056/NEJMoa2401513 https://doi.org/10.1056/NEJMoa2401513 PMid:39216095 |
||||
| 9. Ridker PM, Moorthy MV, Cook NR, Rifai N, Lee IM, Buring JE. Inflammation, cholesterol, lipoprotein(a), and 30-year cardiovascular outcomes in women. New Engl J Med 2024; DOI: 10.1056/NEJMoa2405182 https://doi.org/10.1056/NEJMoa2405182 PMid:39216091 |
||||
| 10. Solomon SD, McMurray JJV, Vaduganathan M, Claggett B, Jhund PS, | ||||
| A.S. Desai, et al. for the FINEARTS HF investigators, Finerenone in heart failure with mildly reduced or preserved ejection fraction. New Engl J Med 2024; DOI: 10.1056/NEJMoa2407107 https://doi.org/10.1056/NEJMoa2407107 PMid:39225278 |
||||
| 11. Dulai R, Sulke R, Fremantle L, et al. Pulmonary vein isolation vs sham intervention in symptomatic atrial fibrillation. JAMA 2024; doi:10.1001/jama.2024.17921 https://doi.org/10.1001/jama.2024.17921 PMid:39221629 |
||||
| 12. Ommen SR, Ho CY, Asif IM, Balaji S, Burke MA, Day SM, et al. 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. https://doi.org/10.1161/CIR.0000000000001250 PMid:38718139 |
||||
| 2024; 83: 2324-405. | ||||
| 13. CDC. Available at: URL: https:// www.cdc.gov/covid/vaccines | ||||
| 14. CDC. Clinical overview of long COVID. Available at: URL: https:// www.cdc.gov/covid/hcp/clinical-overview/index.html | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

